Ocular Neurosyphilis As First Manifestation of Infection in a Non
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Diagnostic Dilemma: Young Stroke in Neurosyphilis and HIV
Case Report Annals of Clinical Case Reports Published: 28 Jul, 2021 A Diagnostic Dilemma: Young Stroke in Neurosyphilis and HIV Prakash Narayanan*, Lai WS and Limun MF Department of Medicine, Tawau General Hospital, Malaysia Abstract A 36 years old gentleman was reported to have cerebrovascular accident. Patient was found to have positive serology for syphilis and retroviral disease. The case discussed in this report is to ascertain the importance of diagnosing neurosyphilis based on a high index of clinical suspicion including history and imaging and not only based on CSF VDRL test. This case report is also aimed to establish neurosyphilis as an important etiology for young stroke. Background Syphilis is systemic illness that have wide spectrum of clinical manifestations starting from chancre (early syphilis) that can results as neurosyphilis (late syphilis) among untreated patients. In HIV patients, neurosyphilis are frequents and which nearly 10% of untreated syphilis patients can develop neurosyphilis [1]. Neurosyphilis have varies manifestation depending on clinical dominant at presentations of diagnosis; neuropsychiatric, meningovascular and myelopathic [2]. However, there are challenges in diagnosing neurosyphilis among HIV patients. Here in we report a case of neurosyphilis with clinical presentation of young stroke in HIV patient. Case Presentation A 36-years old gentleman who experienced of multiple sexual partners presented with sudden onset of right sided body weakness and headache for 2 days prior to admission. Clinical evaluations revealed he had normal mental function (MMSE 25/25). His motor examination showed power of right upper limb of 0/5 and power of right lower limb of 1/5 with positive Babinski sign on the right side. -

Role of Intuitive Knowledge in the Diagnostic Reasoning of Hospital Specialists: a Focus Group Study
Open access Research BMJ Open: first published as 10.1136/bmjopen-2018-022724 on 28 January 2019. Downloaded from Role of intuitive knowledge in the diagnostic reasoning of hospital specialists: a focus group study Nydia Van den Brink,1 Birgit Holbrechts,1 Paul L P Brand,2 Erik C F Stolper,1,3 Paul Van Royen3 To cite: Van den Brink N, ABSTRACT Strengths and limitations of this study Holbrechts B, Brand PLP, et al. Background and objective Intuition is an important part Role of intuitive knowledge of human decision-making and can be explained by the ► This is the first study exploring the role of intuition in in the diagnostic reasoning dual-process theory where analytical and non-analytical of hospital specialists: a hospital specialists’ diagnostic reasoning. reasoning processes continually interact. These processes focus group study. BMJ Open ► The study was performed in two European countries. can also be identified in physicians’ diagnostic reasoning. 2019;9:e022724. doi:10.1136/ ► The used qualitative approach enabled the re- The valuable role of intuition, including gut feelings, has bmjopen-2018-022724 searchers to study the views of specialists on the been shown among general practitioners and nurses, but topic and the meanings they attach to the concept. ► Prepublication history for less is known about its role among hospital specialists. ► It was not the aim of the researchers to gather data this paper is available online. This study focused on the diagnostic reasoning of hospital To view these files, please visit for the calculation of predictive values of intuitive specialists, how they value, experience and use intuition. -

Taking the Mystery out of Abnormal Pupils
Taking the mystery out of abnormal pupils No financial disclosures Course Title: Taking the mystery out [email protected] of abnormal pupils Lecturer: Brad Sutton, OD, FAAO Clinical Professor IU School of Optometry . •Review of Anatomy Iris anatomy Iris sphincter Iris dilator Parasympathetic pathway Sympathetic pathway Parasympathetic Pathway Parasympathetic Pathway Light stimulates the retina then impulse Four neuron arc travels with the ganglion cells through the Retina to the pretectal nucleus in the chiasm into the optic tracts. 80% go to the midbrain (1) LGN , 20% to the pretectal nuclei.They Pretectal nucleus to the EW nucleus (2) then hemidecussate and terminate at the EW nucleus EW nucleus to the ciliary ganglion (3) Ciliary ganglion to the iris sphincter with short ciliary nerves (4) 1 Points of Interest Sympathetic Pathway Within the second order neuron there are Three neuron arc 30 near response fibers for every light Posterior hypothalamus to ciliospinal response fiber. This allows for light - near center of Budge ( C8 - T2 ). (1) dissociation. Center of Budge to the superior cervical The third order neuron runs with cranial ganglion in the neck (2) nerve III from the brain stem to the ciliary Superior cervical ganglion to the dilator ganglion. Superficially located prior to the muscle (3) cavernous sinus. Points of Interest Second order neuron runs along the surface of the lung, can be affected by a Pancoast tumor Third order neuron runs with the carotid artery then with the ophthalmic division of cranial nerve V 2 APD Testing testing……………….AKA……… … APD / reverse APD Direct and consensual response Which is the abnormal pupil ? Very simple rule. -

