Detection and Dynamic Changes of EGFR Mutations from Circulating
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Engaging with the Trans-East Asian Cultural Tradition in Modern Chinese, Japanese, Korean, and Taiwanese Literatures, 1880S-1940S
Afterlives of the Culture: Engaging with the Trans-East Asian Cultural Tradition in Modern Chinese, Japanese, Korean, and Taiwanese Literatures, 1880s-1940s The Harvard community has made this article openly available. Please share how this access benefits you. Your story matters Citation Hashimoto, Satoru. 2014. Afterlives of the Culture: Engaging with the Trans-East Asian Cultural Tradition in Modern Chinese, Japanese, Korean, and Taiwanese Literatures, 1880s-1940s. Doctoral dissertation, Harvard University. Citable link http://nrs.harvard.edu/urn-3:HUL.InstRepos:13064962 Terms of Use This article was downloaded from Harvard University’s DASH repository, and is made available under the terms and conditions applicable to Other Posted Material, as set forth at http:// nrs.harvard.edu/urn-3:HUL.InstRepos:dash.current.terms-of- use#LAA Afterlives of the Culture: Engaging with the Trans-East Asian Cultural Tradition in Modern Chinese, Japanese, Korean, and Taiwanese Literatures, 1880s-1940s A dissertation presented by Satoru Hashimoto to The Department of East Asian Languages and Civilizations in partial fulfillment of the requirements for the degree of Doctor of Philosophy in the subject of East Asian Languages and Civilizations Harvard University Cambridge, Massachusetts August 2014 ! ! © 2014 Satoru Hashimoto All rights reserved. ! ! Dissertation Advisor: Professor David Der-Wei Wang Satoru Hashimoto Afterlives of the Culture: Engaging with the Trans-East Asian Cultural Tradition in Modern Chinese, Japanese, Korean, and Taiwanese Literatures, 1880s-1940s Abstract This dissertation examines how modern literature in China, Japan, Korea, and Taiwan in the late-nineteenth to the early-twentieth centuries was practiced within contexts of these countries’ deeply interrelated literary traditions. -
Lin Shen *, Yi-Long Wu *, Ying Yuan , Yuxian Bai , Qingyuan Zhang , Qing Zhou , Tianshu Liu , Jun Zhao , Siyang Wang , Xiaoming
SAFETY AND EFFICACY OF LONG-TERM EXPOSURE (LTE) TO TISLELIZUMAB IN CHINESE PATIENTS WITH ADVANCED SOLID TUMORS Lin Shen1*, Yi-Long Wu2*, Ying Yuan3, Yuxian Bai4, Qingyuan Zhang4, Qing Zhou2, Tianshu Liu5, Jun Zhao1, Siyang Wang6, Xiaoming Huang7, Hongming Pan8, Aiping Zhou9, Ting Sun10, Jie Wang9, Yujuan Gao11, Silu Yang11, Yanjun Li11, Juan Zhang11, Jun Guo1 1Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education/Beijing), Peking University Cancer Hospital & Institute, Beijing, China; 2Guangdong Lung Cancer Institute, Guangdong Provincial People’s Hospital and Guangdong Academy of Medical Sciences, Guangzhou, China; 3The Second Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, China; 4Harbin Medical University Cancer Hospital, Harbin, China; 5Zhongshan Hospital, Fudan University, Shanghai, China; 6The Fifth Affiliated Hospital of Sun Yat-Sen University, Zhuhai, China; 7Sun Yat-Sen Memorial Hospital, Sun Yat-Sen University, Guangzhou, China; 8Sir Run Run Shaw Hospital, Zhejiang University School of Medicine, Hangzhou, China; 9Tumor Hospital of Chinese Medical Science Institute, Beijing, China; Poster: 522P 10The First Affiliated Hospital of Nanchang University, Nanchang, China; 11BeiGene (Beijing) Co., Ltd., Beijing, China European Society of Medical Oncology *Contributed equally September 19-21, 2020, Virtual Congress Table 1: Demographics and Baseline Characteristics (ITT Analysis Set) Tumor reductions were reported regardless of PD-L1 expression status or number Continued tumor reduction -

