Surgical Removal of Choroidal Neovascular Membranes After Laser
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Masqueraders of Age-Related Macular Degeneration
COVER STORY Masqueraders of Age-related Macular Degeneration A number of inherited retinal diseases phenocopy AMD. BY RONY GELMAN, MD, MS; AND STEPHEN H. TSANG, MD, PHD ge-related macular degeneration (AMD) is a leading cause of central visual loss among the elderly population in the developed world. The Currently, there are no published A non-neovascular form is characterized by mac- guidelines to prognosticate ular drusen and other abnormalities of the retinal pigment epithelium (RPE) such as geographic atrophy (GA) and Stargardt macular degeneration. hyperpigmented areas in the macula. The neovascular form is heralded by choroidal neovascularization (CNV), with subsequent development of disciform scarring. ABCA4 defect heterozygote carrier may be as high as This article reviews the pathologic and diagnostic char- one in 20.11,12 An estimated 600 disease-causing muta- acteristics of inherited diseases that may masquerade as tions in the ABCA4 gene exist, of which the three most AMD. The review is organized by the following patterns common mutations account for less than 10% of the of inheritance: autosomal recessive (Stargardt disease and disease phenotypes.13 cone dystrophy); autosomal dominant (cone dystrophy, The underlying pathology of disease in STGD involves adult vitelliform dystrophy, pattern dystrophy, North accumulation of lipofuscin in the RPE through a process Carolina macular dystrophy, Doyne honeycomb dystro- of disc shedding and phagocytosis.14,15 Lipofuscin is toxic phy, and Sorsby macular dystrophy); X-linked (X-linked to the RPE; furthermore, A2E, a component of lipofuscin, retinoschisis); and mitochondrial (maternally inherited causes inhibition of 11-cis retinal regeneration16 and diabetes and deafness). complement activation. -

Mcardle Disease Associated Maculopathy and the Role of Glycogen in the Retina
Marques JH and Beirão JM, J Ophthalmic Clin Res 2020, 7: 067 DOI: 10.24966/OCR-8887/100067 HSOA Journal of Ophthalmology & Clinical Research Case Report demanding tissues like the RPE depend on glycogen phosphoryla- McArdle Disease associated tion to produce energy and, on the other hand, glycogen erroneous accumulation may impair cellular functions. Probably due to higher Maculopathy and the Role of photoreceptor concentration and subsequent energy demand in the macula, this is the primary site for degeneration in our patient. The Glycogen in the Retina present report reinforces the role of the glycogen pathway as a pos- sible player in the pathophysiology of RPE pathologies, genetically and/or environmentally determined. Keywords: Age-related macular degeneration; Geographic atrophy; João Heitor Marques1* and João Melo Beirão1,2 Glycogen; McArdle; Retinal pigmented epithelium 1Serviço de Oftalmologia, Centro Hospitalar e Universitário do Porto, Portugal Introduction 2Instituto de Ciências Biomédicas Abel Salazar, Universidade do Porto, Portugal Intracellular glycogen works as a buffer for glucose metabolism. Glycogen phosphorylase breaks down glycogen, making glucose available for aerobic and anaerobic energetic pathways. It can be rapidly metabolized without ATP requirement. A deficit in glycogen phosphorylation results, not only in energy shortage, but also in its Abstract intracellular accumulation, which may further interfere with other Purpose: To report a case of maculopathy with pattern dystrophy cellular functions. and geographic atrophy in a patient with McArdle disease and to review the glycogen pathway’s disorders as a source of energy but Glycogen Storage Disease type V (GSDV), also known as McAr- also cause of disease in the retina. -

Clinical Study on Hypotony Following Blunt Ocular Trauma
