Study Protocol, Including One Week of Hospitalization/In-Patient Stay
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(12) Patent Application Publication (10) Pub. No.: US 2017/0020892 A1 Thompson Et Al
US 20170020892A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2017/0020892 A1 Thompson et al. (43) Pub. Date: Jan. 26, 2017 (54) USE OF NEGATIVE MODULATORS OF Related U.S. Application Data GABA RECEPTORS CONTAINING ALPHAS SUBUNITS AS FAST ACTING (60) Provisional application No. 61/972,446, filed on Mar. ANTDEPRESSANTS 31, 2014. (71) Applicant: University of Maryland, Baltimore, Publication Classification Baltimore, MD (US) (51) Int. Cl. A 6LX 3/557 (2006.01) (72) Inventors: Scott Thompson, Baltimore, MD (US); A6II 3/53 (2006.01) Mark D. Kvarta, Ellicott City, MD A6II 45/06 (2006.01) (US); Adam Van Dyke, Baltimore, MD (52) U.S. Cl. (US) CPC ........... A61 K3I/55.17 (2013.01); A61K 45/06 (2013.01); A61 K3I/53 (2013.01) (73) Assignee: University of Maryland, Baltimore, Baltimore, MD (US) (57) ABSTRACT Embodiments of the disclosure include methods and com (21) Appl. No.: 15/300,984 positions related to treatment of one or more medical conditions with one or more negative modulators of GABA (22) PCT Filed: Mar. 31, 2015 receptors. In specific embodiments, depression and/or Sui cidability is treated or ameliorated or prevented with one or (86) PCT No.: PCT/US2O15/023667 more negative modulators of GABA receptors, such as a S 371 (c)(1), partial inverse agonist of a GABA receptor comprising an (2) Date: Sep. 30, 2016 alpha5 subunit. Patent Application Publication Jan. 26, 2017. Sheet 1 of 12 US 2017/002O892 A1 ×1/ /|\ Patent Application Publication Jan. 26, 2017. Sheet 3 of 12 US 2017/002O892 A1 & Patent Application Publication Jan. -

Sex Differences in a Transgenic Rat Model of Huntington's Disease
Human Molecular Genetics, 2008, Vol. 17, No. 17 2595–2609 doi:10.1093/hmg/ddn159 Advance Access published on May 23, 2008 Sex differences in a transgenic rat model of Huntington’s disease: decreased 17b-estradiol levels correlate with reduced numbers of DARPP321 neurons in males 1,{ 1,{ 1 1 2 Felix J. Bode , Michael Stephan , Hendrik Suhling , Reinhard Pabst , Rainer H. Straub , Downloaded from https://academic.oup.com/hmg/article-abstract/17/17/2595/632381 by guest on 27 June 2020 Kerstin A. Raber3, Michael Bonin4, Huu Phuc Nguyen4, Olaf Riess4, Andreas Bauer5,6, Charlotte Sjoberg7,A˚ sa Peterse´n7 and Stephan von Ho¨ rsten1,3,Ã 1Institute of Functional and Applied Anatomy, Medical School of Hannover, 30625 Hannover, Germany, 2Department of Internal Medicine I, University Regensburg, 93042 Regensburg, Germany, 3Experimental Therapy, Franz-Penzoldt- Center, Friedrich-Alexander-University Erlangen-Nu¨rnberg, 91054 Erlangen, Germany, 4Department of Medical Genetics, University of Tu¨bingen, 72076 Tu¨bingen, Germany, 5Institute of Neurosciences and Biophysics, Research Centre Juelich, 52425 Juelich, Germany, 6Department of Neurology, Heinrich-Heine University Duesseldorf, 40001 Duesseldorf, Germany and 7Translational Neuroendocrine Research Unit, Department of Experimental Medical Science, Lund University, 22184 Lund, Sweden Received March 10, 2008; Revised May 8, 2008; Accepted May 21, 2008 Recent clinical studies have highlighted that female sex hormones represent potential neuroprotective mediators against damage caused by acute and chronic brain diseases. This evidence has been confirmed by experimental studies documenting the protective role of female sex hormones both in vitro and in vivo, although these studies did not specifically focus on Huntington’s disease (HD). -