Celebrate Dragon Boat Festival with Michelin-Starred Exclusive Handmade Abalone Sticky Rice Dumpling
April 2019 Celebrate Dragon Boat Festival With Michelin-starred Exclusive Handmade Abalone Sticky Rice Dumpling Celebrate Dragon Boat Festival with a sumptuous interpretation of the classic Hong Kong style sticky rice dumpling, hand crafted by The Peninsula Shanghai’s Michelin-starred culinary team. Back in popular demand following its introduction in 2018, The Peninsula Shanghai exclusive handmade abalone sticky rice dumpling is an authentic rendition of Hong Kong classic prepared with world-class gastronomic techniques. The exclusive handmade abalone sticky rice dumpling is a triumph of Chef Tony Chan of two Michelin-starred Cantonese restaurant Yi Long Court. With over 20 years in the industry, Chef Chan combines an intimate knowledge of his ancestral cuisine and the superlative standards of luxury gastronomy to reimagine timeless dishes that epitomize culinary heritage of Hong Kong and southern China. Each exclusive handmade abalone sticky rice dumpling is crafted with premium, hand-selected ingredients to guarantee the essence of flavour and fragrance stipulated by the key principles of Hong Kong cuisine. The robust flavours of pork belly and dried scallop, free-range salted egg yolk and are combined with the earthiness of mushrooms, sweetness of Chinese chestnut and sweetness of fresh lotus seed and shelled mung beans. Each dumpling is crowned with four premium quality dried abalone – a distinguished Hong Kong delicacy. Cradled within a body of delicately perfumed Chinese glutinous rice and preserved in an aromatic lotus and bamboo leaf wrap, each artfully constructed Yi Long Court exclusive handmade abalone sticky rice dumpling is a symphony of flavour and aromas. Traditional handmade abalone sticky rice dumpling with two premium quality dried abalone will also be available to cater for larger parties and banquets featuring an already abundant array of rich festive dishes and Cantonese delicacies. -

“The Eight Loves of the Peninsula Shanghai” Lets Guests Rediscover the Distinctive Cuisine, Activities, Culture and Community of Their Home Away from Home
FOR IMMEDIATE RELEASE 2 June 2020 The Peninsula Shanghai Launches “We Meet Again” - A Unique Staycation and Guest Experience Programme A celebration of “The Eight Loves of The Peninsula Shanghai” lets guests rediscover the distinctive cuisine, activities, culture and community of their home away from home Guests contribute to the love and support for the Shanghai community with a one-for-one pack food donation programme For nearly a century, The Peninsula Hotels has been more than a global leader in luxury hospitality; the hotels have also been cherished second homes for guests, employees and the larger communities where they are located. That’s why, as the pandemic crisis shows signs of improving and people around the world ease back into their favourite routines, The Peninsula Hotels is extending a warm invitation to residents, with the new “We Meet Again” campaign. The Eight Loves of The Peninsula Shanghai The first pillar of the campaign is a collection of special experiences that celebrate “The Eight Loves of The Peninsula Hotels” – food and drink, art, fashion and culture, exploration, transport, wellness, entertainment, and community – through which The Peninsula family excitedly anticipates a joyful reunion with the families of its guests. The “Eight Loves of The Peninsula Shanghai” experiential programmes begin on 1 June, 2020 and will continue through 30 December 2020. Guests can enjoy special room-rate packages, along with an array of curated experiences that let them enjoy the best of Shanghai and the unparalleled and heart-warming service of The Peninsula Hotels. The Peninsula is the ideal destination for restorative comfort and the creation of precious memories, and for enjoying special time with friends and family, a long-overdue holiday, or a celebration of missed milestones. -

