What You Need to Know About Cataract Treatment
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Visual Outcomes of Combined Cataract Surgery and Minimally Invasive Glaucoma Surgery
1422 REVIEW/UPDATE Visual outcomes of combined cataract surgery and minimally invasive glaucoma surgery Steven R. Sarkisian Jr, MD, Nathan Radcliffe, MD, Paul Harasymowycz, MD, Steven Vold, MD, Thomas Patrianakos, MD, Amy Zhang, MD, Leon Herndon, MD, Jacob Brubaker, MD, Marlene Moster, MD, Brian Francis, MD, for the ASCRS Glaucoma Clinical Committee Minimally invasive glaucoma surgery (MIGS) has become a reliable on visual outcomes based on the literature and the experience of standard of care for the treatment of glaucoma when combined the ASCRS Glaucoma Clinical Committee. with cataract surgery. This review describes the MIGS procedures J Cataract Refract Surg 2020; 46:1422–1432 Copyright © 2020 Published currently combined with and without cataract surgery with a focus by Wolters Kluwer on behalf of ASCRS and ESCRS inimally invasive (sometimes referred to as mi- and thereby lower IOP. The endoscope consists of a fiber- croinvasive) glaucoma surgery (MIGS) is a pro- optic camera, light source, and laser aiming beam with an Mcedure that lowers intraocular pressure (IOP) 832 nm diode laser. The endoscope probe is introduced into without significantly altering the tissue, allows for rapid the globe via a limbal corneal or pars plana incision. The visual recovery, is moderately effective, and can be com- anterior approach requires inflation of the ciliary sulcus with bined with cataract surgery in a safe and efficient manner.1,2 an ophthalmic viscosurgical device, whereas the posterior This is in contrast to more conventional glaucoma surgery approach uses a pars plana or anterior chamber irrigation (eg, trabeculectomy or large glaucoma drainage device port. Although the anterior approach can be used in a phakic implantation), which requires conjunctival and scleral eye, it is typically performed with cataract extraction as a incisions as well as suturing. -

Ocular Surface Disease: Supplement April 2018 Accurately Diagnose & Effectively Treat Your Surgical Patients
Ocular Surface Disease: Supplement April 2018 Accurately Diagnose & Effectively Treat Your Surgical Patients Supported by an unrestricted educational grant from Ocular Surface Disease: Accurately Diagnose & Effectively Treat Your Surgical Patients Prevalence of Ocular Surface Disease and Its Impact on Surgical Outcomes Accurate diagnosis of dry eye disease is critical before cataract or refractive surgery By Elisabeth M. Messmer, MD ry eye is a common disease, but it may remain EPIDEMIOLOGY OF DRY EYE SYNDROME undetected. If it is not treated before cataract or 1-4 refractive surgery, patients may have suboptimal visual AFTER CATARACT SURGERY outcomes from their procedures. D l Very limited data available, mostly small descriptive/ IMPACT ON CATARACT SURGERY non-randomised studies There are a number of triggering factors for dry eye (Figure 1). l 10-20% of patients: DED induced or worsened after Cataract surgery worsens or causes dry eye in approximately uncomplicated cataract surgery 10% to 20% of patients (Figure 2).1-4 l In all studies: Signs and symptoms of dry eye In a study of 136 patients with a mean age of 71 years who increase after surgery were having cataract surgery, 22% had a prior diagnosis of dry eye that was not treated.5 Thirty-one percent complained l In most studies: gradual improvement of signs and of stinging, burning or other symptoms of dry eye when asked symptoms of dry eye within 3 months about their symptoms, and 41% reported a foreign body l In some studies: signs and symptoms persist > 3 months sensation. When the patients were examined, 77% had corneal staining and 50% had central staining. -
Intraocular Lenses and Spectacle Correction
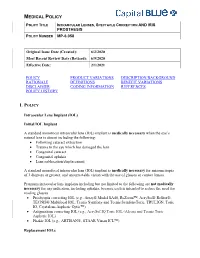