陨灶贼允韵责澡贼澡葬造皂燥造熏灾燥造援 5熏晕燥援 6熏 Dec.18, 圆园12 www.IJO.cn 栽藻造押8629原愿圆圆源缘员苑圆 8629-83085628 耘皂葬蚤造押ijopress岳员远猿援糟燥皂 窑Monograph窑 ClinicalstudyonHypotonyfollowingbluntocular trauma DepartmentofOphthalmology, theSecondXiangya INTRODUCTION HospitalofCentralSouthUniversityandInstitutionof ypotonyfollowingbluntoculartraumaisasevere OphthalmicCenter,Changsha410011,HunanProvince, H complicationwhoseexactpathogenesisisnotclear. China Ocular hypotension canbeassociatedwithseveral Correspondenceto: JunZeng.DepartmentofOphthalmo- complications suchasmacularedema,discedema, logy,theSecondXiangyaHospitalof CentralSouth hypotonymaculopathy,cornealedema,shallowanterior UniversityandInstitutionofOphthalmicCenter,139# chamber,choroidaleffusionorhemorrhage,exudative RenminMiddleRoad,Changsha410011,HunanProvince, retinaldetachment,orcataractformation,ultimatelyleading [email protected] tophthisisbulbi [1-3].Anyofthesecomplicationscanbe Received:2012-04-15 Accepted:2012-11-01 associatedwithvisualsymptomsorareductioninvisual acuity.Thereisrelativelylessdataontheriskfactorsfor Abstract hypotonyafterbluntoculartrauma.Sothisarticlebriefly · AIM:Toevaluatetheincidenceandriskfactorsof discussestheriskfactorsofhypotonyfollowingbluntocular hypotonyinpatientswithbluntoculartrauma. trauma. MATERIALSANDMETHODS ·METHODS:Themedicalrecordsof145patientswithblunt StudyDesign Thiswasaretrospectivestudyofpatients oculartraumawerereviewed.Hypotonywasdefinedasan seenintheophthalmologydepartmentattheSecond averageintraocularpressure(IOP)of5mmHgorlessfor threetimes. XiangyaHospital'semergencyserviceovertwoandahalf -

A Clinical Study of Prevalence of Dry Eyes in Diabetes and Diabetic Retinopathy
International Journal of General Medicine and Pharmacy (IJGMP) ISSN(P): 2319-3999; ISSN(E): 2319-4006 Vol. 3, Issue 2, Mar 2014, 31-36 © IASET A CLINICAL STUDY OF PREVALENCE OF DRY EYES IN DIABETES AND DIABETIC RETINOPATHY MURTUZA JHABUAWALA1 & A. P. AGASHE2 1Fellow in Phacoemulsifation and Refractive Surgery, Narayan Nethralaya, Bangalore, Karnataka, India 2Professor, MGM Medical College & Hospital, Navi Mumbai, Maharashtra, India ABSTRACT Introduction: Diabetes mellitus is associated with a number of ocular complications which can even lead to blindness. Recently, problems involving the ocular surface, dryness in particular, have been reported in diabetic patients. These patients suffer from a variety of corneal complications, including superficial punctate keratopathy, corneal ulceration, and persistent epithelial defects. In addition, many diabetic patients complain of typical dry eye symptoms, such as burning and/or foreign body sensation, indicating a clear role of tear film abnormalities. Materials and Methods: A cross sectional study was conducted on 100 diabetic patients who came to the department of Ophthalmology, MGM Hospital, Mumbai. These patients were examined to study the prevalence of dry eyes in patients with diabetes and diabetic retinopathy. Results: The prevalence of dry eyes in diabetics was 14% with significant association with male gender. The prevalence of Retinopathy among diabetes patients was 18%. Around 55% patients of retinopathy patients suffer from dry eyes, the association was found to be statistically significant. -

R·Fermces Pres�Ure, Which Fluctuated Between 40 and 00 Mrnhg
Sir, Primary surgical management in a case of subtotal iridodialysis Iridodialysis is the separation of the iris bast' from the ciliary body and the scleral spm. The iris root is the thinnest and weakest part of iris anatomy, making it 1 \'Ulnerable to ocular trauma. \\'(, desnibe a case where traumatic iridodialysis was sustaim'd resulting in secondary glaucoma. Surgical interwntion invoh'ing an anterior chamber washout and removal of necrotic iris brought about control of the intraocular pressure. Case' rt?l'Mt A 66-year-old man susteHned blw)t trauma to his right eye whilst repairing his garage door. Visual al"uity in this eye WclS hand movements. On slit-lamp examinati('O an iridodialy!'is of 3300 W,)S pr('sC'nt, as was a microscopic hyphaema (Fig. 1). There was a vitreous haemorrhage, with no fundal view. The lens was subluxed postt'riorly and cataractous. ThE-' iris appeared to be ne':l'lltic 111ere Fig. I, C(l/ollr l'ilvt"grtll'iI <holL'l1IS �lIbt(}tal md(}dillly�is. was zonular d('hi�cenct' exCt'pt inferiorly \'Ilhen' the iris 4 :; was stll! attached. The intraocular pressure was 40 taUooing. , In cast's wht're a cataract has developed and e oc mmHg. An ultrasound scan showed a f1clt rC'tinel. '1 he thE.' l ns zonule is stablC', rrostC'd intra ular ll'nses have patient was treated with topical steroids emd beta been implanted v.ath �uccess." blockers, togl'ther with systemic aceta/.olamidl' emd mannitol. None of this served to rt'duce the intraocular R·fermces pres�ure, which fluctuated between 40 and 00 mrnHg. -