Hitting a Wall: an Ambiguous Case of Wallenberg Syndrome
Open Access Case Report DOI: 10.7759/cureus.16268 Hitting a Wall: An Ambiguous Case of Wallenberg Syndrome James R. Pellegrini 1 , Rezwan Munshi 1 , Bohao Cao 1 , Samuel Olson 2 , Vincent Cappello 1 1. Internal Medicine, Nassau University Medical Center, East Meadow, USA 2. Physical Medicine and Rehabilitation, Stony Brook University, Stony Brook, USA Corresponding author: Bohao Cao, [email protected] Abstract Wallenberg syndrome is the most common stroke of the posterior circulation. Diagnosis of Wallenberg syndrome is often overlooked as initial MRI may show no visible lesion. We present an atypical case of Wallenberg syndrome in which the initial MRI of the brain was normal. Our patient is a 65-year-old male who was brought in by emergency medical services complaining of right- sided facial droop, slurred speech, and left-sided weakness for one day. Physical examination showed decreased left arm and leg strength compared to the right side, decreased left facial temperature sensations, decreased left arm and leg temperature sensations, and difficulty sitting upright with an associated leaning towards the left side. An initial magnetic resonance imaging (MRI) of the brain with and without contrast revealed no abnormality. In light of such a high suspicion for stroke based on the patient’s neurologic deficits, a repeat MRI of the brain was performed three days later and exposed a small focus of bright signal (hyperintensity) on T2-weighted fluid-attenuated inversion recovery and diffusion-weighted imaging (DWI) in the left posterior medulla. Wallenberg syndrome, also known as lateral medullary syndrome or posterior inferior cerebellar artery syndrome, is a constellation of symptoms caused by posterior vascular accidents. -

Cognition and Steroidogenesis in the Rhesus Macaque
Cognition and Steroidogenesis in the Rhesus Macaque Krystina G Sorwell A DISSERTATION Presented to the Department of Behavioral Neuroscience and the Oregon Health & Science University School of Medicine in partial fulfillment of the requirements for the degree of Doctor of Philosophy November 2013 School of Medicine Oregon Health & Science University CERTIFICATE OF APPROVAL This is to certify that the PhD dissertation of Krystina Gerette Sorwell has been approved Henryk Urbanski Mentor/Advisor Steven Kohama Member Kathleen Grant Member Cynthia Bethea Member Deb Finn Member 1 For Lily 2 TABLE OF CONTENTS Acknowledgments ......................................................................................................................................................... 4 List of Figures and Tables ............................................................................................................................................. 7 List of Abbreviations ................................................................................................................................................... 10 Abstract........................................................................................................................................................................ 13 Introduction ................................................................................................................................................................. 15 Part A: Central steroidogenesis and cognition ............................................................................................................ -
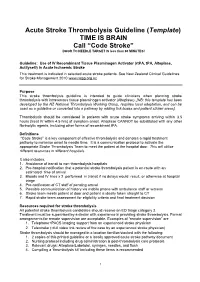
Acute Stroke Thrombolysis Guideline (Template) TIME IS BRAIN Call “Code Stroke” DOOR to NEEDLE TARGET IS Less Than 60 MINUTES!
Acute Stroke Thrombolysis Guideline (Template) TIME IS BRAIN Call “Code Stroke” DOOR TO NEEDLE TARGET IS less than 60 MINUTES! Guideline: Use of IV Recombinant Tissue Plasminogen Activator (rtPA, tPA, Alteplase, Actilyse®) in Acute Ischaemic Stroke This treatment is indicated in selected acute stroke patients. See New Zealand Clinical Guidelines for Stroke Management 2010 www.nzgg.org.nz Purpose This stroke thrombolysis guideline is intended to guide clinicians when planning stroke thrombolysis with intravenous tissue plasminogen activator (Alteplase). [NB: this template has been developed by the NZ National Thrombolysis Working Group, requires local adaptation, and can be used as a guideline or converted into a pathway by adding tick boxes and patient sticker areas]. Thrombolysis should be considered in patients with acute stroke symptoms arriving within 3.5 hours (treat IV within 4.5 hrs) of symptom onset. Alteplase CANNOT be substituted with any other fibrinolytic agents, including other forms of recombinant tPA. Definitions “Code Stroke” is a key component of effective thrombolysis and denotes a rapid treatment pathway to minimise onset to needle time. It is a communication protocol to activate the appropriate Stroke Thrombolysis Team to meet the patient at the hospital door. This will utilise different resources in different hospitals. It also includes: 1. Avoidance of transit to non-thrombolysis hospitals 2. Pre-hospital notification that a potential stroke thrombolysis patient is en-route with an estimated time of arrival 3. Bloods and IV lines x 2 performed in transit if no delays would result, or otherwise at hospital triage 4. Pre-notification of CT staff of pending arrival 5. -