A Rare Case of Tabes Dorsalis
Journal of Gynecology and Women’s Health ISSN 2474-7602 Case Report J Gynecol Women’s Health Volume 17 Issue 2- November 2019 Copyright © All rights are reserved by Tobe S Momah DOI: 10.19080/JGWH.2019.17.555960 A Rare Case of Tabes Dorsalis Tobe S Momah*, Bhavsar Parth, Jones Shawntiah, Berry Kelsey and Duff David Department of Family Medicine, University of Mississippi Medical Center, USA Submission: November 05, 2019; Published: November 12, 2019 *Corresponding author: Tobe S Momah, Department of Family Medicine, University of Mississippi Medical Center, USA Background Tabes Dorsalis has become a rare clinical presentation in cases of neuro syphilis since the advent of antibiotics. The recent surge in syphilis cases [1], however, has once again raised interest in the diagnosis and treatment of this rare clinical entity. In this case report, a case of tabes dorsalis in an 82 year African American female is presented. She, also, had right peroneal nerve mono neuropathy that challenged the clinical diagnosis of tabes dorsalis and complicated its management. Keywords: Emergency room; Patient’s laboratory; Arterial duplex; Neurology; Magnetic Resonance; Cerebro Spinal; Serology returned; Physical therapy; Tabes dorsalis Abbreviatations: ER: Emergency Room; CT: Computerized Tomography; MRI: Magnetic Resonance Imaging; CSF: Cerebro Spinal Fluid; RPR: Rapid Plasma Reagin; EMG: Electromyography; PT: Physical Therapy Case Report ness of breath, chest pain or loss of consciousness. Patient’s lab- oratory values were significant for low copper (743mcg/l) and thrombocytopeniaPatient was assessed (64,000k/UL). in ER and determined to have impaired sensation in right lower extremity with inability to move the right leg in any direction. -

New Media for New Organs: a Virtual Community For
462-469 CON342344 Bers_CON 170x242mm 06/10/2009 16:29 Page 462 Convergence: The International Journal of Research into New Media Technologies Copyright © The Author(s), 2009. Reprints and permissions http://www.sagepub.co.uk/journalsPermissions.nav FEATURE REPORT London, Los Angeles, New Delhi, Singapore, and Washington DC Vol 15(4): 462–469 DOI: 10.1177/1354856509342344 http://con.sagepub.com New Media for New Organs A Virtual Community for Pediatric Post-Transplant Patients Marina U. Bers Tufts University, USA Abstract / This article describes an eight-month pilot study in which 19 pediatric post-transplant patients at Children’s Hospital Boston, ages 11 to 15, used a computer-based psychosocial inter- vention developed on the Zora 3D multiuser environment. Zora provides tools to create an online virtual city and populate it with houses and personally-meaningful objects. Users can communicate with each other via real-time chat and participate in open-ended guided activities to create a social network of peers. Preliminary results support the idea that innovative technologies can help adoles- cent patients to create a support network of peers when face-to-face interactions are impossible. Key Words / children’s virtual community / health care / multi-user virtual environment / online games / real-time chat Introduction New media is having an impact in the way children learn, play and communicate. From video-games to virtual tutors, from I-pods to on-line shopping, today’s children are immersed in a culture in which computers and the internet are vastly used for most of their needs (Subrahmanyam et al., 2001). Most recently, these needs have also started to expand to health care. -