Two Cases of Torpedo Maculopathy with OCT Scans, One Demonstrating a Unique Deep Pit with Visible Bare Sclera
Two Cases of Torpedo Maculopathy with OCT scans, one demonstrating a unique deep pit with visible bare sclera. Isadora Ritter, OD; Sarah Brehm, OD; Susan S. Schuettenberg, OD, FAAO Abstract: This case discussion presents two cases of torpedo maculopathy not previously diagnosed. One patient displays significant tissue disruption overlying the lesion, indicating possibility of full-thickness loss to neurosensory retina accompanying this rare retinal pathology. Case Report: A 27 year old white male visited the University Eye Care clinic complaining of longstanding blur in his right eye at both distance and near. He had a history of longstanding poor vision OD for “as long as he could remember,” and had been diagnosed with amblyopia as a child. He had been patched OD at the age of 5 for a period of about one year, although he noticed no change in vision after patching. He had no history of ocular surgery and no history of ocular trauma, although after questioning he mentioned a car accident in childhood. He could not recall any injury to eye, orbit or adnexa during the accident or at any other time. Family history was significant only for glaucoma (late onset, via his maternal grandmother). He suffered from occasional outbreaks of facial acne for which he was taking oral amoxicillin. Best corrected visual acuities were: OD 20/50+2 , OS 20/20. Extraocular motilities were full, pupils were equal, round, and reactive to light with no APD, and confrontation visual fields were full to finger counting in both right and left eyes. Cover tests revealed no tropia at distance or near (near cover test revealed mild exophoria). -

Methylmalonic Aciduria and Homocystinuria-Associated Are Similar As Well
Correspondence 1731 exists about its metabolism and effects on development.3 Case report Given the rarity of its use in children, performing a A 2-year-old boy was reported to develop nystagmus at 5 randomised control trial is unrealistic, but an alternative months of age. He was born without complication at 40 method would be to establish a central database that weeks gestation and weighed 6 pounds 11 ounces at allows clinicians who use anti-vascular endothelial birth. At the age of 1 month, he was evaluated for failure growth factor therapy in children to report results and to thrive and found to have elevated urine levels of complications. methylmalonic acid and homocysteine, and was diagnosed with methylmalonic aciduria and Conflict of interest homocystinuria. He has since received regular The authors declare no conflict of interest. intramuscular injections of hydroxycobalamin and betaine, and been maintained on a special diet. Ophthalmic examination revealed the ability to fix and follow objects, and the presence of horizontal References jerk nystagmus. Fundoscopic examination showed well-circumscribed, round, and relatively flat yellow 1 Brown DM, Kaiser PK, Michels M, Soubrane G, Heier JS, lesions in both maculae, which were vitelliform in Kim RY et al. Ranibizumab versus verteporfin for neovascular appearance. The lesion in the right eye appeared to be age-related macular degeneration. N Engl J Med 2006; 355: larger than the one in the left eye, which was ring-like, 1432–1444. suggesting an early stage of development (Figure 1). 2 Rosenfeld PJ, Brown DM, Heier JS, Boyer DS, Kaiser PK, Fluorescein angiography was performed under Chung CY et al. -
Eye Conditions-DBQ
INTERNAL AFFAIRS VETERANS USE EYE CONDITIONS DISABILITY BENEFITS QUESTIONNAIRE IMPORTANT - THE DEPARTMENT OF VETERANS AFFAIRS (VA) WILL NOT PAY OR REIMBURSE ANY EXPENSES OR COST INCURRED IN THE PROCESS OF COMPLETING AND/OR SUBMITTING THIS FORM. PLEASE READ THE PRIVACY ACT AND RESPONDENT BURDEN INFORMATION ON REVERSE BEFORE COMPLETING FORM. NAME OF PATIENT/VETERAN PATIENT/VETERAN'S SOCIAL SECURITY NUMBER NOTE: This examination must be conducted by a licensed ophthalmologist or by a licensed optometrist. The examiner must identify the disease, injury or other pathologic process responsible for any decrease in visual acuity or other visual impairment found. Examinations