A Program Guide for Public Health: Partnering with Pharmacists
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
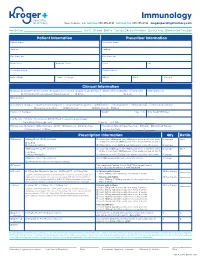
Immunology New Orleans, LA Toll Free 888.355.4191 Toll Free Fax 888.355.4192 Krogerspecialtypharmacy.Com
Immunology New Orleans, LA toll free 888.355.4191 toll free fax 888.355.4192 krogerspecialtypharmacy.com Need By Date: _________________________________________________ Ship To: Patient Office Fax Copy: Rx Card Front/Back Clinical Notes Medical Card Front/Back Patient Information Prescriber Information Patient Name Prescriber Name Address Address City State Zip City State Zip Main Phone Alternate Phone Phone Fax Social Security # Contact Person Date of Birth Male Female DEA # NPI # License # Clinical Information Diagnosis: J45.40 Moderate Asthma J45.50 Severe Asthma L20.9 Atopic Dermatitis L50.1 Chronic Idiopathic Urticaria (CIU) Eosinophil Levels J33 Chronic Rhinosinusitis with Nasal Polyposis Other: ________________________________ Dx Code: ___________ Drug Allergies Concomitant Therapies: Short-acting Beta Agonist Long-acting Beta Agonist Antihistamines Decongestants Immunotherapy Inhaled Corticosteroid Leukotriene Modifiers Oral Steroids Nasal Steroids Other: _____________________________________________________________ Please List Therapies Weight kg lbs Date Weight Obtained Lab Results: History of positive skin OR RAST test to a perennial aeroallergen Pretreatment Serum lgE Level: ______________________________________ IU per mL Test Date: _________ / ________ / ________ MD Specialty: Allergist Dermatologist ENT Pediatrician Primary Care Prescription Type: Naïve/New Start Restart Continued Therapy Pulmonologist Other: _________________________________________ Last Injection Date: _________ / ________ -
DC Health Systems Plan 2017
DISTRICT OF COLUMBIA HEALTH SYSTEMS PLAN 2017 NOTICE OF NON-DISCRIMINATION In accordance with the D.C. Human Rights Act of 1977, as amended, D.C. Code section 2.1401.01 et seq., the District of Columbia does not discriminate on the basis of race, color, religion, national origin, sex, age, marital status, personal appearance, sexual orientation, family responsibilities, matriculation, political affiliation, disability, source of income, or place of residence or business. Discrimination in violation of the Act will not be tolerated. Violators will be subject to disciplinary action. Published July, 2017 Dear Residents: Upon taking office in 2015, my Administration focused on improving health outcomes for all residents, recognizing that all government policies—from education and housing, to economic development and transportation—impact the health and wellness of our communities. Every Washingtonian, regardless of where they live, should have the ability to live a healthy and fulfilling life in our nation’s capital. This Health Systems Plan will serve as a guide for all stakeholders as they implement initiatives aimed at strengthening Washington DC’s health system to improve the overall health status of residents by ad- dressing social determinants of health and promoting health equity. Through this plan, we will ensure that public and private agencies throughout DC have the direction they need to make sound investments and implement initiatives that will improve the health and well-being of residents across all eight wards. I am proud of the work we have done thus far. In 2016, the number of newly diagnosed HIV cases in Washington, DC decreased by 52 percent to 347. -

Clinical Pharmacy Specialist
SAMPLE JOB DESCRIPTION Clinical Pharmacist Specialist I. JOB SUMMARY The Clinical Pharmacist Specialists are responsible and accountable for the provision of safe, effective, and prompt medication therapy. Through various assignments within the department, they provide support of centralized and decentralized medication-use systems as well as deliver optimal medication therapy to patients with a broad range of disease states. Clinical Pharmacist Specialists proficiently provide direct patient-centered care and integrated pharmacy operational services in a decentralized practice setting with physicians, nurses, and other hospital personnel. These clinicians are aligned with target interdisciplinary programs and specialty services to deliver medication therapy management within specialty patient care services and to ensure pharmaceutical care programs are appropriately integrated throughout the institution. In these clinical roles, Clinical Pharmacist Specialists participate in all necessary aspects of the medication-use system while providing comprehensive and individualized pharmaceutical care to the patients in their assigned areas. Pharmaceutical care services include but are not limited to assessing patient needs, incorporating age and disease specific characteristics into drug therapy and patient education, adjusting care according to patient response, and providing clinical interventions to detect, mitigate, and prevent medication adverse events. Clinical Pharmacist Specialists serve as departmental resources and liaisons to other -