MEDICAL POLICY POLICY TITLE INTRAOCULAR LENSES, SPECTACLE CORRECTION AND IRIS PROSTHESIS POLICY NUMBER MP-6.058 Original Issue Date (Created): 6/2/2020 Most Recent Review Date (Revised): 6/9/2020 Effective Date: 2/1/2021 POLICY PRODUCT VARIATIONS DESCRIPTION/BACKGROUND RATIONALE DEFINITIONS BENEFIT VARIATIONS DISCLAIMER CODING INFORMATION REFERENCES POLICY HISTORY I. POLICY Intraocular Lens Implant (IOL) Initial IOL Implant A standard monofocal intraocular lens (IOL) implant is medically necessary when the eye’s natural lens is absent including the following: Following cataract extraction Trauma to the eye which has damaged the lens Congenital cataract Congenital aphakia Lens subluxation/displacement A standard monofocal intraocular lens (IOL) implant is medically necessary for anisometropia of 3 diopters or greater, and uncorrectable vision with the use of glasses or contact lenses. Premium intraocular lens implants including but not limited to the following are not medically necessary for any indication, including aphakia, because each is intended to reduce the need for reading glasses. Presbyopia correcting IOL (e.g., Array® Model SA40, ReZoom™, AcrySof® ReStor®, TECNIS® Multifocal IOL, Tecnis Symfony and Tecnis SymfonyToric, TRULIGN, Toric IO, Crystalens Aspheric Optic™) Astigmatism correcting IOL (e.g., AcrySof IQ Toric IOL (Alcon) and Tecnis Toric Aspheric IOL) Phakic IOL (e.g., ARTISAN®, STAAR Visian ICL™) Replacement IOLs MEDICAL POLICY POLICY TITLE INTRAOCULAR LENSES, SPECTACLE CORRECTION AND IRIS PROSTHESIS POLICY NUMBER -

Visual Symptoms and Convergence Insufficiency in University Teachers
242ARTIGO ORIGINAL DOI 10.5935/0034-7280.20170050 Sintomas visuais e insuficiência de convergência em docentes universitários Visual symptoms and convergence insufficiency in university teachers Nágila Cristiana Menigite1, Marcelo Taglietti1 RESUMO Objetivo: Investigar a prevalência de desconforto visual e insuficiência de convergência (IC) em docentes universitários. Métodos: Tratar-se de um estudo transversal, com 60 docentes de ambos os sexos, tendo sido utilizado o questionário Convergence Insufficiency Symptom Survey, validado para a população brasileira. Resultados: Dos docentes entrevistados 55,0% eram do sexo feminino. 48,3% responderam dedicar menos que duas horas por dia à leitura, sendo que 40,0% dos entrevistados disseram que fazem pausas de 30 minutos à uma hora durante a leitura e 63,3% afirmaram passar entre 2 a 5 horas por dia em frente ao computador. Em relação à investigação sobre as doenças do sistema visual, 25,0% relataram apresentar miopia, sendo que 55,0% dos indivíduos usam óculos e destes 41,7% o usam com frequência. Quanto à investigação da prevalência de insuficiência de convergência, obteve-se frequência de (1,8) %. Conclusão: Constatou-se que a maioria dos entrevistados se apresentou com desconforto visual e uma pequena porcentagem foram acometidos pela IC. Descritores: Acuidade visual; Transtornos da motilidade ocular; Transtornos da visão; Visão binocular ABSTRACT Objective: To investigate the prevalence of visual discomfort and convergence failure in professors. Methods: A cross-sectional study was done, consisting of 60 teachers of both sexes, of the Centro Universitário FAG, which used the Convergence Insufficiency Symptom Survey, validated for the Brazilian population. Results: Of those surveyed 55.0% are female. -

CAUSES, COMPLICATIONS &TREATMENT of A“RED EYE”
CAUSES, COMPLICATIONS & TREATMENT of a “RED EYE” 8 Most cases of “red eye” seen in general practice are likely to be conjunctivitis or a superficial corneal injury, however, red eye can also indicate a serious eye condition such as acute angle glaucoma, iritis, keratitis or scleritis. Features such as significant pain, photophobia, reduced visual acuity and a unilateral presentation are “red flags” that a sight-threatening condition may be present. In the absence of specialised eye examination equipment, such as a slit lamp, General Practitioners must rely on identifying these key features to know which patients require referral to an Ophthalmologist for further assessment. Is it conjunctivitis or is it something more Iritis is also known as anterior uveitis; posterior uveitis is serious? inflammation of the choroid (choroiditis). Complications include glaucoma, cataract and macular oedema. The most likely cause of a red eye in patients who present to 4. Scleritis is inflammation of the sclera. This is a very rare general practice is conjunctivitis. However, red eye can also be presentation, usually associated with autoimmune a feature of a more serious eye condition, in which a delay in disease, e.g. rheumatoid arthritis. treatment due to a missed diagnosis can result in permanent 5. Penetrating eye injury or embedded foreign body; red visual loss. In addition, the inappropriate use of antibacterial eye is not always a feature topical eye preparations contributes to antimicrobial 6. Acid or alkali burn to the eye resistance. The patient history will usually identify a penetrating eye injury Most general practice clinics will not have access to specialised or chemical burn to the eye, but further assessment may be equipment for eye examination, e.g. -

