A Review on the Value of Imaging in Differentiating Between Large Vessel Vasculitis and Atherosclerosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Documentationand Coding Tips: Peripheral Vascular Disease
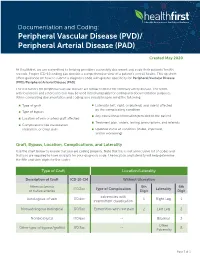
Documentation and Coding: Peripheral Vascular Disease (PVD)/ Peripheral Arterial Disease (PAD) Created May 2020 At Healthfirst, we are committed to helping providers accurately document and code their patients’ health records. Proper ICD-10 coding can provide a comprehensive view of a patient’s overall health. This tip sheet offers guidance on how to submit a diagnosis code with greater specificity for Peripheral Vascular Disease (PVD)/Peripheral Arterial Disease (PAD). The risk factors for peripheral vascular disease are similar to those for coronary artery disease. The terms arteriosclerosis and atherosclerosis may be used interchangeably for coding and documentation purposes. When completing documentation and coding, you should keep in mind the following: Type of graft Laterality (left, right, or bilateral) and side(s) affected by the complicating condition Type of bypass Any educational information provided to the patient Location of vein or artery graft affected Treatment plan, orders, testing, prescriptions, and referrals Complications like claudication, ulceration, or chest pain Updated status of condition (stable, improved, and/or worsening) Graft, Bypass, Location, Complications, and Laterality Use the chart below to ensure that you are coding properly. Note that this is not an inclusive list of codes and that you are required to have six digits for your diagnosis code. The location and laterality will help determine the fifth and sixth digits for the codes. Type of Graft Location/Laterality Description of Graft ICD-10-CM Without -

Report on the Cooperative Study of Intracranial Aneurysms And
Report on the Cooperative Study of Intracranial Aneurysms and Subarachnoid Hemorrhage SECTION VIII, Part I Results of the Treatment of Intracranial Aneurysms by Occlusion of the Carotid Artery in the Neck HIRO NISHIOKA, M.D.* Introduction In a late postoperative study of retinal artery CCLUSION of the cervical portion of the pressures in 13 patients with carotid liga- carotid artery has been employed tion, Christiansson '6~ found eight patients O since 1885 as a definitive treatment who had maintained pressure drops of 20 per for intracranial aneurysm. The resultant re- cent or more over a period of from 1 to 13 duction of intra-arterial pressure is expected years. The observation that there was stasis to reduce the likelihood of subsequent of blood within the aneuwsmal sac after hemorrhage. The alteration of blood flow carotid occlusion was made at angiography characteristics within the aneurysmal sac by Eeker and Riemenschneider '51. During may encourage thrombosis with organization digital carotid occlusion, they found that and fibrosis, which would strengthen the wall Diodrast remained within the sac for over a or obliterate the sac. That pressure can be minute, and, in the same patient, angiog- reduced effectively in the internal carotid raphy performed one week after partial artery by proximal internal or common ca- occlusion of the common carotid by a tan- rotid occlusion has been substantiated amply talum clip showed no filling of the aneurysm. by the works of many authors. However, Aneurysms may decrease visibly in size or pressure reductions distal to the bifurcation become progressively thrombosed after ca- of the internal carotid artery following ca- rotid ligation. -

Peripheral Arterial Disease
SEMINAR Seminar Peripheral arterial disease Kenneth Ouriel Lower extremity peripheral arterial disease (PAD) most frequently presents with pain during ambulation, which is known as “intermittent claudication”. Some relief of symptoms is possible with exercise, pharmacotherapy, and cessation of smoking. The risk of limb-loss is overshadowed by the risk of mortality from coexistent coronary artery and cerebrovascular atherosclerosis. Primary therapy should be directed at treating the generalised atherosclerotic process, managing lipids, blood sugar, and blood pressure. By contrast, the risk of limb-loss becomes substantial when there is pain at rest, ischaemic ulceration, or gangrene. Interventions such as balloon angioplasty, stenting, and surgical revascularisation should be considered in these patients with so-called “critical limb ischaemia”. The choice of the intervention is dependent on the anatomy of the stenotic or occlusive lesion; percutaneous interventions are appropriate when the lesion is focal and short but longer lesions must be treated with surgical revascularisation to achieve acceptable long-term outcome. Peripheral arterial disease (PAD) comprises those entities ankle systolic pressure measured with a blood pressure at which result in obstruction to blood flow in the arteries, the malleolar level by the higher of the two brachial exclusive of the coronary and intracranial vessels. pressures. Defining PAD by an ankle-brachial index of Although the definition of PAD technically includes less than 0·95, a frequency of 6·9% was observed in problems within the extracranial carotid circulation, the patients aged 45–74 years, only 22% of whom had upper extremity arteries, and the mesenteric and renal symptoms.5 The frequency of intermittent claudication circulation, we will focus on chronic arterial occlusive increases dramatically with advancing age, ranging from disease in the arteries to the legs. -

