Spinal Motion Restriction in the Trauma Patient
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Multi-County Ambulance Inspection Basic Life Support Checklist
Multi-County Ambulance Inspection Basic Life Support Checklist Company Name: ___________________________________________ Date: _____________________ Sticker Number: __________ Old Sticker Number: _________ Based in the following counties: Adams Arapahoe Broomfield Douglas Elbert Jefferson Unit No.: _______ VIN: __________________________________________Lic #: ___________________ Exp. Date: _________ Ambulance Make: _____________________ Manufacturer: ________________________ Year: ________ Odometer: _________ Insurance Company: ______________________________ Policy No.: _____________________________ Exp. Date: _________ __Basic Life Support __Basic Life Support with Advanced Life Support Capabilities __Advanced Life Support (BLS) (BLS/ALS) (ALS) __ Reserve Vehicle (Will be fully stocked according to this Inspection list before going into service.) Basic Life Support Check List Emergency Systems: __ AED-Automatic External Defibrillator Serial No ________ __ Ambulance Service Medical Treatment __Adult Pads __Pediatric Pads Protocols (Current) __Computerized __Printed Passed Self-Test Date: _____________ Time:___________ __ Running Lights __ Emergency Lights __Siren __Opticom Dressings and Bandages: __Wipers __ ABD Pads __ Communications appropriate for jurisdiction served. __ Bandages, roller type, self-adhesive __cell phone __ Portable Radio __ Multi Trauma Dressing (10 x 36) __ Dispatched by: _________________________ __ Sterile Burn Sheets __ A set of 3 warning reflectors or devices. __ Occlusive Dressing ______________________________________ -

Lights and Siren Use by Emergency Medical Services (EMS): Above All Do No Harm
U. S. Department of Transportation National Highway Traffic Safety Administration Office of Emergency Medical Services (EMS) Lights and Siren Use by Emergency Medical Services (EMS): Above All Do No Harm Author: Douglas F. Kupas, MD, EMT-P, FAEMS, FACEP Submitted by Maryn Consulting, Inc. For NHTSA Contract DTNH22-14-F-00579 About the Author Dr. Douglas Kupas is an EMS physician and emergency physician, practicing at a tertiary care medical center that is a Level I adult trauma center and Level II pediatric trauma center. He has been an EMS provider for over 35 years, providing medical care as a paramedic with both volunteer and paid third service EMS agencies. His career academic interests include EMS patient and provider safety, emergency airway management, and cardiac arrest care. He is active with the National Association of EMS Physicians (former chair of Rural EMS, Standards and Practice, and Mobile Integrated Healthcare committees) and with the National Association of State EMS Officials (former chair of the Medical Directors Council). He is a professor of emergency medicine and is the Commonwealth EMS Medical Director for the Pennsylvania Department of Health. Disclosures The author has no financial conflict of interest with any company or organization related to the topics within this report. The author serves as an unpaid member of the Institutional Research Review Committee of the International Academy of Emergency Dispatch, Salt Lake City, UT. The author is employed as an emergency physician and EMS physician by Geisinger Health System, Danville, PA. The author is employed part-time as the Commonwealth EMS Medical Director by the Pennsylvania Department of Health, Bureau of EMS, Harrisburg, PA. -

Spinal Motion Restriction Feasibility Study (SMRFS)
CONFIDENTIAL: Spinal Motion Restriction Feasibility Study (SMRFS). Spinal Motion Restriction Feasibility Study SMRF Study Protocol Version 1.1 IRAS ID: 253128 SMRF Study protocol v 1.1 24/01/20 Page 1 of 57 CONFIDENTIAL: Spinal Motion Restriction Feasibility Study (SMRFS). CONTACT NAMES AND NUMBERS Sponsor: Michelle Jackson, Research and Development Manager, North East Ambulance Service NHS Foundation Trust, Bernicia House, Goldcrest Way, Newburn Riverside, Newcastle Upon Tyne. NE15 8NY Tel: 01914302000 Email: [email protected] Chief Investigators: Lee Thompson, Trauma Team, North East Ambulance Service NHS Foundation Trust, Bernicia House, Goldcrest Way, Newburn Riverside, Newcastle Upon Tyne. NE15 8NY Tel: 01914302399 Email: [email protected] Investigators Group: Dr. Charlotte Bates, Northumbria Specialist Emergency Care Hospital, Email: [email protected] Dr. Christopher Hawkins. Sunderland Royal Hospital. Email: [email protected] Lt Col. Paul Hunt, James Cook University Hospital Email: [email protected] Gary Shaw, North East Ambulance Service. Email: [email protected] Study Steering/Monitoring: Dr Alasdair Corfield. NHS Greater Glasgow and Clyde. Dr Peter McMeekin. Northumbria University. Michelle Jackson. North East Ambulance Service Research and Development. Lee Thompson. North East Ambulance Service. Gary Shaw. North East Ambulance Service. Dr. Charlotte Bates. Northumbria Specialist Emergency Care Hospital. Shane Woodhouse. North East Ambulance Service Clinical Audit. Gary Shaw. North East Ambulance Service. Dan Haworth. North East Ambulance Service. Study Co-ordination Centre: North East Ambulance Service NHS Foundation Trust, Bernicia House, Goldcrest Way, Newburn Riverside, Newcastle Upon Tyne. NE15 8NY IRAS ID: 253128 SMRF Study protocol v 1.1 24/01/20 Page 2 of 57 CONFIDENTIAL: Spinal Motion Restriction Feasibility Study (SMRFS). -