Contacts Vs. Iols for Congenital Cataract
in Review News commentary and perspectives Contacts vs. IOLs for Congenital Cataract he verdict is in on the issue of optical correction in children who undergo unilateral cataract surgery before age 7 months: Aphakia, corrected with a contact lens, is a better option than an T CONTACT LENS PATIENT. Dr. Lambert examines a 6-year-old intraocular lens (IOL) for 55 others who received an aphakic girl in the IATS trial. This child was prescribed a most of these babies. IOL implant (median VA in contact lens in one eye at 1 month of age and could insert “Primary IOL implan- both groups, 0.90 logMAR her own contact lens by the age 4 years. tation should be reserved [20/159]). for those infants where, in More complications. pillary membranes occurred one normal eye. But the the opinion of the surgeon, However, a significantly 10 times more often in the thing about children is that the cost and handling of greater number of the pseu- pseudophakic eyes. they’re going to live for a a contact lens would be so dophakic eyes required one Scott R. Lambert, MD, very long time, and it is burdensome as to result in or more additional intra- a professor of ophthalmol- important for them to have significant periods of uncor- operative procedures over ogy at Emory University in the best possible visual acu- rected aphakia,” stated the the course of the study (41 Atlanta and the lead inves- ity in their problem eye,” investigators in the Infant patients compared with tigator in the trial, credited he said, particularly in case Aphakia Treatment Study.1 12 in the aphakic group; advocacy by the pediatric anything should happen to Comparable VA. -

Treatment of Stable Keratoconus by Cataract Surgery with Toric IOL Implantation
10.5005/jp-journals-10025-1024 JaimeCASE Levy REPORT et al Treatment of Stable Keratoconus by Cataract Surgery with Toric IOL Implantation Jaime Levy, Anry Pitchkhadze, Tova Lifshitz ABSTRACT implantation in the right eye. On presentation, uncorrected We present the case of a 73-year-old patient who underwent visual acuity (UCVA) was 6/60 OU. Refraction was –0.75 successful phacoemulsification and toric intraocular lens (IOL) –5.0 × 65° OD and –3.25 –4.0 × 98° OS. Nuclear sclerosis implantation to correct high stable astigmatism due to and posterior subcapsular cataract +2 was observed in the keratoconus and cataract. Preoperative refraction was –3.25 – left eye. The posterior segments were unremarkable. 4.0 × 98°. A toric IOL (Acrysof SN60T6) with a spherical power of 16.5 D and a cylinder power of 3.75 D at the IOL plane and Corneal topography performed with Orbscan (Bausch 2.57 D at the corneal plane was implanted and aligned at an and Lomb, Rochester, NY) showed central thinning of 457 axis of 0°. Uncorrected visual acuity improved from 6/60 to microns and positive islands of elevation typical for 6/10. Postoperative best corrected visual acuity was 6/6, 6 months after the operation. In conclusion, phacoemulsification keratoconus in the right eye (Fig. 1). In the left eye a less with toric IOL implantation can be performed in eyes with pronounced inferior cone was observed (Fig. 2), without keratoconus and cataract. any area of significant thinning near the limbus typical for Keywords: Intraocular lens, Toric IOL, Keratoconus, Cataract pellucid marginal degeneration.2 Keratometry (K)-values surgery. -
Directory of Participating Optical Panelists