GABA Receptors
D Reviews • BIOTREND Reviews • BIOTREND Reviews • BIOTREND Reviews • BIOTREND Reviews Review No.7 / 1-2011 GABA receptors Wolfgang Froestl , CNS & Chemistry Expert, AC Immune SA, PSE Building B - EPFL, CH-1015 Lausanne, Phone: +41 21 693 91 43, FAX: +41 21 693 91 20, E-mail: [email protected] GABA Activation of the GABA A receptor leads to an influx of chloride GABA ( -aminobutyric acid; Figure 1) is the most important and ions and to a hyperpolarization of the membrane. 16 subunits with γ most abundant inhibitory neurotransmitter in the mammalian molecular weights between 50 and 65 kD have been identified brain 1,2 , where it was first discovered in 1950 3-5 . It is a small achiral so far, 6 subunits, 3 subunits, 3 subunits, and the , , α β γ δ ε θ molecule with molecular weight of 103 g/mol and high water solu - and subunits 8,9 . π bility. At 25°C one gram of water can dissolve 1.3 grams of GABA. 2 Such a hydrophilic molecule (log P = -2.13, PSA = 63.3 Å ) cannot In the meantime all GABA A receptor binding sites have been eluci - cross the blood brain barrier. It is produced in the brain by decarb- dated in great detail. The GABA site is located at the interface oxylation of L-glutamic acid by the enzyme glutamic acid decarb- between and subunits. Benzodiazepines interact with subunit α β oxylase (GAD, EC 4.1.1.15). It is a neutral amino acid with pK = combinations ( ) ( ) , which is the most abundant combi - 1 α1 2 β2 2 γ2 4.23 and pK = 10.43. -

Α5gabaa Receptor Activity Sets the Threshold for Long-Term Potentiation and Constrains Hippocampus-Dependent Memory
The Journal of Neuroscience, April 14, 2010 • 30(15):5269–5282 • 5269 Cellular/Molecular ␣ 5GABAA Receptor Activity Sets the Threshold for Long-Term Potentiation and Constrains Hippocampus-Dependent Memory Loren J. Martin,1 Agnieszka A. Zurek,2 John F. MacDonald,2 John C. Roder,3 Michael F. Jackson,2 and Beverley A. Orser1,2,4 1Institute of Medical Science and 2Department of Physiology, University of Toronto, Toronto, Ontario M5S 1A8, Canada, 3Samuel Lunenfeld Research Institute, Mount Sinai Hospital, Toronto, Ontario M5G 1X5, Canada, and 4Department of Anesthesia, Sunnybrook Health Sciences Centre, Toronto, Ontario M4N 3M5, Canada Synaptic plasticity, which is the neuronal substrate for many forms of hippocampus-dependent learning, is attenuated by GABA type A receptor (GABAAR)-mediated inhibition. The prevailing notion is that a synaptic or phasic form of GABAergic inhibition regulates synaptic plasticity; however, little is known about the role of GABAAR subtypes that generate a tonic or persistent inhibitory conductance. ␣ ␣ We studied the regulation of synaptic plasticity by 5 subunit-containing GABAARs ( 5GABAARs), which generate a tonic inhibitory conductance in CA1 pyramidal neurons using electrophysiological recordings of field and whole-cell potentials in hippocampal slices ؊/؊ ␣ from both wild-type and null mutant mice for the 5 subunit of the GABAAR(Gabra5 mice). In addition, the strength of fear- ␣ associated memory was studied. The results showed that 5GABAAR activity raises the threshold for induction of long-term potentiation in a highly specific band of stimulation frequencies (10–20 Hz) through mechanisms that are predominantly independent of inhibitory ␣ synaptic transmission. The deletion or pharmacological inhibition of 5GABAARs caused no change in baseline membrane potential or inputresistancebutincreaseddepolarizationduring10Hzstimulation.Theencodingofhippocampus-dependentmemorywasregulated ␣ by 5GABAARs but only under specific conditions that generate moderate but not robust forms of fear-associated learning. -
42711 IPEG Programmaboekje
19 th Biennial Conference 19th Biennial Conference October 26th – 30th 2016 October 26 Nijmegen, the Netherlands th – 30 th 2016 Nijmegen, the Netherlands 2016 Nijmegen, 42711 IPEG programmaboekje omslag.indd 1 06-10-16 17:52 The “International Pharmaco-EEG Society, Association for Electrophysiological Brain Research in Preclinical and Clinical Pharmacology and Related Fields” (IPEG) is a non-profit organization, established in 1980 and composed of scientists and researchers actively involved in electrophysiological brain research in preclinical and clinical pharmacology, neurotoxicology and related areas of interest. my.thesis nl for the design of your Thesis & to show your Thesis 42711 IPEG programmaboekje omslag.indd 2 06-10-16 17:52 IPEG 2016 in Nijmegen | 1 Welcome to Nijmegen, dear attendants of the 19th IPEG meeting. Nijmegen, a 2000 year old city; Nijmegen, a Roman and a medieval city; Nijmegen, the home town of the first catholic university funded by the Faithfull to improve education of a suppressed part of the Netherlands; Nijmegen, the city that heavily suffered in WWII; Nijmegen, the home town of the Donders Institute. Nijmegen, as we hope and trust, your home town for the upcoming IPEG meeting. As you all know, electrophysiological brain research has a long tradition going back as far as 1875 when the first report on the animal electroencephalogram (EEG) was published by Caton. The often forgotten Polish physiologist Adolf Beck was also a EEG pioneer many years before Hans Berger’s initial reports. Beck recorded electrical potentials in several brain areas evoked by peripheral sensory stimuli. Using this technique, Beck localised various centres in the brain of several animal species and described desynchronization in electrical brain potentials. -

