Mandibular Premolar Impaction: 2 Case Reports
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Maxillary Lateral Incisor Agenesis and Its Relationship to Overall Tooth Size Jane Wright, DDS, MS,A Jose A
RESEARCH AND EDUCATION Maxillary lateral incisor agenesis and its relationship to overall tooth size Jane Wright, DDS, MS,a Jose A. Bosio, BDS, MS,b Jang-Ching Chou, DDS, MS,c and Shuying S. Jiang, MSd Prosthodontists, orthodontists, ABSTRACT and general dentists frequently fi Statement of problem. Agenesis of the maxillary lateral incisor has been linked to differences in encounter dif culties when the size of the remaining teeth. Thus, the mesiodistal space required for definitive esthetic resto- attempting to restore the oc- ration in patients with missing maxillary lateral incisors may be reduced. clusion if unilateral or bilateral Purpose. The purpose of this study was to determine whether a tooth size discrepancy exists in maxillary lateral incisors are orthodontic patients with agenesis of one or both maxillary lateral incisors. congenitally missing. Restora- tion of the missing lateral Material and methods. Forty sets of dental casts from orthodontic patients (19 men and 21 women; mean 15.9 years of age; all of European origin) were collected. All casts had agenesis of one incisor using an implant- or both maxillary lateral incisors. Teeth were measured with a digital caliper at their greatest supported crown, a partial mesiodistal width and then compared with those of a control group matched for ethnicity, age, and fi xed dental prosthesis, or sex. Four-factor ANOVA with repeated measures of 2 factors was used for statistical analysis (a=.05). mesial movement of the Results. Orthodontic patients with agenesis of one or both maxillary lateral incisors exhibited canine are treatment options. smaller than normal tooth size compared with the control group. -

Tooth Size Proportions Useful in Early Diagnosis
#63 Ortho-Tain, Inc. 1-800-541-6612 Tooth Size Proportions Useful In Early Diagnosis As the permanent incisors begin to erupt starting with the lower central, it becomes helpful to predict the sizes of the other upper and lower adult incisors to determine the required space necessary for straightness. Although there are variations in the mesio-distal widths of the teeth in any individual when proportions are used, the sizes of the unerupted permanent teeth can at least be fairly accurately pre-determined from the mesio-distal measurements obtained from the measurements of already erupted permanent teeth. As the mandibular permanent central breaks tissue, a mesio-distal measurement of the tooth is taken. The size of the lower adult lateral is obtained by adding 0.5 mm.. to the lower central size (see a). (a) Width of lower lateral = m-d width of lower central + 0.5 mm. The sizes of the upper incisors then become important as well. The upper permanent central is 3.25 mm.. wider than the lower central (see b). (b) Size of upper central = m-d width of lower central + 3.25 mm. The size of the upper lateral is 2.0 mm. smaller mesio-distally than the maxillary central (see c), and 1.25 mm. larger than the lower central (see d). (c) Size of upper lateral = m-d width of upper central - 2.0 mm. (d) Size of upper lateral = m-d width of lower central + 1.25 mm. The combined mesio-distal widths of the lower four adult incisors are four times the width of the mandibular central plus 1.0 mm. -

Dental Anatomy Lecture (8) د
Dental Anatomy Lecture (8) د. حسين احمد Permanent Maxillary Premolars The maxillary premolars are four in number: two in the right and two in the left. They are posterior to the canines and anterior to the molars. The maxillary premolars have shorter crowns and shorter roots than those of the maxillary canines. The maxillary first premolar is larger than the maxillary second premolar. Premolars are named so because they are anterior to molars in permanent dentition. They succeed the deciduous molars (there are no premolars in deciduous dentition). They are also called “bicuspid -having two cusps-“, but this name is not widely used because the mandibular first premolar has one functional cusp. The premolars are intermediate between molars and canines in: Form: The labial aspect of the canine and the buccal aspect of premolar are similar. Function: The canine is used to tear food while the premolars and molars are used to grind it. Position: The premolars are in the center of the dental arch. [Type a quote from the document or the summary of [Type a quote from the document or the summary of an interesting point. You can position the text box an interesting point. You can anywhere in the document. position the text box Use the Text Box Tools tab to anywhere in the document. change the formatting of the Use the Text Box Tools tab to Some characteristic features to all posterior teeth: 1. Greater relative facio-lingual measurement as compared with the mesio-distal measurement. 2. Broader contact areas. 3. Contact areas nearly at the same level. -

