The Hybrid OR of the Future
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Patients and Staff in the Hybrid Operating Room Experiences and Challenges
Patients and Staff in the Hybrid Operating Room Experiences and Challenges May Bazzi Institute of Health and Care Sciences Sahlgrenska Academy, University of Gothenburg Gothenburg 2019 Cover illustration: Dario Soltani. The patients’ descriptions of the hybrid OR in Study I are shown in the puzzles. Patients and Staff in the Hybrid Operating Room: Experiences and Challenges © May Bazzi 2019 [email protected] ISBN 978-91-7833-702-6 (PRINT) ISBN 978-91-7833-703-3 (PDF) http://hdl.handle.net/2077/60818 Printed in Gothenburg, Sweden 2019 Printed by BrandFactory To Alicia Patients and Staff in the Hybrid Operating Room Experiences and Challenges May Bazzi Institute of Health and Care Sciences Sahlgrenska Academy, University of Gothenburg Gothenburg, Sweden ABSTRACT The hybrid operating room (OR), which combines a traditional OR with a radiological intervention room, is one example of the technical advancements within hospitals. In a hybrid OR, the staff have to manage the technique confidently in a not completely familiar environment and still be able to care for the vulnerable patient in the safest way. The overall aim of this thesis was to explore and describe the care and work processes, staff interactions, and experiences of both patients and staff in the hybrid OR. Data were collected through 18 individual interviews, nine video recordings of endovascular aortic repairs (EVARs) and five focus group interviews. Data were mainly analyzed qualitatively (hermeneutic, hermeneutic phenomenology and qualitative content analysis) but also with the use of descriptive statistics. The environment in the hybrid OR was experienced as safe by both patients and staff. -

How the Hybrid Operating Room Can Influence Cardiac Surgery
CLAUDIO GROSSI Cardiac Surgery Ospedale Santa Croce CUNEO (Italy) INNOVATIONS IN THE ENVIRONMENT: HOW THE HYBRID OPERATING ROOM CAN INFLUENCE CARDIAC SURGERY Impossibile visualizzare l'immagine. La memoria del computer potrebbe essere insufciente per aprire l'immagine oppure l'immagine potrebbe essere danneggiata. Riavviare il computer e aprire di nuovo il file. Se viene visualizzata di nuovo la x rossa, potrebbe essere necessario eliminare l'immagine e inserirla di nuovo. The hybrid surgical suite Basic equipment and design of the hybrid endovascular operating room § A fully integrated interventional hybrid operating room combines: Ø high level surgical sterility Ø flat-panel cardiovascular imaging, Ø a linked workstation with post processing and storage facilities § The imaging system must provide superior image quality, higher tube heat capacity Imaging techniques in the hybrid operating room • Rotational angiography is a medical imaging technique based on x-ray, that allows to acquire CT-like 3D volumes using a fixed C-Arm. • The fixed C-Arm thereby rotates around the patient and acquires a series of x-ray images that are then reconstructed through software algorithms into a 3D image. • Commercial name for Siemens is DynaCT Imaging techniques in the hybrid operating room • Rotational angiography versus angio CT • The patient positioning on the CT scanner table differs from the positioning on an interventional table during hybrid surgery, • Intraoperative 3D imaging with rotational angiography is much more precise and can be performed with rapid ventricular pacing. Advanced visualization in the hybrid operating room Examples of syngo DynaCT Cardiac Segmentations: Left atrium (red), Aorta (blue), Esophagus (green) Segmented left atrium Segmented aortic root with landmarks. -