STEM Disciplines
STEM Disciplines In order to be applicable to the many types of institutions that participate in the HERI Faculty Survey, this list is intentionally broad and comprehensive in its definition of STEM disciplines. It includes disciplines in the life sciences, physical sciences, engineering, mathematics, computer science, and the health sciences. Agriculture/Natural Resources Health Professions 0101 Agriculture and related sciences 1501 Alternative/complementary medicine/sys 0102 Natural resources and conservation 1503 Clinical/medical lab science/allied 0103 Agriculture/natural resources/related, other 1504 Dental support services/allied 1505 Dentistry Biological and Biomedical Sciences 1506 Health & medical administrative services 0501 Biochem/biophysics/molecular biology 1507 Allied health and medical assisting services 0502 Botany/plant biology 1508 Allied health diagnostic, intervention, 0503 Genetics treatment professions 0504 Microbiological sciences & immunology 1509 Medicine, including psychiatry 0505 Physiology, pathology & related sciences 1511 Nursing 0506 Zoology/animal biology 1512 Optometry 0507 Biological & biomedical sciences, other 1513 Osteopathic medicine/osteopathy 1514 Pharmacy/pharmaceutical sciences/admin Computer/Info Sciences/Support Tech 1515 Podiatric medicine/podiatry 0801 Computer/info tech administration/mgmt 1516 Public health 0802 Computer programming 1518 Veterinary medicine 0803 Computer science 1519 Health/related clinical services, other 0804 Computer software and media applications 0805 Computer systems -

Pharmacist-Physician Team Approach to Medication-Therapy
Pharmacist-Physician Team Approach to Medication-Therapy Management of Hypertension The following is a synopsis of “Primary-Care-Based, Pharmacist-Physician Collaborative Medication-Therapy Management of Hypertension: A Randomized, Pragmatic Trial,” published online in June 2014 in Clinical Therapeutics. What is already known on this topic? found that the role of the pharmacist differed within each study; whereas some pharmacists independently initiated and High blood pressure, also known as hypertension, is a changed medication therapy, others recommended changes major risk factor for cardiovascular disease, the leading to physicians. Pharmacists were already involved in care in all cause of death for U.S. adults. Helping patients achieve but one study. blood pressure control can be difficult for some primary care providers (PCPs), and this challenge may increase with After reviewing the RCTs, the authors conducted a randomized the predicted shortage of PCPs in the United States by 2015. pragmatic trial to investigate the processes and outcomes that The potential shortage presents an opportunity to expand result from integrating a pharmacist-physician team model. the capacity of primary care through pharmacist-physician Participants were randomly selected to receive PharmD-PCP collaboration for medication-therapy management (MTM). MTM or usual care from their PCPs. The authors conducted MTM performed through a collaborative practice agreement the trial within a university-based internal medicine medical allows pharmacists to initiate and change medications. group where the collaborative PharmD-PCP MTM team Researchers have found positive outcomes associated included an internal medicine physician and two clinical with having a pharmacist on the care team; however, the pharmacists, both with a Doctor of Pharmacy degree, at least evidence is limited to only a few randomized controlled 1 year of pharmacy practice residency training, and more than trials (RCTs). -

Chapter 54 Manual of Requirements for Family Child Care Registration
CHAPTER 54 MANUAL OF REQUIREMENTS FOR FAMILY CHILD CARE REGISTRATION STATE OF NEW JERSEY DEPARTMENT OF CHILDREN AND FAMILIES EFFECTIVE - March 20, 2017 EXPIRES - February 21, 2024 DEPARTMENT OF CHILDREN AND FAMILIES OFFICE OF LICENSING PO BOX 717 TRENTON, NEW JERSEY 08625-0717 Toll - Free Telephone 1-877-667-9845 N.J.A.C. 3A:54 MANUAL OF REQUIREMENTS FOR FAMILY CHILD CARE REGISTRATION SUBCHAPTER 1. GENERAL PROVISIONS................................................................................ 1 3A:54-1.1 Legal authority ................................................................................................................ 1 3A:54-1.2 Definitions ....................................................................................................................... 2 3A:54-1.3 Approval requirements for sponsoring organizations ..................................................... 4 3A:54-1.4 Public access to records ................................................................................................... 6 SUBCHAPTER 2. ADMINISTRATION OF SPONSORING ORGANIZATIONS ................... 8 3A:54-2.1 Sponsoring organization eligibility ................................................................................. 8 3A:54-2.2 Administrative responsibility .......................................................................................... 8 3A:54-2.3 Reporting requirements ................................................................................................... 9 3A:54-2.4 Sponsoring organization records -