Hypertension and Coronary Heart Disease
Journal of Human Hypertension (2002) 16 (Suppl 1), S61–S63 2002 Nature Publishing Group All rights reserved 0950-9240/02 $25.00 www.nature.com/jhh Hypertension and coronary heart disease E Escobar University of Chile, Santiago, Chile The association of hypertension and coronary heart atherosclerosis, damage of arterial territories other than disease is a frequent one. There are several patho- the coronary one, and of the extension and severity of physiologic mechanisms which link both diseases. coronary artery involvement. It is important to empha- Hypertension induces endothelial dysfunction, exacer- sise that complications and mortality of patients suffer- bates the atherosclerotic process and it contributes to ing a myocardial infarction are greater in hypertensive make the atherosclerotic plaque more unstable. Left patients. Treatment should be aimed to achieve optimal ventricular hypertrophy, which is the usual complication values of blood pressure, and all the strategies to treat of hypertension, promotes a decrease of ‘coronary coronary heart disease should be considered on an indi- reserve’ and increases myocardial oxygen demand, vidual basis. both mechanisms contributing to myocardial ischaemia. Journal of Human Hypertension (2002) 16 (Suppl 1), S61– From a clinical point of view hypertensive patients S63. DOI: 10.1038/sj/jhh/1001345 should have a complete evaluation of risk factors for Keywords: hypertension; hypertrophy; coronary heart disease There is a strong and frequent association between arterial hypertension.8 Hypertension is frequently arterial hypertension and coronary heart disease associated to metabolic disorders, such as insulin (CHD). In the PROCAM study, in men between 40 resistance with hyperinsulinaemia and dyslipidae- and 66 years of age, the prevalence of hypertension mia, which are additional risk factors of atheroscler- in patients who had a myocardial infarction was osis.9 14/1000 men in a follow-up of 4 years. -

Peripheral Arterial Disease
Peripheral arterial disease (Poor blood supply) Information sheet What is it? Peripheral arterial disease (PAD) is the narrowing of one or more arteries (blood vessels). It affects arteries that take blood to the legs, reducing the oxygen that gets to the foot that helps keep the tissues healthy. Also known as 'peripheral vascular disease' and sometimes called 'hardening of the arteries'. What causes it? The narrowing of the arteries is caused by atheroma. Atheroma is like fatty patches or 'plaques' that develop inside the lining of arteries. A patch of atheroma starts quite small, and causes no problems at first. Over the years it can thicken up and start to affect the blood flow through the arteries. (It is a bit like limescale that forms on the inside of water pipes). What are the symptoms? The typical symptom is like a ‘cramping’ sensation in the calves when walking a short distance. It is called 'intermittent claudication'. The pain is relieved when you stop walking. In more serious cases, cramp can be felt in the calf muscles during rest and at night. How can I help prevent it? The best way to help prevent this is to: Stop smoking Exercise regularly Maintain a healthy weight Eat a healthy diet Limit the amount of alcohol you drink (Contact your practice nurse for any further advice on the above) Take care of your feet www.oxleas.nhs.uk How do I take care of my feet? Try not to injure your feet as this can lead to an ulcer or infection developing more easily if the blood supply to the feet is reduced. -