How Zhang Juzheng Dominated China, 1572‒82
Ideas, Determination, Power: How Zhang Juzheng Dominated China, 1572–82 Handwritten pencil manuscript on scrap paper, left unfinished by John W. Dardess. Transcribed by Bruce M. Tindall Edited (lightly) by Sarah Schneewind and Bruce M. Tindall © The Estate of John W. Dardess, 2021 The ms. and notes have been deposited with the library of the University of Kansas. The ms. contains many long paraphrases and quotations, the two not always clearly distinguished. Generally, unless we are sure that the passage is a direct quotation, we have marked it as “in paraphrase.” Researchers wishing to quote should consult the original passages. Numbers in curly brackets { } show where a new page of the handwritten ms. begins, but many complications (backs of pages, interpolated additions, etc.) are not noted. We have reorganized silently where needed, and added section headings. We have silently corrected where it leaves the sense unchanged; other additions, as well as question marks showing that we cannot quite read a word, are in square brackets [ ]. Square brackets also mark words we could not read at all. In the notes, we silently filled in information where certain of the reference. Abstract: Zhang Juzheng (1525-1582) was psychologically the most complex of Ming China’s chief grand secretaries. His rise owed something to an appealing combination of brilliance with diffidence and humility. He was learned, and mastered the literary arts of memorization, comprehension, and interpretation, and the articulation of these things in a clear and creative way in writing. But learning, for Zhang, was never enough. One’s learning, if thoroughly and conscientiously come by, must somehow find its appropriate impact and end in the rectified governance of a realm that after functioning in a faltering way for two centuries had developed some very serious problems. -

A Consensus on Immunotherapy from the 2017 Chinese Lung Cancer Summit Expert Panel
428-436 Guideline A consensus on immunotherapy from the 2017 Chinese Lung Cancer Summit expert panel Yi-Long Wu1, Chang-Li Wang2, Mei-Lin Liao3, Zhong-Zhen Guan4, Chen-Yan Gao5, Shun Lu3, Ming- Fang Zhao6, Jie Wang7, Xiao-Qing Liu8, Jin-Ji Yang1, Jun Liang9, Wei-Min Mao10, Bao-Hui Han3, Xu- Chao Zhang1, Yong Song11, Ji-Feng Feng12, Sheng-Lin Ma13, Gang Wu14, Cai-Cun Zhou15, Ke-Neng Chen16, Ying Cheng17, Yong He18, Chun Chen19, Qun Wang20, Ji-Zhen Lin21, Bo Zhu22, Yun-Peng Liu6, Yi Hu23, Gui-Bin Qiao24, Qing Zhou1, Qi-Bin Song25, Nan Wu16, Lin Wu26, Cheng Huang27, Xiao-Long Fu3, Jian-Ping Xiong28, Jie Hu20, Cheng-Ping Hu29, Jian-Hua Chang30, Qiong Zhao31, Jun Zhao16, Peng- Hui Zhou4, Zhi-Yong Ma32, Yuan Chen33, He-Long Zhang34, Fan Yang35, Jian-Jun Wang14, Yue-Yin Pan36, Xue-Ning Yang1, Yun Fan10, Zhe Liu37, Wen Fan30, Nong Yang26, Yan-Fang Guan38, Hao Sun1, Wen-Zhao Zhong1 1Guangdong Lung Cancer Institute, Guangdong General Hospital and Guangdong Academy of Medical Sciences, Guangzhou 510080, China; 2Department of Lung Cancer, Tianjin Medical University Cancer Institute and Hospital, Tianjin 300060, China; 3Department of Shanghai Lung Cancer Center, Shanghai Chest Hospital, Shanghai Jiaotong University, Shanghai 200240, China; 4Sun Yat-sen University Cancer Center, Guangzhou 510030, China; 5Center for Food and Drug Inspection of China Food and Drug Administration, 6Department of Medical Oncology, The First Hospital of China Medical University, Shenyang 110001, China; 7Department of Medical Oncology, National Cancer Center/Cancer Hospital, -