Required ALS and BLS Equipment and Supplies
S T A T E O F H A W A I I D E P A R T M E N T O F H E A L T H ESSENTIAL EQUIPMENT and SUPPLIES FOR BASIC and ADVANCED LIFE SUPPORT Ambulance Service Standards Revised 10-14-10 ESSENTIAL EQUIPMENT FOR BASIC LIFE SUPPORT Ambulance cot w/ 3 seatbelts Sheets, linen or disp., 4 ea Cot fasteners, Floor/Wall Mount Blankets, non-synthetic, 4 ea Portable oxygen unit 360L min. tank Gauze pads, sterile, 3x3 min, 24 ea Flowmeter 0-15L/min Gauze rolls, sterile, 2" x 5 yds, 4 ea Positive pressure elder-type valve Gauze rolls, sterile 3"/4" x 5 yds, 4 ea Oxygen masks, clear, disposable, adult/pedi 1 ea Gauze rolls, sterile, 6" x 5 yds, 4 ea Oxygen nasal cannula, disposable 2 ea Triangle bandage, 40" min, 3 ea Oropharyngeal airways, adult/ped/infant 1 ea Universal dressing, 8 x 10 min, sterile, 1 ea Nasopharyngeal airways, 2 ea Tape, 1" and 2" x 5 yds, 1 ea Oxygen tanks, spare, 360L min, 2 ea Bandaids, assorted Bag-valve-mask, pedi w/02 reservoir Plastic wrap, 12" x' 12" min, 1 ea Bag-valve-mask, adult w/02 reservoir Burn sheets, sterile, 2 ea Suction, portable, battery operated Sphygmomanometer, adult, 1 ea Widebore tubing Extra large adult, 1 ea Rigid pharyngeal suction tip Pediatric, 1 ea Suction catheters 5, 10, 14, 18fr, 1 ea Stethescope, 1 ea Bite sticks (mouth gag), 2 ea Scissors, bandage, 5" min Ammonia inhalants, 3 ea Thermometer, oral and rectal, 1 ea Antiseptic swabs, 50 ea Spineboard, short, w/straps, 1 ea Bulb syringe, 3 oz. -

Guide for Developing an EMS Agency Safety Program
National EMS SAFETY COUNCIL Guide for Developing an EMS Agency Safety Program A roadmap for EMS agencies to develop and implement a comprehensive workplace safety program, customizable to their agency type, size and needs. Introduction to the EMS Safety Program Guide National EMS Safety In 2013, the National EMS Culture of Safety Strategy was published. Funded by Council Mission the National Highway Traffic Safety Administration (NHTSA), the initiative brought Statement together the EMS stakeholder community to identify what constitutes a safe environment for EMS patients and practitioners; barriers to achieving a safe EMS • Develop practical environment; and a strategy to overcome these challenges. ways to implement the recommendations The strategy envisioned the establishment of a national level organization to included in National coordinate national EMS safety efforts and serve as a repository for information, EMS Culture of Safety data and resources. In 2015, leading national EMS and safety organizations came Strategy. together to form the National EMS Safety Council. The goals of the council are to: • Review the latest information, research • Ensure that patients receive emergency and mobile healthcare with the highest and best practices standards of safety. on EMS patient and • Promote a safe and healthy work environment for all emergency and mobile practitioner safety. healthcare practitioners. • Develop and publish consensus statements This Guide for Developing an EMS Agency Safety Program is an initiative of the on the issues of EMS National EMS Safety Council. Its members saw the need to provide tools and patient and practitioner resources that EMS agencies could use to put the concepts outlined in the Culture safety. -