Nicole Marie Psaltis, O.D. WJB Dorn VAMC, Columbia SC Residents Day Proposal August 30, 2010
Nicole Marie Psaltis, O.D. WJB Dorn VAMC, Columbia SC Residents Day Proposal August 30, 2010 • Abstract ‐ Retinitis pigmentosa (RP) is a group of inheritable eye conditions, constituting retinal and RPE dystrophies, which progress to vision loss. Patients with identical genetic mutations can manifest different phenotypic presentations. This case describes an atypical presentation of RP. • Case History ‐ A 57‐year‐old Caucasian male veteran presented to the Wm. Jennings Bryan Dorn VA Eye Cinic in Columbia, South Carolina on June 23, 2009 ‐ Chief Complaint Decreasing peripheral field of vision The patient had a secondary complaint of painless blurred vision distance and near of gradual onset ‐ Ocular History Hyperopic astigmatism OU Unremarkable ocular health history per patient’s account Last eye exam was 2.5 years ago ‐ Medical History Alcohol abuse Esophageal reflux Hypercholesterolemia Hypothyroidism Depression PTSD Substance Abuse ‐ Medications Citalopram Hydrobromide Hydrochlorothiazide Nicotine Patch Omeprazole Simvastatin Trazodone ‐ Allergies Naproxen ‐ Family Ocular History Unremarkable ‐ Pertinent Findings Entering VA: 20/25+2 OD, 20/25 OS cc Pupils: PERRL (‐) APD EOM: FROM OU CVF: Constricted OU Subjective Refraction: +2.00‐2.00x109 OD +2.25‐1.25x065 OS Anterior Segment Evaluation: WNL OU Tap: 13 mmHg OD, 14 mmHg OS @ 1109 AM DFE: Atrophic presentation with distinct cessation perifoveally OU. Coalesced hyperplastic lesions, rarely in bone spicule appearance, scattered throughout posterior pole OU. Scattered areas of atrophy of scalloped appearance in far periphery to ora serrata. Vessels are mildly narrow and attenuated OU. Maculae were flat and intact OU. The optic nerve cup‐to‐disc ratios are 0.10, round OU. The presentation is symmetrical. -
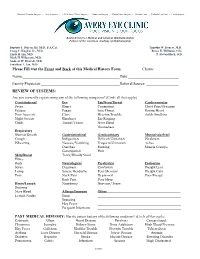
Please Fill out the Front and Back of This Medical History Form. Chart#: Name: Date: Family Physician: Referral Source: REVI
Advanced Cataract Surgery • Lens Implants • LASIK Laser Vision Surgery • Glaucoma Surgery • Retina Laser Surgery • Contact Lens • Pediatric Eye Care • Eyelid Surgery Board-Certifie d Medical and Surgical Ophthalmologists Fellows of the American Academy of Ophthalmology Baptiste J. Dejean, III, M.D., F.A.C.S. Timothy W. Doucet, M.D. Craig C. Kuglen, Jr., M.D. Renee E. Williams, O.D. Linda H. Lin, M.D. P. Steven Black, O.D. Mark H. Wilkerson, M.D. Andrew W. Dvorak, M.D. Jonathan T. Jan, M.D. Please Fill Out the Front and Back of this Medical History Form. Chart#: Name: Date: Family Physician: Referral Source: REVIEW OF SYSTEMS: Are you currently experiencing any of the following symptoms? (Circle all that apply) Constitutional Eye Ear/Nose/Throat Cardiovascular Fever Blurry Congestion Chest Pain/Pressure Fatigue Foggy Sore Throat Racing Heart Poor Appetite Glare Hearing Trouble Ankle Swelling Night Sweats Blindness Ear Ringing Chills Tunnel Vision Nose Bleed Hoarseness Respiratory Short of Breath Gastrointestinal Genitourinary Musculoskeletal Cough Indigestion Difficult Urination Weakness Wheezing Nausea/Vomiting Frequent Urination Aches Diarrhea Burning Muscle Cramps Constipation Pain Skin/Breast Tarry/Bloody Stool Hives Rash Neurological Psychiatric Endocrine Sores Dizziness Confusion Weight Loss Lump Severe Headache Poor Memory Weight Gain Pain Neck Pain Depressed Poor Energy Back Pain Poor Sleep Heme/Lymph Numbness Nervous/Tense Bruising Nose Bleed Allergy/Immune Other: Lymph Nodes Sinus Sneezing Hay Fever Frequent Infections PAST MEDICAL HISTORY: Has the patient had any of the following conditions? (Circle all that apply) Cataracts Ulcer Heart Disease Paralysis Cancer (type): Glaucoma Jaundice Kidney Stone Drug Addiction High Blood Pressure Hay Fever Gallstone Bladder Trouble Prostate Trouble Tuberculosis Asthma Liver Disease Thyroid Disease Nerve Disease Anemia Diabetes Hepatitis Stroke Muscle Disease Bleeding Disorder Pneumonia Colitis Infections Seizure High Cholesterol (over) OTHER EYE OR MEDICAL PROBLEM: Eye/Medical Issue Date Eye/Medical Issue Date 1. -
Setting High Standards of Care for Low Vision
Low Vision Treatment Setting High Standards of Care for Low Vision www.neoretina.com Thousands of Indians suer from low vision. Are you one among them? Low Vision is a condition of visual impairment that cannot be corrected through glasses, medicines or surgical treatments. The condition is often characterized by partial sight, blurred vision, tunnel vision or blind spots. Low vision impacts both adults and children but mostly occurs among adults above 60 years of age. Losing the ability to perform basic activities: drive, read, watch or view, etc. can make one feel shut o from living a normal life. What causes low vision? Generally, the low vision condition is caused by eye diseases or health conditions such as Age-related Macular Degeneration (AMD), Cataract, Diabetic Retinopathy, Retinitis Pigmentosa, Stargardt's Disease (juvenile Macular Degeneration) and Glaucoma. Eye injuries, congenital disabilities and brain damages are some other causes. The chances to restore eyesight due to low vision are unlikely, but it can be managed with proper devices and vision rehabilitation. How do you know if you have low vision? A person with low vision condition has poor eyesight, where he is unable to perform routine duties, despite regular glasses, medicine, and surgery. Commonly individuals with low vision can have diculty in: Reading and writing Using a Computer/Tablet or watching Reading trac signals, Television name boards, etc. Spotting switches, dials or other Recognizing familiar faces mechanical controls Neoretina: Comprehensive & Technologically Enhanced Centre for Low Vision Treatment Neoretina Eyecare Institute, Hyderabad oers world-class treatment in the management of the low vision and other eye conditions. -