Alternative Titles Index
VHD Index - 02 9/29/04 4:43 PM Page 715 Alternative Titles Index While it's true that we couldn't include every Asian cult flick in this slim little vol- ume—heck, there's dozens being dug out of vaults and slapped onto video as you read this—the one you're looking for just might be in here under a title you didn't know about. Most of these films have been released under more than one title, and while we've done our best to use the one that's most likely to be familiar, that doesn't guarantee you aren't trying to find Crippled Avengers and don't know we've got it as The Return of the 5 Deadly Venoms. And so, we've gathered as many alternative titles as we can find, including their original language title(s), and arranged them in alphabetical order in this index to help you out. Remember, English language articles ("a", "an", "the") are ignored in the sort, but foreign articles are NOT ignored. Hey, my Japanese is a little rusty, and some languages just don't have articles. A Fei Zheng Chuan Aau Chin Adventure of Gargan- Ai Shang Wo Ba An Zhan See Days of Being Wild See Running out of tuas See Gimme Gimme See Running out of (1990) Time (1999) See War of the Gargan- (2001) Time (1999) tuas (1966) A Foo Aau Chin 2 Ai Yu Cheng An Zhan 2 See A Fighter’s Blues See Running out of Adventure of Shaolin See A War Named See Running out of (2000) Time 2 (2001) See Five Elements of Desire (2000) Time 2 (2001) Kung Fu (1978) A Gai Waak Ang Kwong Ang Aau Dut Air Battle of the Big See Project A (1983) Kwong Ying Ji Dut See The Longest Nite The Adventures of Cha- Monsters: Gamera vs. -
The Dreaming Mind and the End of the Ming World
The Dreaming Mind and the End of the Ming World The Dreaming Mind and the End of the Ming World • Lynn A. Struve University of Hawai‘i Press Honolulu © 2019 University of Hawai‘i Press This content is licensed under the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International license (CC BY-NC-ND 4.0), which means that it may be freely downloaded and shared in digital format for non-commercial purposes, provided credit is given to the author. Commercial uses and the publication of any derivative works require permission from the publisher. For details, see https://creativecommons.org/licenses/by-nc-nd/4.0/. The Creative Commons license described above does not apply to any material that is separately copyrighted. The open-access version of this book was made possible in part by an award from the James P. Geiss and Margaret Y. Hsu Foundation. Cover art: Woodblock illustration by Chen Hongshou from the 1639 edition of Story of the Western Wing. Student Zhang lies asleep in an inn, reclining against a bed frame. His anxious dream of Oriole in the wilds, being confronted by a military commander, completely fills the balloon to the right. In memory of Professor Liu Wenying (1939–2005), an open-minded, visionary scholar and open-hearted, generous man Contents Acknowledgments • ix Introduction • 1 Chapter 1 Continuities in the Dream Lives of Ming Intellectuals • 15 Chapter 2 Sources of Special Dream Salience in Late Ming • 81 Chapter 3 Crisis Dreaming • 165 Chapter 4 Dream-Coping in the Aftermath • 199 Epilogue: Beyond the Arc • 243 Works Cited • 259 Glossary-Index • 305 vii Acknowledgments I AM MOST GRATEFUL, as ever, to Diana Wenling Liu, head of the East Asian Col- lection at Indiana University, who, over many years, has never failed to cheerfully, courteously, and diligently respond to my innumerable requests for problematic materials, puzzlements over illegible or unfindable characters, frustrations with dig- ital databases, communications with publishers and repositories in China, etcetera ad infinitum. -