Maxillary Premolars
Maxillary Premolars Dr Preeti Sharma Reader Oral & Maxillofacial Pathology SDC Dr. Preeti Sharma, Subharti Dental College, SVSU Premolars are so named because they are anterior to molars in permanent dentition. They succeed the deciduous molars. Also called bicuspid teeth. They develop from the same number of lobes as anteriors i.e., four. The primary difference is the well-formed lingual cusp developed from the lingual lobe. The lingual lobe is represented by cingulum in anterior teeth. Dr. Preeti Sharma, Subharti Dental College, SVSU The buccal cusp of maxillary first premolar is long and sharp assisting the canine as a prehensile or tearing teeth. The second premolars have cusps less sharp and function as grinding teeth like molars. The crown and root of maxillary premolar are shorter than those of maxillary canines. The crowns are little longer and roots equal to those of molars. Dr. Preeti Sharma, Subharti Dental College, SVSU As the cusps develop buccally and lingually, the marginal ridges are a little part of the occlusal surface of the crown. Dr. Preeti Sharma, Subharti Dental College, SVSU Maxillary second premolar Dr. Preeti Sharma, Subharti Dental College, SVSU Maxillary First Premolar Dr Preeti Sharma Reader Oral Pathology SDC Dr. Preeti Sharma, Subharti Dental College, SVSU The maxillary first premolar has two cusps, buccal and lingual. The buccal cusp is about 1mm longer than the lingual cusp. The crown is angular and buccal line angles are more prominent. The crown is shorter than the canine by 1.5 to 2mm on an average. The premolar resembles a canine from buccal aspect. -

Study of Root Canal Anatomy in Human Permanent Teeth
Brazilian Dental Journal (2015) 26(5): 530-536 ISSN 0103-6440 http://dx.doi.org/10.1590/0103-6440201302448 1Department of Stomatologic Study of Root Canal Anatomy in Human Sciences, UFG - Federal University of Goiás, Goiânia, GO, Brazil Permanent Teeth in A Subpopulation 2Department of Radiology, School of Dentistry, UNIC - University of Brazil’s Center Region Using Cone- of Cuiabá, Cuiabá, MT, Brazil 3Department of Restorative Dentistry, School of Dentistry of Ribeirão Beam Computed Tomography - Part 1 Preto, USP - University of São Paulo, Ribeirão Preto, SP, Brazil Carlos Estrela1, Mike R. Bueno2, Gabriela S. Couto1, Luiz Eduardo G Rabelo1, Correspondence: Prof. Dr. Carlos 1 3 3 Estrela, Praça Universitária s/n, Setor Ana Helena G. Alencar , Ricardo Gariba Silva ,Jesus Djalma Pécora ,Manoel Universitário, 74605-220 Goiânia, 3 Damião Sousa-Neto GO, Brasil. Tel.: +55-62-3209-6254. e-mail: [email protected] The aim of this study was to evaluate the frequency of roots, root canals and apical foramina in human permanent teeth using cone beam computed tomography (CBCT). CBCT images of 1,400 teeth from database previously evaluated were used to determine the frequency of number of roots, root canals and apical foramina. All teeth were evaluated by preview of the planes sagittal, axial, and coronal. Navigation in axial slices of 0.1 mm/0.1 mm followed the coronal to apical direction, as well as the apical to coronal direction. Two examiners assessed all CBCT images. Statistical data were analyzed including frequency distribution and cross-tabulation. The highest frequency of four root canals and four apical foramina was found in maxillary first molars (76%, 33%, respectively), followed by maxillary second molars (41%, 25%, respectively). -