Left Atheroma Mass and Occurrence Out-Of-Office Hypertension in an Extensive Population Raimondo Thomas*
Editorial iMedPub Journals Journal of Cardiovascular Medicine and Therapy 2021 www.imedpub.com Vol.4 No.1:e001 Left Atheroma Mass and Occurrence Out-of-Office Hypertension in an Extensive Population Raimondo Thomas* Department of Cardiology, Alfaisal University, Riyadh, Saudi Arabia *Corresponding author: Thomas R, Department of Cardiology, Alfaisal University, Riyadh, Saudi Arabia, E-mail: [email protected] Received date: February 01, 2021; Accepted date: February 15, 2021; Published date: February 22, 2021 Citation: Thomas R (2021) Left Atheroma Mass and Occurrence out- - of Office Hypertension in an Extensive Population. J Cardiovasc Med Ther Vol.4 No.1: e001 supplementation, physical activity, reduced alcohol consumption, and low-fat diets rich in fruits and vegetables have Abstract been effective in lowering BP and avert hypertension. Hypertension is an important risk factor for the development of cardiovascular disease, and is a major cause Discussion of morbidity and mortality worldwide. Traditionally, The current array of drug and nondrug therapeutic options hypertension diagnosis and treatment and clinical permit for control of hypertension to currently recommended evaluations of antihypertensive efficacy have been based on office blood pressure (BP) measurements; however, there is goal BP levels in all but the rarest patient and supply the increasing evidence that office measures may provide capacity to decrease BP to levels much lower than current inadequate or misleading estimates of a patient’s true BP guidelines recommend. Despite this capability, the vast majority status and level of cardiovascular risk. The introduction, and of patients with hypertension worldwide are untreated or badly endorsement by treatment guidelines, of 24-hour treated. -

SIGN Guideline No 89
89 SIGN Scottish Intercollegiate Guidelines Network Diagnosis and management of 89 peripheral arterial disease A national clinical guideline 1 Introduction 1 2 Cardiovascular risk reduction 3 3 Referral, diagnosis and investigation 7 4 Treatment of symptoms 13 5 Follow up 19 6 Information for discussion with patients and carers 21 7 Development of the guideline 23 8 Implementation, audit and resource implications 26 Abbreviations 28 Annexes 29 References 34 October 2006 COPIES OF ALL sign GUIDELINES ARE AVAILABLE ONLINE AT WWW.SIGN.AC.UK KEY to eVIDENCe statements anD graDes of reCOMMENDATIONS LEVels of eVIDENCE 1++ High quality meta-analyses, systematic reviews of randomised controlled trials (RCTs), or RCTs with a very low risk of bias 1+ Well conducted meta-analyses, systematic reviews of RCTs, or RCTs with a low risk of bias 1 - Meta-analyses, systematic reviews of RCTs, or RCTs with a high risk of bias 2++ High quality systematic reviews of case control or cohort studies High quality case control or cohort studies with a very low risk of confounding or bias and a high probability that the relationship is causal 2+ Well conducted case control or cohort studies with a low risk of confounding or bias and a moderate probability that the relationship is causal 2 - Case control or cohort studies with a high risk of confounding or bias and a significant risk that the relationship is not causal 3 Non-analytic studies, eg case reports, case series 4 Expert opinion GRADES OF RECOMMENDATION Note: The grade of recommendation relates to the strength of the evidence on which the recommendation is based. -