DIRECTORY OF PARTICIPATING OPTICAL PANELISTS September 2019 WWW.UFTWF.ORG Table of Contents GENERAL INFORMATION ...................................... 2 PARTICIPATING PANELISTS ................................. 7 NEW YORK .............................................................. 7 Manhattan ......................................................... 7 Staten Island ..................................................... 11 Bronx ................................................................. 12 Queens .............................................................. 15 Brooklyn ............................................................ 21 Nassau .............................................................. 28 Suffolk ............................................................... 32 Westchester, Hudson Valley & Upstate NY ........................................................ 34 NEW JERSEY .......................................................... 38 CONNECTICUT ....................................................... 42 FLORIDA .................................................................. 42 SUPPLEMENTAL LISTINGS ................................... 46 A complete listing of providers throughout the U.S. is available on our website: www.uftwf.org 1 General Information DESCRIPTION OF BENEFITS (A complete description is available in our Red Apple or on our website at: www.uftwf.org) PLAN OVERVIEW PARTICIPATING OPTICAL CENTERS Members can use the optical plan once every two (2) years by bringing a validated certificate to any of -

Incidence of Posterior Vitreous Detachment After Cataract Surgery
ARTICLE Incidence of posterior vitreous detachment after cataract surgery Alireza Mirshahi, MD, FEBO, Fabian Hoehn, MD, FEBO, Katrin Lorenz, MD, Lars-Olof Hattenbach, MD PURPOSE: To report the incidence of posterior vitreous detachment (PVD) after uneventful state- of-the-art small-incision phacoemulsification with implantation of a posterior chamber intraocular lens (PC IOL). SETTING: Department of Ophthalmology, Ludwigshafen Hospital, Ludwigshafen, Germany. METHODS: This prospective study evaluated the vitreous status of eyes by biomicroscopic exam- ination, indirect binocular ophthalmoscopy, and B-scan ultrasonography before planned cataract surgery. Patients with the posterior vitreous attached were included for follow-up and examined 1 week, 1 month, and 1 year after uneventful phacoemulsification with PC IOL implantation. The preoperative prevalence and postoperative incidence of PVD were determined by ultrasonography. RESULTS: The study included 188 eyes of 188 patients (131 women, 57 men) with a mean age of 77.2 years. The mean spherical equivalent was À0.78 diopter (D) (range À8.75 to C6.25 D) and the mean axial length (AL), 23.22 mm (range 20.50 to 26.04 mm). Preoperatively, 130 eyes (69.1%) had PVD and 58 eyes (30.9%) had no PVD. Postoperatively, 12 eyes (20.7%) developed PVD at 1 week, 18 eyes (31%) at 1 month, and 4 eyes (6.9%) at 1 year. The vitreous body remained at- tached to the retina in 24 eyes (41.4%) 1 year after surgery. No preoperatively measured parameter (eg, age, refraction, AL, effective phacoemulsification time) was predictive of the occurrence of PVD after cataract surgery. CONCLUSION: The occurrence of PVD after modern cataract surgery was frequent in cases in which the posterior hyaloid was attached to the retinal surface preoperatively. -

Florida Board of Medicine and Florida Board Of
FLORIDA BOARD OF MEDICINE AND FLORIDA BOARD OF OSTEOPATHIC MEDICINE APPROVED INFORMED CONSENT FORM FOR CATARACT OPERATION WITH OR WITHOUT IMPLANTATION OF INTRAOCULAR LENS DOES THE PATIENT NEED OR WANT A TRANSLATOR, INTERPRETOR OR READER? YES _____ NO_____ TO THE PATIENT: You have the right, as a patient, to be informed about your cataract condition and the recommended surgical procedure to be used, so that you may make the decision whether or not to undergo the cataract surgery, after knowing the risks, possible complications, and alternatives involved. This disclosure is not meant to scare or alarm you; it is simply an effort to make you better informed so that you may give or withhold your consent to cataract surgery and should reflect the information provided by your eye surgeon. If you have any questions or do not understand the information, please discuss the procedure with your eye surgeon prior to signing. WHAT IS A CATARACT, AND HOW IS IT TREATED? The lens in the eye can become cloudy and hard, a condition known as a cataract. Cataracts can develop from normal aging, from an eye injury, various medical conditions or if you have taken certain medications such as steroids. Cataracts may cause blurred vision, dulled vision, sensitivity to light and glare, and/or ghost images. If the cataract changes vision so much that it interferes with your daily life, the cataract may need to be removed to try to improve your vision. Surgery is the only way to remove a cataract. You can decide to postpone surgery or not to have the cataract removed. -
The Capsulotomy: from There to Where?