The All-On-Four Treatment Concept: Systematic Review
J Clin Exp Dent. 2017;9(3):e474-88. All-on-four: Systematic review Journal section: Prosthetic Dentistry doi:10.4317/jced.53613 Publication Types: Review http://dx.doi.org/10.4317/jced.53613 The all-on-four treatment concept: Systematic review David Soto-Peñaloza 1, Regino Zaragozí-Alonso 2, María Peñarrocha-Diago 3, Miguel Peñarrocha-Diago 4 1 Collaborating Lecturer, Master in Oral Surgery and Implant Dentistry, Department of Stomatology, Faculty of Medicine and Dentistry, University of Valencia, Spain Peruvian Army Officer, Stomatology Department, Luis Arias Schreiber-Central Military Hospital, Lima-Perú 2 Dentist, Department of Stomatology, Faculty of Medicine and Dentistry, University of Valencia, Spain 3 Assistant Professor of Oral Surgery, Stomatology Department, Faculty of Medicine and Dentistry, University of Valencia, Spain 4 Professor and Chairman of Oral Surgery, Stomatology Department, Faculty of Medicine and Dentistry, University of Valencia, Spain Correspondence: Unidad de Cirugía Bucal Facultat de Medicina i Odontologìa Universitat de València Gascó Oliag 1 46010 - Valencia, Spain [email protected] Soto-Peñaloza D, Zaragozí-Alonso R, Peñarrocha-Diago MA, Peñarro- cha-Diago M. The all-on-four treatment concept: Systematic review. J Clin Exp Dent. 2017;9(3):e474-88. http://www.medicinaoral.com/odo/volumenes/v9i3/jcedv9i3p474.pdf Received: 17/11/2016 Accepted: 16/12/2016 Article Number: 53613 http://www.medicinaoral.com/odo/indice.htm © Medicina Oral S. L. C.I.F. B 96689336 - eISSN: 1989-5488 eMail: [email protected] Indexed in: Pubmed Pubmed Central® (PMC) Scopus DOI® System Abstract Objectives: To systematically review the literature on the “all-on-four” treatment concept regarding its indications, surgical procedures, prosthetic protocols and technical and biological complications after at least three years in function. -
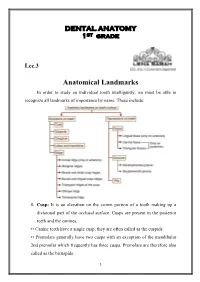
Anatomical Landmarks in Order to Study an Individual Tooth Intelligently, We Must Be Able to Recognize All Landmarks of Importance by Name
DENTAL ANATOMY 1ST grade Lec.3 Anatomical Landmarks In order to study an individual tooth intelligently, we must be able to recognize all landmarks of importance by name. These include: 1. Cusp: It is an elevation on the crown portion of a tooth making up a divisional part of the occlusal surface. Cusps are present in the posterior teeth and the canines. •• Canine teeth have a single cusp; they are often called as the cuspids. •• Premolars generally have two cusps with an exception of the mandibular 2nd premolar which frequently has three cusps. Premolars are therefore also called as the bicuspids. 1 •• Maxillary and mandibular 1st molars have five cusps, while other molars generally have four cusps. Each cusp is a gothic pyramid with four sides formed by four ridges that run down from the cusp tip: •• Mesial and distal cusp ridges (cusp slopes) •• Buccal/lingual cusp ridge •• Triangular ridge of the cusp. There are two cusp slopes on either side of the triangular ridge. In case of canines, there is a labial ridge analogous to the buccal ridge posterior teeth; there is a lingual ridge analogous to triangular ridge of posterior teeth. In the Table below the Number of cusps in different types of teeth: Tooth type Maxillary arch Mandibular arch Incisors 0 0 Canines 1 1 Premolars 2 2 in 1st premolar 3 or 2 in 2nd premolar Molars 1st molar 4 +1 accessory cusp 5 (cusp of Carabelli) 2nd molar 4 4 3rd molar 4 or 3 4 or 5 A cusp is named according to its location on the tooth. -