of visual fields or muscle function should be conducted ONLY when there is a medical indication of disease or injury that may be associated with visual field defect or impaired muscle function. If indicated to address requested claim, and not medically contraindicated, dilated fundus exam required. IS THIS DBQ BEING COMPLETED IN CONJUNCTION WITH A VA21-2507, C&P EXAMINATION REQUEST? YES NO If "No," how was the examination completed (check all that apply)? In-person examination Records reviewed Other, please specify: Comments: ACCEPTABLE CLINICAL EVIDENCE (ACE) INDICATE METHOD USED TO OBTAIN MEDICAL INFORMATION TO COMPLETE THIS DOCUMENT: Review of available records (without in-person or video telehealth examination) using the Acceptable Clinical Evidence (ACE) process because the existing medical evidence provided sufficient information on which to prepare the DBQ and such an examination will likely provide no additional relevant evidence. Review of available records in conjunction with a telephone interview with the Veteran (without in-person or telehealth examination) using the ACE process because the existing medical evidence supplemented with a telephone interview provided sufficient information on which to prepare the DBQ and such an examination would likely provide no additional relevant evidence. -

Paracentral Acute Middle Maculopathy a New Variant of Acute Macular Neuroretinopathy Associated with Retinal Capillary Ischemia
Research Original Investigation | CLINICAL SCIENCES Paracentral Acute Middle Maculopathy A New Variant of Acute Macular Neuroretinopathy Associated With Retinal Capillary Ischemia David Sarraf, MD; Ehsan Rahimy, MD; Amani A. Fawzi, MD; Elliott Sohn, MD; Irene Barbazetto, MD; David N. Zacks, MD, PhD; Robert A. Mittra, MD; James M. Klancnik Jr, MD; Sarah Mrejen, MD; Naomi R. Goldberg, MD, PhD; Robert Beardsley, MD; John A. Sorenson, MD; K. Bailey Freund, MD IMPORTANCE With the advent of more sophisticated imaging systems, such as spectral domain optical coherence tomography (SD-OCT), disruption of the inner segment/outer segment (IS/OS) band, and thinning of the outer nuclear layer (ONL) have been identified in association with acute macular neuroretinopathy (AMN). OBJECTIVES To characterize a new SD-OCT presentation of AMN as a paracentral acute middle maculopathy and to describe multimodal imaging findings that implicate an underlying pathogenesis related to retinal capillary ischemia. DESIGN, SETTING, AND PARTICIPANTS Retrospective observational case series (January 1, 2012, to January 1, 2013) reviewing clinical and imaging data from 9 patients (11 eyes) with AMN at 6 tertiary referral centers. Lesions were classified as type 1 or 2 in relation to the SD-OCT location of the lesion above (type 1) or below (type 2) the outer plexiform layer (OPL) at 6 tertiary referral centers. RESULTS Of the 9 patients, 5 were female and 4 were male (mean age, 47.6 years; range, 21-65 years). All patients presented with an acute paracentral scotoma and demonstrated a classic dark gray paracentral lesion with near-infrared imaging. Visual acuity ranged from 20/15 to 20/30. -
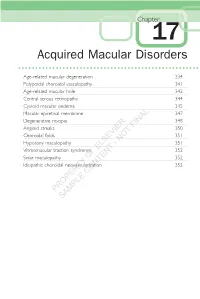
Acquired Macular Disorders
Chapter 17 Acquired Macular Disorders Age-related macular degeneration 334 Polypoidal choroidal vasculopathy 341 Age-related macular hole 342 Central serous retinopathy 344 Cystoid macular oedema 345 Macular epiretinal membrane 347 Degenerative myopia 348 Angioid streaks FINAL 350 Choroidal folds 351 NOT Hypotony maculopathy - 351 Vitreomacular traction syndrome ELSEVIER 352 Solar maculopathy OF 352 Idiopathic choroidal neovascularization 352 CONTENT PROPERTY SAMPLE 334 Acquired Macular Disorders Age-related macular degeneration Drusen 1. Histopathology (Fig. 17.1) • Discrete deposits of the abnormal material located between the basal lamina of the RPE and the inner collagenous layer of Bruch membrane. • Thickening of Bruch membrane Fig. 17.2 Hard drusen compounded by excessive production of basement mem- brane deposit by the RPE. a FINAL Atrophy and depigmentation NOT - RPE ELSEVIER OF Bruch membrane Drusen Thickening CONTENTb Fig. 17.1 Histopathology of drusen 2. Signs – yellow sub-RPEPROPERTY excrescences distributed symmetricallySAMPLE at both posterior poles. a. Small hard