Neurosyphilis Presenting As Intermittent Explosive Disorder and Acute Psychosis
Open Access Case Report DOI: 10.7759/cureus.6337 Neurosyphilis Presenting as Intermittent Explosive Disorder and Acute Psychosis Harneel S. Saini 1 , Matthew Sayre 2 , Ishveen Saini 3 , Nehad Elsharkawy 4 1. Neurology, Allegheny General Hospital, Pittsburgh, USA 2. Internal Medicine, Lewis Katz School of Medicine at Temple University, Philadelphia, USA 3. Internal Medicine, Lake Erie College of Osteopathic Medicine (LECOM), Erie, USA 4. Pharmacy, Lake Erie College of Osteopathic Medicine (LECOM), Bradenton, USA Corresponding author: Harneel S. Saini, [email protected] Abstract We present a case of a patient with tertiary syphilis, manifesting as acute psychosis, auditory hallucinations and intermittent explosive disorder with pending legal ramifications for physical violence. Our patient had been seen and treated by a psychologist with Aripiprazole for his erratic and aggressive behavior coupled with his new found psychosis over a one-year period with no avail. Prior accounts of interaction with the patient described him as “easy going”, “laid back”, and cooperative. Our patient had a complete return to baseline mentation and functionality post treatment with 4 Million Units every four hours of penicillin for two weeks. Neurosyphilis is a disease that greatly affects the mental functioning capacity of those infected. While treatment of syphilis has become greatly straightforward, those living in impoverished conditions and without a continual access to the health care system can progress through the stages of syphilis. It is of vital importance to keep syphilis on our differential for patients with rapidly progressing and broadly encompassing psychiatric disturbances especially in patients that have a lower socioeconomic status. Categories: Public Health, Neurology, Infectious Disease Keywords: syphilis Introduction Syphilis is a sexually transmitted disease caused by the gram-negative bacteria, Treponema pallidum. -

Transplant Chronicles
Transplant Chronicles Volume 6 A publication for transplant recipients of all organs and their families, Number 2 published by the National Kidney Foundation, Inc. Crossing the Finish Line by Jennifer Kinlund y ordeal started when I During the seventh grade, I wasM only 18 months old, with a was ready to begin an active flu virus I picked up on a life in the world of sports, but family vacation. After a few that was not to be. The doctor days I was still not getting who did my sports physical better and was brought to the informed me that I did not pass hospital. I was given fluids the physical due to a high through an I-V because I was protein level in my urine. I dehydrated. The nursing staff headed back to the Mayo Clinic did not do an adequate job of and found that I would need a monitoring the fluid, which transplant unless my kidney lead my kidneys to shut down. function stopped declining. My kidney function did not But the next few years showed return and therefore, I had to continued deterioration. I be put on dialysis. Luck was began a trial with prednisone, again not with me; part of the which did not help. So equipment needed for my throughout the next few years, dialysis treatment had to be I was on a restricted diet, and flown in from California, and it added routine blood pressure ended up in Washington. With checks and medicine to my surgery already scheduled, the daily routine. doctors had to use an adult piece to get the dialysis started, My senior year was the most as my body was beginning to Jennifer Kinlund (right) races her way to recovery difficult, as my kidney function shut down. -