Anterior and Posterior Tooth Arrangement Manual
Anterior & Posterior Tooth Arrangement Manual Suggested procedures for the arrangement and articulation of Dentsply Sirona Anterior and Posterior Teeth Contains guidelines for use, a glossary of key terms and suggested arrangement and articulation procedures Table of Contents Pages Anterior Teeth .........................................................................................................2-8 Lingualized Teeth ................................................................................................9-14 0° Posterior Teeth .............................................................................................15-17 10° Posterior Teeth ...........................................................................................18-20 20° Posterior Teeth ...........................................................................................21-22 22° Posterior Teeth ..........................................................................................23-24 30° Posterior Teeth .........................................................................................25-27 33° Posterior Teeth ..........................................................................................28-29 40° Posterior Teeth ..........................................................................................30-31 Appendix ..............................................................................................................32-38 1 Factors to consider in the Aesthetic Arrangement of Dentsply Sirona Anterior Teeth Natural antero-posterior -

All-On-Four Treatment Concept in Dental Implants: a Review Articles
Surgery & Case Studies: Open Access Journal DOI: ISSN: 2643-6760 10.32474/SCSOAJ.2019.02.0001Review Article42 All-On-Four Treatment Concept in Dental Implants: A Review Articles Shakhawan M. Ali1*, Zanyar M. Amin2, Rebwar A Hama3, Hawbash O Muhamed3, Rozhyna P Kamal4 and Payman Kh Mahmud5 1Lecturer at Department of Oral and Maxillofacial Surgery, Shar Surgical Emergency Hospital, Sulaimany, Kurdistan region, Iraq 2Lecturer at Department of Oral and Maxillofacial Surgery, School of Medicine, Faculty of Dentistry, University of Sulaimani, Kurdistan Region, Iraq 3KBMS trainee, Maxillofacial Department, Sulaimany teaching hospital, Sulaimany, Kurdistan region, Iraq 4KBMS trainee, Restorative Department, Shorsh dental teaching center, Sulaimany, Kurdistan region, Iraq 5Lecturer at Department of Oral and Maxillofacial medicine, Shar teaching hospital, Kurdistan Region, Iraq *Corresponding author: Shakhawan M. Ali, Board certified Oral and Maxillofacial Surgery, Shar teaching hospital, Sulaimany, Kurdistan region, Iraq Received: March 03, 2019 Published: March 21, 2019 Abstract Edentulism has been demonstrated to have negative social and psychological effects on individuals that include adverse impacts on facial and oral esthetics, masticatory function and speech abilities, that when combined, are translated into significant reductions in patients’ quality of lives. It is well-known that immediate placement of implants is a challenging surgical procedure that requires proper treatment planning and surgical techniques. There are several prosthetic options to rehabilitate severely atrophic maxillae and mandibles have been developed such as conventional complete dentures, implant supported removable and implant supported fixed prosthesis. Implant supported prosthesis may not be feasible in many conditions because of the vicinity of vital anatomical structures, poor bone quality and quantity. -
CHAPTER 5Morphology of Permanent Molars
CHAPTER Morphology of Permanent Molars Topics5 covered within the four sections of this chapter B. Type traits of maxillary molars from the lingual include the following: view I. Overview of molars C. Type traits of maxillary molars from the A. General description of molars proximal views B. Functions of molars D. Type traits of maxillary molars from the C. Class traits for molars occlusal view D. Arch traits that differentiate maxillary from IV. Maxillary and mandibular third molar type traits mandibular molars A. Type traits of all third molars (different from II. Type traits that differentiate mandibular second first and second molars) molars from mandibular first molars B. Size and shape of third molars A. Type traits of mandibular molars from the buc- C. Similarities and differences of third molar cal view crowns compared with first and second molars B. Type traits of mandibular molars from the in the same arch lingual view D. Similarities and differences of third molar roots C. Type traits of mandibular molars from the compared with first and second molars in the proximal views same arch D. Type traits of mandibular molars from the V. Interesting variations and ethnic differences in occlusal view molars III. Type traits that differentiate maxillary second molars from maxillary first molars A. Type traits of the maxillary first and second molars from the buccal view hroughout this chapter, “Appendix” followed Also, remember that statistics obtained from by a number and letter (e.g., Appendix 7a) is Dr. Woelfel’s original research on teeth have been used used within the text to denote reference to to draw conclusions throughout this chapter and are the page (number 7) and item (letter a) being referenced with superscript letters like this (dataA) that Treferred to on that appendix page. -