Balance Billing Protection for Out-Of-Network Services
Form 405-A (eff. 1/2021) BALANCE BILLING PROTECTION FOR OUT-OF-NETWORK SERVICES Starting January 1, 2021, Virginia state law may protect you from “balance billing” when you get: • EMERGENCY SERVICES from an out-of-network hospital, or an out-of-network doctor or other medical provider at a hospital; or • NON-EMERGENCY SURGICAL OR ANCILLARY SERVICES from an out-of-network lab or health care professional at an in-network hospital, ambulatory surgical center or other health care facility. What is balance billing? • An “IN-NETWORK” health care provider has signed a contract with your health insurance plan. Providers who haven’t signed a contract with your health plan are called “OUT-OF-NETWORK” providers. • In-network providers have agreed to accept the amounts paid by your health plan after you, the patient, has paid for all required cost sharing (copayments, coinsurance and deductibles for covered services). • But, if you get all or part of your care from out-of-network providers, you could be billed for the difference between what your plan pays to the provider and the amount the provider bills you. This is called “balance billing.” • The new Virginia law prevents certain balance billing, but it does not apply to all health plans. Applies May Apply Does Not Apply o Fully insured managed care plans, o Employer-based coverage o Health plans issued to an including those bought through o Health plans issued to an employer association outside Virginia HealthCare.gov outside Virginia o Health plans that do not use a o The state employee health plan o Short-term limited duration plans network of providers o Group health plans that opt-in o Limited benefit plans How can I find out if I am protected? Be sure to check your plan documents or contact your health plan to find out if you are protected by this law. -

Botswana Health Professions Council (BHPC) Before Seeing Patients
BHPC Application Instructions for BUP Travelers Just as no person would be allowed to walk onto the wards of HUP or any other US hospital and begin treating patients without presenting their credentials, no one may practice in any hospital or clinic in Botswana without official permission. Any physician practicing medicine in Botswana is required to register with the Botswana Health Professions Council (BHPC) before seeing patients. To register you must bring the following documents with you to Botswana: 4 x passport photos 1 x notarized copy of passport photo page 2 x letters of recommendation from doctors/supervisors you work with (letters to be original, no digital copies allowed by BHPC, dated no older than six months) 1 x notarized copy of your medical degree/diploma 1 x notarized copy of your state medical license/registration 1 x CV Copy of offer letter (provided in Botswana) Cover letter of application form (provided in Botswana) Application fee (P30 ≈ $3) BUP staff will assist you in completing the application (pp 3-6 of this document) in country and take you to the BHPC on your first day during orientation to submit the forms and then again on the Wednesday following arrival to receive your approval. Note that you cannot practice medicine until the BHPC registration is completed. You should plan to arrive in Botswana on the weekend prior to when you plan to work so that your BHPC application can be turned in on Monday and you can receive registration certification on Wednesday afternoon. You will then be able to start to practice medicine on Thursday. -

Patient Safety Clinical Pharmacy Collaborative (PSPC) Guidebook
GUIDEBOOK Planning and Implementing a Successful Collaborative in a Rural Area How the Eastern Virginia Medical School (EVMS) Patient Safety and Clinical Pharmacy Services Collaborative is changing Pharmacy Services in the Eastern Virginia ACKNOWLEDGEMENTS Thank you to the many people who contributed to this document. We acknowledge the Eastern Virginia Medical School Patient Safety and Clinical Pharmacy Services Collaborative members who initiated the development of this document. Thank you to the participant organizations’ leadership members who consistently supported these efforts. The following individuals provided extensive time, effort and dedication to the development of this document: Judy Wessell Judy A. Wessell MSN, APRN, BC, ACRN, AACRN, AAHIVS. Ms. Wessell has been an HIV Nurse Practitioner for 13 years and a Registered Nurse for greater than 36 years. She received her diploma of Nursing from the Newport Hospital School of Nursing in Newport, RI, her BSN and MSN at Old Dominion University, Norfolk, VA. Ms. Wessell is currently the Nurse Practitioner Supervisor at the Eastern Virginia Medical School (EVMS), Center for Care of Immune Deficiency (C3ID), Infectious Disease Clinic. She is an HIV Health Educator with the EVMS AIDS Resource and Consultation Center, providing professional and community educational programs. She is a member of the quality improvement committee and a member of the EVMS Patient Safety and Clinical Pharmacy Collaborative. Tanya Kearney Tanya K. Kearney, MPA, has eight years of experience as Director for the AIDS Resource Center at Eastern Virginia Medical School. She works with health care providers, community- based AIDS service organizations, government agencies, professional associations and academic and community health care providers, to offer multidisciplinary educational programs on HIV/AIDS and other related topics. -