Acknowledgements to Reviewers
Acta Pharmacologica Sinica (2020) 41: i–iv © 2020 CPS and SIMM All rights reserved 1671-4083/20 www.nature.com/aps Acknowledgements to Reviewers The Editorial Board of the Acta Pharmacologica Sinica wishes to thank the following scientists for their unique contribution to this journal in reviewing the papers from November 1, 2019 to October 31, 2020 (including papers published and rejected). AA, Ji-ye (Nanjing) CHEN, Hong-guang (Tianjin) DAI, Hou-yong (Nanjing) ACCORNERO, Federica (Columbus) CHEN, Hou-zao (Beijing) DAI, Mei (Cincinnati) ALOBAID, Abdulaziz S (Riyadh) CHEN, Hsin-Hung (Tainan) DAI, Min (Hefei) ARAYA, Jun (Minato-ku) CHEN, Jing (Jining) DAI, Xiao-yan (Guangzhou) ARIGA, Hiroyoshi (Sapporo) CHEN, Jing (Shanghai) DAI, Yue (Nanjing) ARIYOSHI, Wataru (Kitakyushu) CHEN, Jun (Shanghai) DANG, Yong-jun (Shanghai) ASTOLFI, Andrea (Perugia) CHEN, Jun (Tianjin) DAS, Archita (Augusta) BAI, Li-Yuan (Taichung) CHEN, Kun-qi (Suzhou) DAY, Regina M (Bethesda) BAI, Xiaowen (Milwaukee) CHEN, Nai-hong (Beijing) DE GEEST, Bruno (Ghent) BAN, Tao (Harbin) CHEN, Peng (Guangzhou) DENG, Xian-ming (Xiamen) BANERJEE, D (Chandigarh) CHEN, Qiu-yun (Zhenjiang) DENG, Xiao-yong (Shanghai) BAO, Jin-ku (Chengdu) CHEN, Rui-zhen (Shanghai) DENG, Xu-ming (Changchun) BAO, Mei-hua (Changsha) CHEN, Shuai-shuai (Linhai) DENG, Yi-lun (San Antonio) BAO, Yu-qian (Shanghai) CHEN, Shu-zhen (Beijing) DING, Fei (Nantong) BARTON, Samantha (Parkville) CHEN, Tian-feng (Guangzhou) DING, Jin-song (Changsha) BAY, Boon Huat (Singapore) CHEN, Wan-jin (Fuzhou) DING, Jun-jie (Shanghai) -
A Scalable Limited Feedback Design for Network MIMO Using Per-Cell
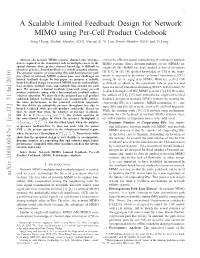
1 A Scalable Limited Feedback Design for Network MIMO using Per-Cell Product Codebook Yong Cheng, Student Member, IEEE, Vincent K. N. Lau, Senior Member, IEEE, and Yi Long Abstract—In network MIMO systems, channel state informa- critical for efficient spatial multiplexing of mobiles in network tion is required at the transmitter side to multiplex users in the MIMO systems. Space division multiple access (SDMA) for spatial domain. Since perfect channel knowledge is difficult to single-cell MU-MIMO has been studied in lots of literatures obtain in practice, limited feedback is a widely accepted solution. The dynamic number of cooperating BSs and heterogeneous path [5]–[11]. In [5], [6], perfect knowledge of CSI at the trans- loss effects of network MIMO systems pose new challenges on mitter is assumed to eliminate cochannel interference (CCI) limited feedback design. In this paper, we propose a scalable among the users engaged in SDMA. However, perfect CSI limited feedback design for network MIMO systems with multiple is difficult to obtain at the transmitter side in practice and base stations, multiple users and multiple data streams for each there are lots of literatures discussing SDMA with limited CSI user. We propose a limited feedback framework using per-cell product codebooks, along with a low-complexity feedback indices feedback in single-cell MU-MIMO systems [7]–[13]. Recently, selection algorithm. We show that the proposed per-cell product the authors of [14], [15] have extended the single-cell limited codebook limited feedback design can asymptotically achieve feedback designs to network MIMO systems by treating the the same performance as the joint-cell codebook approach. -