Neurosyphilis Mimicking Autoimmune Encephalitis in a 52-Year-Old Man
PRACTICE | CASES CPD Neurosyphilis mimicking autoimmune encephalitis in a 52-year-old man Adrian Budhram MD, Michael Silverman MD, Jorge G. Burneo MD MSPH n Cite as: CMAJ 2017 July 24;189:E962-5. doi: 10.1503/cmaj.170190 52-year-old man in a long-term, same-gender sexual relationship presented with agitation, confusion and KEY POINTS problems speaking for about two weeks. On assess- • The rate of syphilis infection in Canada has risen in recent years. ment,A his vital signs were normal, but he was agitated and had • Early neurosyphilis typically presents as meningitis or global aphasia. No other focal deficits were identified on a meningovascular disease, while late neurosyphilis classically screening neurologic examination. He suffered a witnessed gen- causes dementia or tabes dorsalis. eralized tonic–clonic seizure in the emergency department and • Neurosyphilis may rarely mimic autoimmune encephalitis, and was given a loading dose of phenytoin. Seizure activity stopped, recognition of this is critical to ensure accurate diagnosis and but his agitation, confusion and aphasia persisted. prompt treatment with antimicrobial therapy. Six months earlier, he had been admitted to hospital with agi- • Further study is needed to determine whether immunologic tation, disorientation and aphasia that had developed one month mechanisms contribute to this atypical presentation of neurosyphilis. after an episode of vertigo. Brain magnetic resonance imaging (MRI) had shown T2 hyperintensity of the left thalamus and medial temporal lobe (Figure 1). An electroencephalogram during this initial hospital admission showed left posterior temporal slowing, subacute neurologic decline with seizures, medial temporal lobe but no seizure activity. Lumbar puncture had shown inflamma- signal abnormality on initial MRI, and positive serum anti-GAD tory cerebrospinal fluid (CSF) with a leukocyte count of 72 × 106 antibody, a diagnosis of autoimmune encephalitis was consid- cells/L with 86% lymphocytes (normal 0–5 × 106 cells/L), elevated ered. -

A Case of Neurosyphilis in a Patient Presenting with Bipolar Mixed Episode Suggestive Symptoms
25th European Congress of Psychiatry / European Psychiatry 41S (2017) S303–S364 S347 Disclosure of interest The authors have not supplied their decla- Methods Review of clinical records and complementary exams. ration of competing interest. Results By the first admission, the patient presented with http://dx.doi.org/10.1016/j.eurpsy.2017.02.316 depressed and irritable mood, emotional lability, aggressiveness, grandiose and racing thoughts. Upon discharge, he was diagnosed with bipolar disorder and referred to ambulatory unit. The follo- EW0703 wing year he starts presenting cognitive deficits and a progressive The squeezing snake, a psychiatric loss of autonomy in daily living activities, being referred to neuro- presentation of epilepsy: A case report logy evaluation. A year after the first admission, he is admitted in a M. Mangas ∗, L. Bravo , Y. Martins , A. Matos Pires neurology unit and diagnosed with neurosyphilis. Hospital José-Joaquim Fernandes, mental health and psychiatric Conclusions Current prevalence of symptomatic neurosyphilis in service, Beja, Portugal Western Europe is unknown. Atypical cases presenting with hete- ∗ Corresponding author. rogeneous psychiatric and neurologic symptoms, with no previous history of mental illness, should raise a high index of clinical sus- Introduction Epilepsy is considered a complex neurological picion, since consequences for the patient’s health might be severe disorder with a great variety of clinical presentations that can if not properly diagnosed and treated. resemble psychiatric disorders. Disclosure of interest The authors have not supplied their decla- Objectives Disclose an unusual clinical case with psychiatric ration of competing interest. symptoms as the presentation of epilepsy. Methods Psychiatric assessments and retrospective review of the http://dx.doi.org/10.1016/j.eurpsy.2017.02.318 clinical file and literature research.