Risk Factors in Abdominal Aortic Aneurysm and Aortoiliac Occlusive
OPEN Risk factors in abdominal aortic SUBJECT AREAS: aneurysm and aortoiliac occlusive PHYSICAL EXAMINATION RISK FACTORS disease and differences between them in AORTIC DISEASES LIFESTYLE MODIFICATION the Polish population Joanna Miko ajczyk-Stecyna1, Aleksandra Korcz1, Marcin Gabriel2, Katarzyna Pawlaczyk3, Received Grzegorz Oszkinis2 & Ryszard S omski1,4 1 November 2013 Accepted 1Institute of Human Genetics, Polish Academy of Sciences, Poznan, 60-479, Poland, 2Department of Vascular Surgery, Poznan 18 November 2013 University of Medical Sciences, Poznan, 61-848, Poland, 3Department of Hypertension, Internal Medicine, and Vascular Diseases, Poznan University of Medical Sciences, Poznan, 61-848, Poland, 4Department of Biochemistry and Biotechnology of the Poznan Published University of Life Sciences, Poznan, 60-632, Poland. 18 December 2013 Abdominal aortic aneurysm (AAA) and aortoiliac occlusive disease (AIOD) are multifactorial vascular Correspondence and disorders caused by complex genetic and environmental factors. The purpose of this study was to define risk factors of AAA and AIOD in the Polish population and indicate differences between diseases. requests for materials should be addressed to J.M.-S. he total of 324 patients affected by AAA and 328 patients affected by AIOD was included. Previously (joannastecyna@wp. published population groups were treated as references. AAA and AIOD risk factors among the Polish pl) T population comprised: male gender, advanced age, myocardial infarction, diabetes type II and tobacco smoking. This study allowed defining risk factors of AAA and AIOD in the Polish population and could help to develop diagnosis and prevention. Characteristics of AAA and AIOD subjects carried out according to clinical data described studied disorders as separate diseases in spite of shearing common localization and some risk factors. -

Association Between Multi-Site Atherosclerotic Plaques and Systemic Arteriosclerosis
Association between multi-site atherosclerotic plaques and systemic arteriosclerosis: results from the BEST study (Beijing Vascular Disease Patients Evaluation Study) huan liu Peking University Shougang Hospital https://orcid.org/0000-0001-6223-7677 Jinbo Liu Peking University Shougang Hospital Wei Huang Peking University Shougang Hospital Hongwei Zhao Peking University Shougang Hospital Na zhao Peking University Shougang Hospital Hongyu wang ( [email protected] ) Research Keywords: arteriosclerosis, atherosclerosis, atherosclerotic plaque, carotid femoral artery pulse wave velocity CF-PWV Posted Date: June 8th, 2020 DOI: https://doi.org/10.21203/rs.3.rs-31641/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Version of Record: A version of this preprint was published on August 1st, 2020. See the published version at https://doi.org/10.1186/s12947-020-00212-3. Page 1/18 Abstract Background Arteriosclerosis can be reected in various aspect of the artery, including atherosclerotic plaque formation or stiffening on the arterial wall. Both arteriosclerosis and atherosclerosis are important and closely associated with cardiovascular disease (CVD). The aim of the study was to evaluate the association between systemic arteriosclerosis and multi-site atherosclerotic plaques. Methods The study was designed as an observational cross-sectional study. A total of 1178 participants (mean age 67.4 years; 52.2% male) enrolled into the observational study from 2010 to 2017. Systemic arteriosclerosis was assessed by carotid femoral artery pulse wave velocity (CF-PWV) and multi-site atherosclerotic plaques (MAP, >=2 of the below sites) were reected in the carotid or subclavian artery, abdominal aorta and lower extremities arteries using ultrasound equipment. -

Arterial Thrombosis and Accelerated Atheroma in a Member of a Family with Familial Antithrombin III Deficiency J
Postgrad Med J: first published as 10.1136/pgmj.58.676.108 on 1 February 1982. Downloaded from Postgraduate Medical Journal (February 1982) 58, 108-109 Arterial thrombosis and accelerated atheroma in a member of a family with familial antithrombin III deficiency J. WINTER D. DONALD B.Sc., M.B., Ch.B., M.R.C.P. M.B., M.R.C.Path. B. BENNETT A. S. DOUGLAS M.D., M.R.C.P. M.D., D.Sc., F.R.C.P. Departments ofMedicine and Pathology, University ofAberdeen, Aberdeen Royal Infirmary, Foresterhill, Aberdeen AB9 2ZB Summary cigarette smoker. After his death, his mother, 4 of his The case is described of a young man with probable siblings and others in his family were found to have familial antithrombin III deficiency, a disorder ATIII deficiency and have been described previously associated with a marked predisposition to venous (Mackie et al., 1978). thrombo-embolic events. In addition to a history of Protected by copyright. venous thrombosis and pulmonary embolism, at Post-mortem findings post-mortem this patient demonstrated widespread The upper half of the body was deeply jaundiced, arterial thrombosis and atheroma. The probable the lower half paler. association of severe arterial thrombosis and atheroma Heart: Both ventricles were enlarged, 2 areas of with a clearly definable coagulation disorder pre- healed infarction were present, the mitral valve was disposing to thrombosis is of interest. sclerosed and incompetent, the aortic valve sclerosed and stenosed. Introduction Arteries: There was extensive atheroma of the Antithrombin III (ATIII) is the major physio- aorta and vessels arising from it including the logical inhibitor of the coagulation mechanism coronary arteries. -