JUNE 2017 # 42 In My View NextGen Profession Sitting Down With Presbyopia correction in Dry eye: how the humble Louis Pasquale believes it’s Innovator extraordinaire, younger patients – what’s best? eyedrop is evolving time to redefine POAG Sean Ianchulev 17 36 – 38 42 – 45 50 – 51 The Capsulotomy: From There to Where? A tale of jealousy, rivalry and pride… The unfolding story of the capsulotomy over time 18 – 27 www.theophthalmologist.com It’s all in CHOOSE A SYSTEM THAT EMPOWERS YOUR EVERY MOVE. Technique is more than just the motions. Purposefully engineered for exceptional versatility and high-quality performance, the WHITESTAR SIGNATURE PRO Phacoemulsification System gives you the clinical flexibility, confidence and control to free your focus for what matters most in each procedure. How do you phaco? Join the conversation. Contact your Phaco Specialist today. Rx Only INDICATIONS: The WHITESTAR SIGNATURE PRO System is a modular ophthalmic microsurgical system that facilitates anterior segment (cataract) surgery. The modular design allows the users to configure the system to meet their surgical requirements. IMPORTANT SAFETY INFORMATION: Risks and complications of cataract surgery may include broken ocular capsule or corneal burn. This device is only to be used by a trained, licensed physician. ATTENTION: Reference the labeling for a complete listing of Indications and Important Safety Information. WHITESTAR SIGNATURE is a trademark owned by or licensed to Abbott Laboratories, its subsidiaries or affiliates. © 2017 Abbott Medical Optics Inc. | PP2017CT0929 Image of the Month In a Micropig’s Eye This Wellcome Image Award winner depicts a 3D model of a healthy mini-pig eye. -

PHILADELPHIA OPHTHALMOLOGY ASSOCIATES So, You Have A
PHILADELPHIA OPHTHALMOLOGY ASSOCIATES So, You Have A Cataract… WHAT IS A CATARACT? Every year the lens in your eye that helps you see gets thicker. In your forties, the lens is thick enough that it doesn’t change its shape well enough to focus on near objects and is referred to as a cataract. So, the day you need reading glasses, (or if you are nearsighted, the day you are forced to take your glasses off to read), is the day you have a cataract by definition. As the cataract becomes denser, you need stronger reading glasses or bifocals. Eventually you feel you are not seeing as well as you used to for viewing things in the distance, reading or doing close work, or for driving at night or in bad weather despite the best glasses. Once this occurs, you become a candidate for cataract surgery. WHAT IS CATARACT SURGERY? Cataract surgery is lens replacement surgery. Before surgery, measurements are made to determine what lens power needs to be placed in your eye to help improve your vision. Special equipment is used in the surgery center to remove the cataract and a new lens is placed in your eye. Today’s technology allows you to choose what type of lens you want implanted. STANDARD – DISTANCE With “Standard” cataract surgery, a monofocal lens is implanted. This means the lens has one focal point (i.e. the lens focuses the eye to see in the distance OR at near for reading but not both). Most people choose to see in the distance.