Dental Anatomy
Dental Anatomy Lec 9 Dr. Ahmed Ghazi Permanent Mandibular Premolars Mandibular First Premolar It is the smallest premolar in the human dentition. It resembles both the mandibular canine and the mandibular second premolar in function and has some of the characteristics of each of them. A. Characteristics that resemble those of the mandibular canine: 1. The buccal cusp is long, sharp, and is the only occluding cusp. 2. The bucco-lingual measurement is similar to that of the mandibular canine. 3. The occlusal surface slopes sharply lingually in a cervical direction. 4. The mesio-buccal cusp ridge is shorter than the disto-buccal cusp ridge. 5. The outline form from the occlusal aspect resembles the incisal aspect of the mandibular canine. B. Characteristics that resemble those of the mandibular second premolar: 1. The mesial and distal contact areas are located at nearly the same level. 2. The curvature of the cervical line mesially and distally is similar. 3. The tooth has more than one cusp. 4. The length of the root of the mandibular first premolar is closer to the length of the root of the mandibular second premolar. 1 Principal Identifying Features 1. Marked lingual inclination of the crown. 2. Two cusps: buccal and lingual; the buccal cusp is larger, and the lingual cusp is like a more developed cingulum. 3. Circular occlusal outline. 4. Single rounded root. Buccal Aspect 1. The crown is roughly trapezoidal with a prominent middle buccal ridge, which continues from the cusp tip to the cervical line. 2. The mesial slope of the buccal cusp is shorter than the distal slop. -

Maxillary Lateral Incisor Agenesis: a Review of Literature Rehan Qamara, Annam Imtiazb, Muhammad Kamranc
REVIEW ARTICLE POJ 2012:4(2) 69- 72 Maxillary lateral incisor agenesis: A review of literature Rehan Qamara, Annam Imtiazb, Muhammad Kamranc Abstract Introduction: Tooth agenesis is defined as congenital absence of one or more teeth in primary or permanent dentition and is a common oral variation that affects a large population group. Among the missing one’s, maxillary lateral incisor is more frequent causing esthetic and functional impairments in the affected individual. It might be associated with systemic problems, syndromic conditions or other oral anomalies. Management of missing lateral incisors involves a multi-disciplinary approach for rehabilitation of impaired esthetics and function. The current literature review is offered to highlight the important characteristics of this anomaly for better management of such patients. Material and Methods: Several electronic databases were searched. Hand searching was done to short list the relevant articles. A total of 63 studies were retrieved out of which 48 most relevant studies were selected for the review. Results: maxillary lateral incisor agenesis is a common dental anomaly and has been reported to affect a wide group of populations. It can be unilateral or bilateral and females are more prone to be affected than the males. Conclusions: agenesis of maxillary lateral incisors is a common oral variation of either genetic or environmental origin. A comprehensive evaluation of the anomaly would be helpful to develop significant clinical management of the affected patients. Keywords: Tooth