19Th Biennial IPEG Meeting Nijmegen, the Netherlands
Neuropsychiatric Electrophysiology 2016, 2(Suppl 1):8 DOI 10.1186/s40810-016-0021-4 MEETINGABSTRACTS Open Access 19th biennial IPEG Meeting Nijmegen, The Netherlands. 26-30 October 2016 Published: 29 November 2016 Training course measures. This will be illustrated by means of pertinent examples. These include elucidating the mechanisms of stimulant action re- A1 mediating deficient impulse control and the role of the cannabinoid Thalamocortical sleep oscillations system in human working memory, as well as drug effects on Igor Timofeev1,2 sensory gating and specific aspects of visual-spatial attention. Other 1Department of Psychiatry and Neuroscience, Université Laval, Québec, examples concern the added sensitivity of EEG and ERP measures, Canada; 2Centre de recherche de l’Institut universitaire en santé mentale relative to that of performance measures, in detecting effects of alco- de Québec (CRIUSMQ), Université Laval, Québec, Canada hol, and more generally in monitoring and predicting vigilance and Neuropsychiatric Electrophysiology 2016, 2(Suppl 1):A1 the ability to detect external signals in the immediate future. Rela- tions between brain signals and cognitive competences are revealed In waking and sleeping states, thalamocortical system generates a by either comparing different individuals, or moment-to-moment variety of oscillations ranging from 0.1 Hz to hundreds of Hz. Most of fluctuations within individuals, or differences in state (e.g., drug- them are present during NREM sleep, but slower activities prevail in induced) within individuals. this state of vigilance. Thalamocortical network is organized in a loop in which thalamocortical cells excite reticular thalamic and neocor- tical cells, reticular thalamic cells inhibit thalamocortical cells and A3 corticothalamic cells excite thalamocortical and reticular thalamic EEG and ERP as key techniques for functional brain alterations cells. -