Planning Premises and Design Considerations for Hybrid Operating Room 1V Siddharth, 2Sunil Kant, 3R Chandrashekhar, 4Shakti Kumar Gupta
JRFHHA V Siddharth et al 10.5005/jp-journals-10035-1015 REVIEW ARTICLE Planning Premises and Design Considerations for Hybrid Operating Room 1V Siddharth, 2Sunil Kant, 3R Chandrashekhar, 4Shakti Kumar Gupta ABSTRACT in the great changes that have developed in regard to the The hybrid operating room can be defined as the combination construction, and organization, of the modern operating 1 of imaging system and operating table installed in an operating theater suite. ‘OT has been defined as that specialized facility theater room for, e.g. use of an angiography imaging system of the hospital where lifesaving or life improving procedures and operation table in an operation theatre or use of an are carried out on the human body by invasive methods operating table in angiography room. Shorter patient recovery under strict aseptic conditions in a controlled environment time, decreased length of stay, streamlined care delivery, improvement in cross-specialty communication, minimized risk by specially trained personnel to promote healing and for communication-related errors across clinical specialties cure with maximum safety, comfort and economy’.2 and lower overall cost of care are some of the advantages of Imaging has a long history in the operating room (OR). the hybrid operating room. Although no/limited data exists in In the 1960s, X-ray units were mounted on the ceiling, the literature, the potential disadvantages of hybrid operating suite are cost, infection, prolonged anesthesia and radiation as they might be today. But the surgeon had to go to an exposure. The primary components of a hybrid operating suite adjacent room to view the image, and images could only are an imaging system and imaging compatible operation table. -

Improved Efficiency and Safety for EVAR with Utilization of a Hybrid
Improved Efficiency and Safety for EVAR with Utilization of a Hybrid Room5 V.N. Varu, J.I. Greenberg, J.T. Lee * Division of Vascular Surgery, Stanford University Medical Center, Stanford, CA, USA WHAT THIS PAPER ADDS This study is novel in that it shows for the first time inherent differences in doing endovascular aneurysm repair with a standard fluoroscopy versus hybrid operating room setup. The implication is that ultimately a hybrid room may be safer and more efficient in the long run, and perhaps a valued investment by hospitals across the world. Objective: Access to a hybrid endovascular suite is touted as a necessity for advanced endovascular aneurysm repair (EVAR) to improve imaging accuracy and safety. Yet there remain little data documenting this intuitive advantage of a hybrid setup versus a traditional operating room (OR) utilizing a portable fluoroscopic unit (C-arm) for imaging. We hypothesized that standard elective EVAR performed in a hybrid suite would improve procedural efficiency and accuracy, as well minimize patient exposure to both contrast and radiation. Methods: We retrospectively reviewed a single attending surgeon’s EVAR practice, which encompassed the transition to a hybrid endovascular suite (opened July 2010). Only consecutive abdominal aneurysms were included in the analysis to attempt to create a homogenous cohort. All emergent, aorto-uni-iliac (AUI), snorkel, fenestrated, or hybrid procedures were excluded. Standard variables evaluated and compared between the two study subgroups included fluoroscopy time, operative time, contrast use, stent-graft component utilization, complication rates, and short-term endoleaks. Results: From January 2008 to August 2012, we performed 213 EVAR procedures for abdominal aortic aneurysms. -

Capitalizing on the New Wave of Hybrid Ors
SPECIAL REPORT Capitalizing on the New Wave of Hybrid ORs Published by OR Manager and Access Intelligence Introduction www.ormanager.com SENIOR VP/GROUP PUBLISHER Jennifer Schwartz • 301-354-1702 An increasing number of hospitals nationwide now have hybrid [email protected] PUBLISHER, DEFENSE AND HEALTHCARE operating rooms. Building a new hybrid OR takes careful planning, Thomas A. Sloma-Williams • 301-354-1696 requires specialized and advanced audiovisual and imaging [email protected] EDITOR equipment, and involves the collaboration of many decision Elizabeth Wood • 301-354-1786 [email protected] makers. And once a hybrid OR is in place, procedures often require CLINICAL EDITOR teams from several disciplines to work together as one. This process Judith M. Mathias, MA, RN CONTRIBUTING WRITERS may be daunting, but the results may leave you in a better position Paula DeJohn, Cynthia Saver, MS, RN WEBINAR COORDINATOR to offer a variety of surgical procedures, enhance patient safety, and Ellen Lord, MS, RN, CNOR CONFERENCE DIRECTOR achieve long-term cost savings with improved efficiencies. Jess Tyler ART DIRECTOR Regardless of whether you’re building a new hybrid OR or Yelena Shamis remodeling to accommodate the new room within existing space, [email protected] SENIOR PRODUCTION MANAGER you must commit considerable financial and human resources. Joann M. Fato • 301-354-1681 [email protected] This special report provides insights from professionals who have ADVERTISING transitioned to a hybrid OR, offering tips and strategies to help National Advertising Manager Jamila Zaidi Account Executive, OR Manager you through the process. As with any transition, getting input from [email protected] 301-354-1678 physicians, anesthesiologists, nurses, technical staff, and other Fax: 301-340-7136 members of your team is crucial to success. -