Accepted Manuscript
Accepted Manuscript The definite risks and questionable benefits of liberal pre-hospital spinal immobilisation Thomas Adam Purvis, Brian Carlin, Peter Driscoll PII: S0735-6757(17)30063-3 DOI: doi: 10.1016/j.ajem.2017.01.045 Reference: YAJEM 56444 To appear in: Received date: 14 October 2016 Revised date: 3 January 2017 Accepted date: 23 January 2017 Please cite this article as: Thomas Adam Purvis, Brian Carlin, Peter Driscoll , The definite risks and questionable benefits of liberal pre-hospital spinal immobilisation. The address for the corresponding author was captured as affiliation for all authors. Please check if appropriate. Yajem(2017), doi: 10.1016/j.ajem.2017.01.045 This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain. ACCEPTED MANUSCRIPT MANUSCRIPT TITLE PAGE TITLE: The Definite Risks and Questionable Benefits of Liberal Pre-Hospital Spinal Immobilization. CORRESPONDING AUTHOR DETAILS Full name: Mr Thomas Adam Purvis Postal address: 23 Lyndhurst Gardens, Belfast, BT13 3PH email: [email protected] Telephone number: +447887563863 CO-AUTHOR DETAILS Full name: Mr Brian Carlin Department: Pre-hospital Care Institution: Royal -

Need to Create a Head and Spinal Immobilzation Procedure
Michigan General Procedures SPINAL PRECAUTIONS Date: July 18, 2014 Page 1 of 3 Spinal Precautions Pre-Medical Control MFR/EMT/SPECIALIST/PARAMEDIC Indications & General Guidance 1. Refer to the Spinal Injury Assessment Protocol. Patients with a positive spinal injury assessment should have spinal precautions maintained during transport. 2. Major trauma patients who require extrication should have spinal precautions maintained using an extrication device (long backboard or equivalent) during extrication. If sufficient personnel are present, the patient may be log rolled from the extrication device to the ambulance cot during loading of the patient. 3. Patients may remain on the extrication device if the crew deems it safer for the patient considering stability, time and patient comfort considerations. This decision will be at the discretion of the crew. 4. Patients with penetrating traumatic injuries do not require spinal precautions unless a focal neurologic deficit is noted on the spinal injury assessment. 5. An ambulatory patient with a positive spinal injury assessment should have an appropriately sized cervical collar placed. Place the patient directly on the ambulance cot in a position of comfort, limiting movement of the spine during the process. 6. Patients, who are stable, alert and without neurological deficits may be allowed to self-extricate to the ambulance cot after placement of a cervical collar. Limit movement of the spine during the process. 7. Patients over the age of 65 with a mechanism of injury with the potential for causing cervical spine injury will have a cervical collar applied even if the spinal injury clinical assessment is negative. Specific Techniques 1. -

R Mackenzie, R Sutcliffe. Pre-Hospital Care: the Trapped Patient
J R Army Med Corps: first published as 10.1136/jramc-146-01-09 on 1 February 2000. Downloaded from J R Army Med Corps 2000; 146: 39-46 Pre-hospital Care: The Trapped Patient Maj R Mackenzie PhD, MRCP, Dip IMC RCSEd, RAMC(V) Maj R Sutcliffe MA, MRCGP, Dip IMC RCSEd, RAMC(V) 254 (City of Cambridge) Field Ambulance (V), 450 Cherry Hinton Road, Cambridge, CB1 8HQ. Introduction entrapment for an average of 44 minutes (5). In England and Rescue of the injured has always been an inherent feature of Wales between 1996 and 1997, the Fire Service rescued an peacetime and operational medical support (1). Despite this, estimated 10,000 people trapped in vehicles following road doctrine and skills training in technical rescue and extrication has accidents. Thirty percent of these incidents involved more than not been formally developed for Army Medical Services (AMS) one casualty (6). personnel (2). This is in stark contrast to the civilian emergency Collisions with other vehicles account for the majority of road services who have the capability of delivering a wide range of accident casualties (7) with head on, front-oblique, side impact rescue skills (Box 1). One of the most common situations in and rollover impacts involving proportionally more seriously which casualties require rescue is entrapment following a road injured casualties than other collisions (8). In rural areas, 75% of traffic accident. Road accidents, although relatively infrequent, entrapments occur after head on, front-oblique and side impacts. account for over half of all MoD injury deaths and are more In built-up areas, these accident types account for 90% of common on operations (3). -