Pharmacy/Medical Drug Prior Authorization Form
High Cost Medical Drugs List High Cost Medical Drugs administered by Health Alliance™ providers within physician offices, infusion centers or hospital outpatient settings must be acquired from preferred specialty vendors. Health Alliance will not reimburse any drug listed as a “High Cost Medical Drug,” whether obtained from the provider’s own stock or via “buy-and-bill.” This drug list does not apply to members with Medicare coverage. Information on how to acquire these medications is located at the end of this document. Recent Updates Preferred Contact Drug Therapy Drug Name Code PA Effective Change Vendor Number Oncology – Injectable DARZALEX FASPRO J9144 YES 10/1/2021 CVS/Caremark® 800-237-2767 Added High Cost Medical Drug List Preferred Contact Drug Therapy Drug Name Code PA Effective Vendor Number Acromegaly SANDOSTATIN J2353 YES 7/1/2020 CVS/Caremark® 800-237-2767 Acromegaly SOMATULINE J1930 YES 7/1/2020 CVS/Caremark® 800-237-2767 Additional Products JETREA J7316 YES 7/1/2020 LDD Additional Products PROLASTIN J0256 YES 7/1/2020 LDD Additional Products QUTENZA J7336 NO 7/1/2020 LDD Additional Products REVCOVI J3590 YES 7/1/2020 LDD Additional Products RADICAVA J1301 YES 7/1/2020 CVS/Caremark® 800-237-2767 Additional Products SIGNIFOR J2502 YES 7/1/2020 Accredo® 866-759-1557 Additional Products SPRAVATO J3490 YES 7/1/2020 CVS/Caremark® 800-237-2767 Additional Products STRENSIQ J3590 YES 7/1/2020 LDD Additional Products THIOTEPA J9340 YES 7/1/2020 CVS/Caremark® 800-237-2767 Allergic Asthma CINQAIR J2786 YES 7/1/2020 CVS/Caremark® 800-237-2767 -

Clinical Pharmacy in Family Practice
Clinical Pharmacy in Family Practice John P. Geyman, MD One of the innovative directions in family prac services has been high.2 Similar collaborative ef tice during the last several years has been the in forts between family practice and clinical phar troduction of clinical pharmacists into some teach macy have been reported in other medical schools, ing and community practices. This is not surpris such as the Medical University of South Carolina2; ing in view of recent changes in pharmacy educa and in community hospital based family practice tion and practice, which have expanded the clini residencies, such as Family Medicine Spokane in cal training of clinical pharmacists and increased Washington State.4 the range of services which they provide. There With regard to community practices, several are growing numbers of clinical pharmacists in questions are immediately raised concerning this teaching hospitals, outpatient clinics, mental kind of interdisciplinary practice, including ethical health centers, and other institutional settings.1 and economic issues, if dispensing of drugs is to be Although the entry of clinical pharmacists into the carried out; also, logistic and procedural ques relatively smaller group settings of family practice tions; cost-benefit questions; and questions re is still an early trend, the experience to date in garding satisfaction of patients, physicians, and both teaching and community practice settings is pharmacists. Of particular interest in terms of how extremely positive. these questions have been resolved in one practice In this issue of The Journal, Love and his col is the report of Davis and his colleagues of their leagues describe the role and contributions of a experience since 1976 in a rural-suburban family clinical pharmacist in the university based family practice in Lexington, South Carolina.5 This prac practice residency program at the University of tice includes two family physicians and one clin Kentucky. -

Pre-Med & Other Health Programs
PRE-MED & OTHER HEALTH PROGRAMS Berkeley offers excellent undergraduate preparation for medical and other health-related professional schools and sends an impressive number of students on to these graduate programs each year. Cal, like most universities, does not offer a specific “pre-med” major. Few colleges in the United States do, because there is no specific major required for admission to medical or other health- related schools. All students obtain a bachelor’s degree before admission to medical school. For students seeking admission to dentistry, veterinary medicine, optometry, and other health- related graduate programs, many have received a bachelor’s degree prior to admission. What should I major in at Berkeley, AP credits will not satisfy prerequisites at most Does it make a difference where I if I want to go to medical school? medical schools.) Select an academic major that complete my academic preparation for interests you and allows flexibility in taking the There is no preferred pre-med major. Every year medical or other health-related schools? required pre-med courses. students with majors in the social sciences, The quality and reputation of the college or humanities, chemistry and engineering are What should I do when I’m not in class? university from which you graduate can play a accepted to medical school from Berkeley. role in your acceptance to a medical school. If you want to study biology at Berkeley, you One option is to experience the health care The high quality of Berkeley students and can choose from more than 25 areas of environment in a paid or volunteer position during the campus’ worldwide academic reputation specialization in the biological sciences, such college.