drusen – less than half a vein width in diameter with discrete margins (Fig. 17.2). b. Large soft drusen – vein width or more in diameter with indistinct margins (Fig. 17.3a). Fig. 17.3 (a) Soft drusen; (b) FA c. Calcifi ed drusen – may be hard or soft (Fig. 17.4). Age-related macular degeneration 335 a Fig. 17.4 Calcifi ed drusen b 3. FA a. Hyperfl uorescence – window defect due to atrophy of the overlying RPE and late staining (see FINAL Fig. 17.3b). b. Hypofl uorescence – of hydrophobic NOT (high lipid content) drusen. - 4. Drusen and AMD – features ELSEVIER associated with an increased risk of subsequent visual loss include largeOF soft and/or confl uent drusen, and Fig. -
A Case of Self-Documented Paracentral Acute Middle Maculopathy After Cataract Surgery 27
A Case of Self-Documented Paracentral Acute Middle Maculopathy After Cataract Surgery 27 CASE REPORT Timothy J Bennett Correspondence to: Justin D Etzel Timothy J Bennett, CRA, OCT-C, FOPS Sarah R Weber Department of Ophthalmology Jeffrey M Sundstrom The Pennsylvania State University College of Medicine 500 University Drive HU19 Hershey PA, 17033 717/531-5516 [email protected] A Case of Self-Documented Paracentral Acute Middle Maculopathy After Cataract Surgery Abstract diagnosis. This report describes a case of paracentral acute Background: This report illustrates a case of paracen- middle maculopathy (PAMM) occurring within hours of uncomplicated cataract surgery. This case is unique in that tral acute middle maculopathy (PAMM) following rou- it affected an experienced ophthalmic photographer who tine cataract surgery. This case provides unique insight self-documented his condition with infrared reflectance into the development and progression of the condition (IR) and spectral-domain optical coherence tomography through extensive serial ophthalmic imaging. (SD-OCT) images prior to surgery as well as numerous Case presentation: Several hours after cataract sur- serial images following surgery. gery of his left eye, a 57-year-old ophthalmic photog- It is not uncommon for ophthalmic photographers to rapher presented to the clinic with a left paracentral image their own eyes as a test subject when trying new scotoma. Serial infrared reflectance (IR) and spectral equipment, demonstrating techniques, or troubleshoot- domain optical coherence tomography (SD-OCT) ing technical issues. In this case, baseline images had images were obtained prior to, immediately following, been self-captured while demonstrating the capabilities and 10 days after the initial event. -

Identifying Characteristic Features of the Retinal and Choroidal Vasculature in Choroideremia
1 Identifying characteristic features of the retinal and choroidal vasculature in Choroideremia 2 using optical coherence tomography angiography 3 Running head: Choroideremia and OCTA 4 Alessandro Abbouda MD1-2, Adam M Dubis PhD1-2, Andrew R Webster1-2 MD FRCOpth, 5 Mariya Moosajee1-2 PhD FRCOpth 6 1 UCL Institute of Ophthalmology, 11-43 Bath Street, London EC1V 9EL 7 2 Moorfields Eye Hospital NHS Foundation Trust, 162 City Road, London EC1V 2PD 8 Financial Support: National Institute of Health Research (NIHR), Choroideremia Research Inc, USA 9 Foundation 10 Conflict of Interest: No conflicting relationship exists for any author 11 Corresponding Author: 12 Dr. Mariya Moosajee 13 UCL Institute of Ophthalmology, 14 11-43 Bath Street, 15 London, UK, EC1V 9EL 16 Email: [email protected] 1 17 Abstract 18 Aims: Using optical coherence tomography angiography (OCTA) to investigate the area with 19 flow in the superficial retinal vessel network (SVRN) and choriocapillaris (CC) layer 20 amongst male subjects with Choroideremia (CHM), female carriers and normal controls to 21 identify vascular changes. 22 Methods: Images of SRVN and CC layer were acquired in 9 affected males, 5 female 23 carriers and 14 age- and gender-matched controls using the Angiovue software of the RTVue 24 XR Avanti (Optovue, Inc., Fremont, CA). 25 Results: The mean age was 33 years for affected male CHM patients (median 30 years), 46 26 years for female carriers (median 53 years) and 39 years for controls (median 38.5). Mean 27 SRVN area ± SD in subjects with CHM was 12.93±2.06 mm2 in carrier subjects, 15.36±0.60 28 mm2 and in controls 15.30±1.35 mm2 (p<0.01).