Palm Beach County Fire Rescue
PALM BEACH COUNTY FIRE RESCUE BLS STANDING ORDERS 12-14 ALS STANDING ORDERS 16-25 ALS STANDING ORDERS 17-21 TRANSPORT DESTINATIONS 22-25 BASIC LIFE SUPPORT 26-31 BLS MEDICAL EMERGENCIES 27-28 BLS TRAUMA EMERGENCIES 29-30 BLS ENVIRONMENTAL 31 ALS MEDICAL EMERGENCIES 32-50 ALLERGIC REACTIONS 33-34 ALTERED MENTAL STATUS 35 DIABETIC EMERGENCIES 36-37 DYSTONIC REACTION 38 FLUID RESUSCITATION 39 HYPERKALEMIA 40 NAUSEA/VOMITING 41 RESPIRATORY DISTRESS 42-44 SEIZURES 45 SEPSIS 46-47 STROKE 48-50 TABLE OF CONTENTS 3 PALM BEACH COUNTY FIRE RESCUE CARDIAC EMERGENCIES 52-66 ATRIAL FIB/FLUTTER 53 BRADYCARDIA 54-55 CARDIOGENIC SHOCK 56 CHEST PAIN 57 STEMI ALERT 58-59 CHF/PULMONARY EDEMA 60 SVT 61-62 WIDE COMPLEX TACHYCARDIA 63-64 POLYMORPHIC V-TACH 65 LVAD 66 CARDIAC ARREST 68-78 STANDING ORDERS 69-71 ADULT ALGORITHM 72 PEDIATRIC ALGORITHM 73 SPECIAL CONSIDERATIONS 74-75 POST RESUSCITATION 76-77 INDUCED COOLING (ICE) 78 TABLE OF CONTENTS 4 PALM BEACH COUNTY FIRE RESCUE OVERDOSE 80-87 STANDING ORDERS 81-82 BETA BLOCKER 83 CALCIUM CHANNEL BLOCKER 84 COCAINE 85 NARCOTIC 86 TRICYCLIC 87 CHEMICAL CONTROL 88-95 PHYSICAL RESTRAINT 89 EXCITED DELIRIUM 90 VIOLENT/COMBATIVE PATIENT 91 PAIN MANAGEMENT 92-93 ADVANCED AIRWAY 94-95 ENVIRONMENTAL 96-105 DECOMPRESSION SICKNESS 97 FATAL/NON-FATAL DROWNING 98-99 HEAT EMERGENCIES 100-101 BITES AND STINGS 102-103 CARBON MONOXIDE EXPOSURE 104 CYANIDE EXPOSURE 105 TABLE OF CONTENTS 5 PALM BEACH COUNTY FIRE RESCUE TRAUMA 106-130 STANDING ORDERS 107 START TRIAGE 108 JUMP START TRIAGE 109 SCORECARDS 110-112 TRAUMA ARREST 113 -
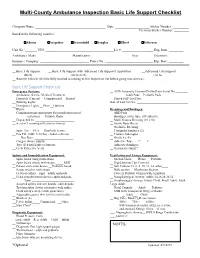
Basic Life Support Checklist
Multi-County Ambulance Inspection Basic Life Support Checklist Company Name: ___________________________________________ Date: _____________________ Sticker Number: __________ Previous Sticker Number: _________ Based in the following counties: Adams Arapahoe Broomfield Douglas Elbert Jefferson Unit No.: _______ VIN: __________________________________________Lic #: ___________________ Exp. Date: _________ Ambulance Make: _____________________ Manufacturer: ________________________ Year: ________ Odometer: _________ Insurance Company: ______________________________ Policy No.: _____________________________ Exp. Date: _________ __Basic Life Support __Basic Life Support with Advanced Life Support Capabilities __Advanced Life Support (BLS) (BLS/ALS) (ALS) __ Reserve Vehicle (Will be fully stocked according to this Inspection list before going into service.) Basic Life Support Check List Emergency Systems: __ AED-Automatic External Defibrillator Serial No ________ __ Ambulance Service Medical Treatment __Adult Pads __Pediatric Pads Protocols (Current) __Computerized __Printed __ Passed Self-Test Date:____________ __ Running Lights Date of Last Service: _________________________________ __ Emergency Lights __Siren __Opticom __Wipers Dressings and Bandages: __ Communications appropriate for jurisdiction served. __ ABD Pads __cell phone __ Portable Radio __ Bandages, roller type, self-adhesive __ Dispatched by: _________________________ __ Multi Trauma Dressing (10 x 36) __ A set of 3 warning reflectors or devices. __ Sterile Burn Sheets ______________________________________ -