Evaluation of the Radiation Dose Received by Patients
diagnostics Article Hybrid Operating Room System for the Treatment of Thoracic and Abdominal Aortic Aneurysms: Evaluation of the Radiation Dose Received by Patients Yoshihiro Haga 1,2, Koichi Chida 1,3,*, Masahiro Sota 1,2, Yuji Kaga 2, Mitsuya Abe 2, Yohei Inaba 1,3 , Masatoshi Suzuki 1,3 , Taiichiro Meguro 4 and Masayuki Zuguchi 1 1 Course of Radiological Technology, Health Sciences, Tohoku University Graduate School of Medicine, 2-1 Seiryo, Aoba, Sendai, Miyagi 980-8575, Japan; [email protected] (Y.H.); [email protected] (M.S.); [email protected] (Y.I.); [email protected] (M.S.); [email protected] (M.Z.) 2 Department of Radiology, Sendai Kousei Hospital, 4-15 Hirosemachi, Aoba, Sendai 980-0873, Japan; [email protected] (Y.K.); [email protected] (M.A.) 3 Department of Radiation Disaster Medicine, International Research Institute of Disaster Science, Tohoku University, 468-1 Aramaki Aza-Aoba, Aoba, Sendai, Miyagi 980-0845, Japan 4 Department of Cardiovascular Medicine, Sendai Kousei Hospital, 4-15 Hirose-machi, Aoba, Sendai 980-0873, Japan; [email protected] * Correspondence: [email protected]; Tel.: +81-22-717-7943 Received: 23 September 2020; Accepted: 10 October 2020; Published: 19 October 2020 Abstract: In recent years, endovascular treatment of aortic aneurysms has attracted considerable attention as a promising alternative to traditional surgery. Hybrid operating room systems (HORSs) are increasingly being used to perform endovascular procedures. The clinical benefits of endovascular treatments using HORSs are very clear, and these procedures are increasing in number. -

Imaging Meets Surgery – the Hybrid OR
Biomed Tech 2012; 57 (Suppl. 1) © 2012 by Walter de Gruyter · Berlin · Boston. DOI 10.1515/bmt-2012-4041 Imaging meets Surgery – The Hybrid OR C.J. Bulitta, MD, Siemens AG Healthcare Sector, Forchheim, Germany, [email protected] Abstract Introduction: The merger of interventional and open surgical procedures leads to novel approaches in various clinical fields. Imaging becomes a critical tool and success factor because it allows for visualization of the targeted anatomical structures and leads the way for the clinician. Moreover high-end imaging (Angiography, CT, MRI) available in the op- erating room allows for assessment of treatment results immediately at the point of care which helps to avoid complica- tions and the need for revision surgery. Methods: Operating rooms in various clinical fields are equipped with high-end imaging systems. The most prominent example is the angiography system in cardiovascular operating theatres. Require- ments for imaging and other medical equipment vary among clinical specialties. Infrastructure and building technology are also important topics for planning and implementation. Workflow and hygienic requirements should not be forgotten. Thus building a hybrid OR is a complex technical challenge. Based on the experience of more than 400 installed an- giography systems in Operating Rooms in more than 30 countries worldwide we have put together lessons learned and recommendations for planning and implementation. Results: Planning needs to consider all aspects and components from building technology to medical equipment. Early planning and room design with all stakeholders and balancing clinical requirements and technical feasibility is critical for success. Hygienic requirements vary significantly and there- fore should be discussed and considered according to local regulations. -
Hybrid Operating Room Design Basics
Hybrid Operating Room Design Basics November 2018 Mary Fearon, MSN, RN, CNOR FACILITY GUIDELINES INSTITUTE [email protected] www.fgiguidelines.org © 2018 The Facility Guidelines Institute www.fgiguidelines.org [email protected] About the Facility Guidelines Institute The Facility Guidelines Institute is a not-for-profit corporation founded in 1998 to provide leadership and continuity to the revision process for the Guidelines for Design and Construction documents. FGI functions as the coordinating entity for development of the Guidelines series of documents using a multidisciplinary, consensus-based process and for provision of ancillary services that encourage and improve their application and use. FGI invests revenue from sales of the Guidelines documents to fund the activities of the next revision cycle as well as research that can inform the Guidelines development process. FGI Disclaimers This document is provided for informational purposes only and is not and should not be construed as legal advice. The views and opinions expressed in this document are the opinions of the author and not the official position of FGI or the Health Guidelines Revision Committee. The information provided in this document may not apply to a reader’s specific situation and is not a substitute for application of the reader’s own independent judgment or the advice of a competent professional. Neither FGI nor the author makes any guaranty or warranty as to the accuracy or completeness of any information contained in this document. FGI and the author disclaim liability for personal injury, property damage, or other damages of any kind, whether special, indirect, consequential, or compensatory, that may result directly or indirectly from use of or reliance on this document. -