3D Waveform Oscilloscope Implemented on Coupled FPGA-GPU Embedded System
2018 5th International Conference on Information Science and Control Engineering (ICISCE 2018) Zhengzhou, China 20-22 July 2018 Pages 1-653 IEEE Catalog Number: CFP18C46-POD ISBN: 978-1-5386-5501-6 1/2 Copyright © 2018 by the Institute of Electrical and Electronics Engineers, Inc. All Rights Reserved Copyright and Reprint Permissions: Abstracting is permitted with credit to the source. Libraries are permitted to photocopy beyond the limit of U.S. copyright law for private use of patrons those articles in this volume that carry a code at the bottom of the first page, provided the per-copy fee indicated in the code is paid through Copyright Clearance Center, 222 Rosewood Drive, Danvers, MA 01923. For other copying, reprint or republication permission, write to IEEE Copyrights Manager, IEEE Service Center, 445 Hoes Lane, Piscataway, NJ 08854. All rights reserved. *** This is a print representation of what appears in the IEEE Digital Library. Some format issues inherent in the e-media version may also appear in this print version. IEEE Catalog Number: CFP18C46-POD ISBN (Print-On-Demand): 978-1-5386-5501-6 ISBN (Online): 978-1-5386-5500-9 Additional Copies of This Publication Are Available From: Curran Associates, Inc 57 Morehouse Lane Red Hook, NY 12571 USA Phone: (845) 758-0400 Fax: (845) 758-2633 E-mail: [email protected] Web: www.proceedings.com 2018 5th International Conference on Information Science and Control Engineering ICISCE 2018 Table of Contents Message from the ICISCE 2018 General Chairs xxx Message from the ICISCE 2018 -

Tion to This Journal in Reviewing the Papers from July to September in 2007 (Including Papers Published and Rejected)
The Editorial Board of the Acta Pharmacologica Sinica wishes to thank the following scientists for their unique contribu- tion to this journal in reviewing the papers from July to September in 2007 (including papers published and rejected). ALBERT, Philippe (Reims) FANG, Jing-yuan (Shanghai) JI, Yong (Nanjing) ARTALI, R (Milano) FENG, HL (Manhasset) JI, Yong-hua (Shanghai) BA, Xue-qing (Changchun) FENG, Li (Chengdu) JIANG, Jia-hua (Indianapolis) BAGOSSI, Peter (Debrecen) FIMOGNARI, Carmela (Bologna) JIANG, Xian-cheng (Brooklyn) BAI, Dong-lu (Shanghai) FU, Li-wu (Guangzhou) JIANG, Xing-hong (Suzhou) BAKER, John E (Milwaukee) FUCHS, Flavio Danni (Porto Alegre) JIN, Mei-lei (Shanghai) BAO, Yong-ping (Norwich) GABIZON, Alberto Abraham (Jerusalem) JING, Yang (Wuhan) BARANCIK, Miroslav (Bratislava) GAMET-PAYRASTRE, Laurence (Toulouse) JUNZHU, Chen (Hangzhou) BEMEUR, Chantal (Montreal) GAO, Feng (Xi’an) KAGEYAMA, Yukio (Saitama) BENAGIANO, V (Bari) GAO, Xue (College Station) KANG, Ji-an (Valhalla) BERROUGUI, Hicham (SHERBROOKE) GAWRISCH, Klaus (Bethesda) KE, Zun-ji (Shanghai) BIERHAUS, Angelika (Heidelberg) GENG, Mei-yu (Qingdao) KERRAM, Parhat (Urumqi) BIN, Zhou (Tianjin) GONG, Jian-ping (chongqing) KHOR, Tin Oo (Piscataway) BISSONNETTE, Elyse (Ste-Foy) GONZALEZ-AMARO, R (SLP) KIM, Sung-jun (Gwangju) BOISSON-VIDAL, Catherine (Paris) GOWDA, T Veerabasappa (Mysore) KINTSCHER, Ulrich (Berlin) BURDA, J (Kosice) GOWER JR, William R (Tampa) KNADLER, Mary Pat (Indianapolis) CABALLERO, R (Madrid) GU, Jing-kai (Changchun) KRALOVEC, Jaroslav A (Dartnouth)