Arkansas State Board of Health Section of Emergency Medical Services
ARKANSAS STATE BOARD OF HEALTH SECTION OF EMERGENCY MEDICAL SERVICES RULES AND REGULATIONS FOR EMERGENCY MEDICAL SERVICES Promulgated Under the Authority of Act 435 of 1975 Effective August 1st, 2016 By the Arkansas State Board of Health Arkansas Department of Health Little Rock, Arkansas (Nathaniel Smith, MD, MPH, Director) 1 EMS RULES AND REGULATIONS TABLE OF CONTENTS 2 AUTHORITY 4 I. DEFINITIONS 4 II. PURPOSE 10 III. LICENSURE OF AMBULANCE SERVICES 10 1. GENERAL STANDARDS 10 IV. GROUND AMBULANCE SERVICE LICENSURE CLASSIFICATION 15 1. AMBULANCE SERVICECLASSIFICATIONS 15 2. GENERAL STANDARDS 15 3. ALS LEVEL 17 4. BLS LEVEL 18 5. ADVANCED RESPONSE 18 6. EMT SPECIALTY 18 7. EMT VOLUNTEER 19 8. MEDICAL FACILITY TRANSPORT SERVICE 19 V. PERMITTING OF GROUND EMERGENCY VECHICLES 20 1. GENERAL STANDARDS 20 2. AMBULANCE STAFFING STANDARDS 24 VI. AIR AMBULANCE STANDARDS 25 1. GENERAL STANDARDS 25 2. ROTOR WING SERVICES 28 3. FIXED WING SERVICES 29 VII. PERMITTING OF AIR AMBULANCE VECHICLES 30 1. GENERAL STANDARDS 30 2. SPECIFIC STANDARDS 31 3. AIR AMBULANCE STAFFING REQUIREMENTS 31 VIII. EMERGENCY MEDICALS SERVICES PERSONNEL SKILLS 38 1. APPROVED SKILLS FOR EMSPs 38 IX. EDUCATION, TESTING AND LICENSURE OF PERSONNEL 41 1. LICENSURE LEVELS 41 2. LICENSURE REQUIREMENTS 42 3. LAPSED LICENSURE 46 4. RECIPROCITY OF EMSPs 49 5. MILITARY PERSONNEL 50 X. HOSPITAL STAFFING 51 XI. GENERAL TRAINING SITE REQUIREMENTS 51 XII. EMS EDUCATION PROGRAM REQUIREMENTS 53 XIII. EMSP EDUCATION STANDARDS AND LICENSURE 58 2 XIV. DRUGS AND PHARMACEUTICALS 62 XV. TRAUMA SYSTEMS 65 XVI. VIOLATIONS 67 XVII. SEVERABILITY 72 XVIII. REPEAL 72 CERTIFICATION 73 APPENDIX 1 - Required Equipment (ALL LEVELS) 2 - Field Triage Decision Scheme: The Arkansas Trauma Triage Protocol 3 RULES AND REGULATIONS PERTAINING TO EMERGENCY MEDICAL SERVICES AUTHORITY The following Rules and Regulations Pertaining to Emergency Medical Services are duly adopted and promulgated by the Arkansas State Board of Health pursuant to the authority expressly conferred by the Laws of the State of Arkansas in Ark. -

Attachment 18 EMS TREATMENT PROTOCOLS ADULT & PEDIATRIC
National Highway Traffic Safety Administration Technical Assistance Program Statewide EMS Re-Assessment Attachment 18 EMS TREATMENT PROTOCOLS ADULT & PEDIATRIC 18 Iowa Department of Public Health BUREAU OF EMERGENCY AND TRAUMA SERVICES Statewide EMS TREATMENT PROTOCOLS ADULT & PEDIATRIC January 2015 LUCAS STATE OFFICE BUILDING DES MOINES, IOWA 50319-0075 (515) 281-0620 (800) 728-3367 www.idph.state.ia.us/ems IOWA EMS TREATMENT PROTOCOLS Table of Contents Contents Introduction .................................................................................................................................................. 2 Protocol Authorization .............................................................................................................................. 3 Protocol Medications ............................................................................................................................... 4 Protocol Revisions ..................................................................................................................................... 4 Medical Director Statement of Affirmation .............................................................................................. 4 Adult Treatment Protocols ........................................................................................................................... 5 Pediatric Treatment Protocols .................................................................................................................... 47 Appendices .................................................................................................................................................