Prehypertension Increases the Risk for Renal Arteriosclerosis in Autopsies: the Hisayama Study
JASN Express. Published on June 20, 2007 as doi: 10.1681/ASN.2007010067 CLINICAL EPIDEMIOLOGY www.jasn.org Prehypertension Increases the Risk for Renal Arteriosclerosis in Autopsies: The Hisayama Study Toshiharu Ninomiya,* Michiaki Kubo,* Yasufumi Doi,† Koji Yonemoto,* Yumihiro Tanizaki,* Kazuhiko Tsuruya,† Katsuo Sueishi,‡ Masazumi Tsuneyoshi,§ Mitsuo Iida,† and Yutaka Kiyohara* Departments of *Environmental Medicine, †Medicine and Clinical Science, ‡Pathophysiological and Experimental Pathology, and §Anatomic Pathology, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan ABSTRACT Information regarding the association between prehypertension BP level and renal arteriosclerosis is limited. In 652 consecutive population-based autopsy samples without hypertension treatment before death, the relationship between the severity of renal arteriosclerosis and BP levels classified according to the criteria of the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure was examined. The age- and gender-adjusted frequencies of renal arteriosclerosis linearly increased with elevating BP levels; both hypertensive and prehypertensive subjects had significantly higher frequencies of renal arteriosclerosis than subjects with normal BP (normal 11.9%; prehypertension 28.5%; stage 1 hypertension 32.9%; stage 2 hypertension 58.2%; all P Ͻ 0.01 versus normal). In a logistic regression model, prehypertension was significantly associated with renal arteriosclerosis after adjustment for other cardiovascular risk factors (prehyper- tension multivariate-adjusted odds ratio [mOR] 5.99 [95% confidence interval (CI) 2.20 to 15.97]; stage 1 hypertension mOR 6.99 [95% CI 2.61 to 18.72]; stage 2 hypertension mOR 22.21 [95% CI 8.35 to 59.08]). This significant association was observed for all renal arterial sizes. -
Pvd-Vs-Pad.Pdf
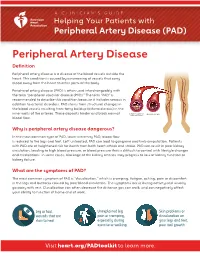
A CLINICIAN'S GUIDE Helping Your Patients with Peripheral Artery Disease (PAD) Peripheral Artery Disease Definition Peripheral artery disease is a disease of the blood vessels outside the heart. This condition is caused by a narrowing of vessels that carry blood away from the heart to other parts of the body. Peripheral artery disease (PAD) is often used interchangeably with the term “peripheral vascular disease (PVD).” The term “PAD” is recommended to describe this condition because it includes venous in addition to arterial disorders. PAD stems from structural changes in the blood vessels resulting from fatty buildup (atherosclerosis) in the inner walls of the arteries. These deposits hinder and block normal blood flow. Why is peripheral artery disease dangerous? In the most common type of PAD, lower extremity PAD, blood flow is reduced to the legs and feet. Left untreated, PAD can lead to gangrene and limb amputation. Patients with PAD are at heightened risk for death from both heart attack and stroke. PAD can result in poor kidney circulation, leading to high blood pressure, or blood pressure that is difficult to control with lifestyle changes and medications. In some cases, blockage of the kidney arteries may progress to loss of kidney function or kidney failure. What are the symptoms of PAD? The most common symptom of PAD is “claudication,” which is cramping, fatigue, aching, pain or discomfort in the legs and buttocks caused by poor blood circulation. The symptoms occur during activity and usually go away with rest. Claudication can often decrease the distance you can walk, and can negatively affect your ability to function at home and at work.