Cognitive Behaviour Therapy (CBT) and Stroke Rehabilitation
Cognitive Behaviour Therapy (CBT) and Stroke Rehabilitation Amy Quilty OT Reg. (Ont.), Occupational Therapist Cognitive Behavioural Therapy (CBT) Certificate Program, University of Toronto Quinte Health Care: [email protected] Learning Objectives • To understand that CBT: • has common ground with neuroscience • principles are consistent with stroke best practices • treats barriers to stroke recovery • is an opportunity to optimize stroke recovery Question? Why do humans dominate Earth? The power of THOUGHT • Adaptive • Functional behaviours • Health and well-being • Maladaptive • Dysfunctional behaviours • Emotional difficulties Emotional difficulties post-stroke • “PSD is a common sequelae of stroke. The occurrence of PSD has been reported as high as 30–60% of patients who have experienced a stroke within the first year after onset” Canadian Stroke Best Practice Recommendations: Mood, Cognition and Fatigue Following Stroke practice guidelines, update 2015 http://onlinelibrary.wiley.com/doi/10.1111/ijs.12557/full • Australian rates: (Kneeborne, 2015) • Depression ~31% • Anxiety ~18% - 25% • Post Traumatic Stress ~10% - 30% • Emotional difficulties post-stroke have a negative impact on rehabilitation outcomes. Emotional difficulties post-stroke: PSD • Post stroke depression (PSD) is associated with: • Increased utilization of hospital services • Reduced participation in rehabilitation • Maladaptive thoughts • Increased physical impairment • Increased mortality Negative thoughts & depression • Negative thought associated with depression has been linked to greater mortality at 12-24 months post-stroke Nursing Best Practice Guideline from RNAO Stroke Assessment Across the Continuum of Care June : http://rnao.ca/sites/rnao- ca/files/Stroke_with_merged_supplement_sticker_2012.pdf Cognitive Behavioral Therapy (CBT) https://www.youtube.com/watch?v=0ViaCs0k2jM Cognitive Behavioral Therapy - CBT A Framework to Support CBT for Emotional Disorder After Stroke* *Figure 2, Framework for CBT after stroke. -

Classification Decisions Taken by the Harmonized System Committee from the 47Th to 60Th Sessions (2011
CLASSIFICATION DECISIONS TAKEN BY THE HARMONIZED SYSTEM COMMITTEE FROM THE 47TH TO 60TH SESSIONS (2011 - 2018) WORLD CUSTOMS ORGANIZATION Rue du Marché 30 B-1210 Brussels Belgium November 2011 Copyright © 2011 World Customs Organization. All rights reserved. Requests and inquiries concerning translation, reproduction and adaptation rights should be addressed to [email protected]. D/2011/0448/25 The following list contains the classification decisions (other than those subject to a reservation) taken by the Harmonized System Committee ( 47th Session – March 2011) on specific products, together with their related Harmonized System code numbers and, in certain cases, the classification rationale. Advice Parties seeking to import or export merchandise covered by a decision are advised to verify the implementation of the decision by the importing or exporting country, as the case may be. HS codes Classification No Product description Classification considered rationale 1. Preparation, in the form of a powder, consisting of 92 % sugar, 6 % 2106.90 GRIs 1 and 6 black currant powder, anticaking agent, citric acid and black currant flavouring, put up for retail sale in 32-gram sachets, intended to be consumed as a beverage after mixing with hot water. 2. Vanutide cridificar (INN List 100). 3002.20 3. Certain INN products. Chapters 28, 29 (See “INN List 101” at the end of this publication.) and 30 4. Certain INN products. Chapters 13, 29 (See “INN List 102” at the end of this publication.) and 30 5. Certain INN products. Chapters 28, 29, (See “INN List 103” at the end of this publication.) 30, 35 and 39 6. Re-classification of INN products. -

REVIEW ARTICLE the Genetics of Autism
REVIEW ARTICLE The Genetics of Autism Rebecca Muhle, BA*; Stephanie V. Trentacoste, BA*; and Isabelle Rapin, MD‡ ABSTRACT. Autism is a complex, behaviorally de- tribution of a few well characterized X-linked disorders, fined, static disorder of the immature brain that is of male-to-male transmission in a number of families rules great concern to the practicing pediatrician because of an out X-linkage as the prevailing mode of inheritance. The astonishing 556% reported increase in pediatric preva- recurrence rate in siblings of affected children is ϳ2% to lence between 1991 and 1997, to a prevalence higher than 8%, much higher than the prevalence rate in the general that of spina bifida, cancer, or Down syndrome. This population but much lower than in single-gene diseases. jump is probably attributable to heightened awareness Twin studies reported 60% concordance for classic au- and changing diagnostic criteria rather than to new en- tism in monozygotic (MZ) twins versus 0 in dizygotic vironmental influences. Autism is not a disease but a (DZ) twins, the higher MZ concordance attesting to ge- syndrome with multiple nongenetic and genetic causes. netic inheritance as the predominant causative agent. By autism (the autistic spectrum disorders [ASDs]), we Reevaluation for a broader autistic phenotype that in- mean the wide spectrum of developmental disorders cluded communication and social disorders increased characterized by impairments in 3 behavioral domains: 1) concordance remarkably from 60% to 92% in MZ twins social interaction; 2) language, communication, and and from 0% to 10% in DZ pairs. This suggests that imaginative play; and 3) range of interests and activities.