A Bottom-Up Cost Analysis of Both a Hybrid Operating Room and Conventional Operating Room
http://ijhpm.com Int J Health Policy Manag 2020, x(x), 1–9 doi 10.34172/ijhpm.2020.119 Original Article Understanding the Costs of Surgery: A Bottom-Up Cost Analysis of Both a Hybrid Operating Room and Conventional Operating Room Sejal Patel1*¶ ID , Melanie Lindenberg2,3¶ ID , Maroeska M. Rovers1,4, Wim H. van Harten2,3, Theo J.M. Ruers5, Lieke Poot6, Valesca P. Retel2,3, Janneke P.C. Grutters1,4 ID Abstract Article History: Background: Over the past decade, many hospitals have adopted hybrid operating rooms (ORs). As resources are limited, Received: 6 January 2020 these ORs have to prove themselves in adding value. Current estimations on standard OR costs show great variety, while Accepted: 29 June 2020 cost analyses of hybrid ORs are lacking. Therefore, this study aims to identify the cost drivers of a conventional and ePublished: 27 July 2020 hybrid OR and take a first step in evaluating the added value of the hybrid OR. Methods: A comprehensive bottom-up cost analysis was conducted in five Dutch hospitals taking into account: construction, inventory, personnel and overhead costs by means of interviews and hospital specific data. The costs per minute for both ORs were calculated using the utilization rates of the ORs. Cost drivers were identified by sensitivity analyses. Results: The costs per minute for the conventional OR and the hybrid OR were €9.45 (€8.60-€10.23) and €19.88 (€16.10- €23.07), respectively. Total personnel and total inventory costs had most impact on the conventional OR costs. For the hybrid OR the costs were mostly driven by utilization rate, total inventory and construction costs. -

Treatment of a Giant Meningioma in a Hybrid OR Prof
Feels right at first sight Treatment of a giant meningioma in a hybrid OR Prof. Jiang Weijian, MD, PLA Stroke Care & Research Center, The Second Artillery General Hospital of Chinese People’s Liberation Army, Beijing, China Illustrated workflows in hybrid operating rooms, No. 10 PLA Stroke Care & Research Center Prof. Jiang Weijian, MD PLA Stroke Care & Research Center is the first Other on-site facilities include a neurological center in the People’s Republic of China with a intensive care unit, a hybrid operating room, neurovascular hybrid operating room featuring neuro-endovascular therapy suites and a multi- Artis zeego, a robot-supported 3D angiography media conference room. system. The center is one of the world’s most Since 2012 Prof. Jiang Weijian, MD has been renowned centers for the management of head of the New Era Stroke & Research Insti- cerebral vascular disease. It provides compre- tute and vice president of The Second Artillery hensive diagnostic and therapeutic care for General Hospital of Chinese PLA. patients with disorders of blood vessels of the brain, including • Ischemic and hemorrhagic stroke • Transient ischemic attack • Chronic carotid occlusion or stenosis • Cerebral hemorrhage • Cerebral aneurysms and subarachnoidal hemorrhage • Dural arteriovenous fistula (DAVF) • Arteriovenous malformation (AVM) • Hypervascular brain tumors 2 Clinical Case Removal of a giant meningioma A 61-year-old female patient with walking unsteadiness was diagnosed with a brain tumor which was regularly controlled for over two years. The patient decided for surgical tumor removal due to significant increase of the walking unsteadiness. MRI showed a giant tumor located in the right temporal-occipital lobe, size approximately 7 cm x 5.7 cm x 7.5 cm. -

Our Experience with Trinias Biplane and Hybrid Operating Room Systems
Vascular Our Experience with Trinias Biplane and Hybrid Operating Room Systems Department of Cardiology, Mitsubishi Kyoto Hospital Masashi Kato, M.D. Masashi Kato 1. Overview of the hospital 2. Background The Mitsubishi Kyoto Hospital was established in Our cardiovascular internal medicine physicians 1946 as a company hospital for the employees of work closely with cardiovascular surgeons for Kyoto Machinery Works, Mitsubishi Heavy treatment of a wide range of cardiovascular Industries Ltd. The hospital is currently affiliated disorders. In the fiscal year 2014, we performed with Mitsubishi Motors Corporation, a spinoff from 306 percutaneous coronary interventions (PCI), the parent company in 1970. Located in the 160 endovascular treatments (EVT) (including southwest part of Kyoto city, the Mitsubishi Kyoto shunt PTA), 84 pacemaker surgeries (including Hospital is a 188-bedded hospital (general ward, biventricular pacing and ICD), 122 cardiovascular 174 beds; ICU/CCU, 8 beds; and NICU, 6 beds). surgeries, and 14 aortic stent graft procedures. In Ever since its establishment, the hospital has the recent years, there has been a steady increase played a vital role as a central hospital in the in the number of conditions that are amenable to region, which caters to not only the Mitsubishi percutaneous interventions via catheters. Moreover, employees and their families but also the general because of the aging population, the need for less public living in the area. Immediately after its invasive interventions is increasing. Given the inception, it served as the nodal hospital for the demographic trends, a hybrid operating room treatment of tuberculosis and other communicable where surgery and percutaneous interventions can diseases. -
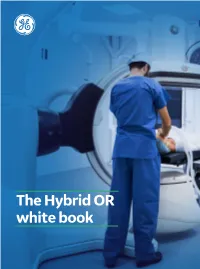
The Hybrid OR White Book Introduction
The Hybrid OR white book Introduction The explosion in image-guided minimally invasive therapies marks a paradigm shift in the surgical world. Success in this new world requires addressing new challenges: • Multidisciplinary collaboration to perform complex, patient-tailored procedures. • Multidisciplinary usage to satisfy diverse imaging and workflow requirement. And that, in turn, requires one sophisticated suite that provides advanced imaging and high flexibility for precise, image-guided therapies while maximizing OR utilization. The intent of this book is to guide you in your Hybrid OR project journey, share with you some advices and key points to consider. Each project is different and needs to fit your specific needs and requirements. This book shall give some concrete elements to help you drive this initiative. Enter GE Healthcare’s multidisciplinary, hybrid operating suite. Offering a new standard of care for the OR of today and the future. 2 | The HOR white book The HOR white book | 3 CHAPTER 1 | What is a Hybrid Operating Room?. 05 HOR definitions. 06 The advent of hybrid Operating Rooms. 06 Clinical specialties involved ............................................................ 07 CHAPTER 2 | How to manage an HOR project? ................ 08 Discover the Hybrid Suite .............................................................. 09 Define the business case ............................................................... 09 Involve the stakeholders and define project leaders .................................. 09 Define your