(ELSO) Guidelines for Adult Respiratory Failure August, 2017
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Incidence, Risk Factors and Management of Severe Post-Transsphenoidal Epistaxis Q ⇑ Kenneth M
Journal of Clinical Neuroscience 22 (2015) 116–122 Contents lists available at ScienceDirect Journal of Clinical Neuroscience journal homepage: www.elsevier.com/locate/jocn Clinical Study Incidence, risk factors and management of severe post-transsphenoidal epistaxis q ⇑ Kenneth M. De Los Reyes a, Bradley A. Gross a, , Kai U. Frerichs a, Ian F. Dunn a, Ning Lin a, Jordina Rincon-Torroella a, Donald J. Annino b, Edward R. Laws a a Department of Neurological Surgery, Brigham and Women’s Hospital and Harvard Medical School, 75 Francis Street, Boston, MA, 02115, USA b Department of Otolaryngology, Brigham and Women’s Hospital and Harvard Medical School, Boston, MA, USA article info abstract Article history: Among the major complications of transsphenoidal surgery, less attention has been given to severe post- Received 16 June 2014 operative epistaxis, which can lead to devastating consequences. In this study, we reviewed 551 consec- Accepted 2 July 2014 utive patients treated over a 4 year period by the senior author to evaluate the incidence, risk factors, etiology and management of immediate and delayed post-transsphenoidal epistaxis. Eighteen patients (3.3%) developed significant postoperative epistaxis – six immediately and 12 delayed (mean postoper- Keywords: ative day 10.8). Fourteen patients harbored macroadenomas (78%) and 11 of 18 (61.1%) had complex Endoscopic nasal/sphenoid anatomy. In the immediate epistaxis group, 33% had acute postoperative hypertension. Epistaxis In the delayed group, one had an anterior ethmoidal pseudoaneurysm, and one had restarted anticoagu- Management Microscopic lation on postoperative day 3. We treated the immediate epistaxis group with bedside nasal packing fol- Pituitary lowed by operative re-exploration if conservative measures were unsuccessful. -

The Incidence of Microemboli to the Brain Is Less with Endarterectomy Than with Percutaneous Revascularization with Distal filters Or flow Reversal
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector From the Southern Association for Vascular Surgery The incidence of microemboli to the brain is less with endarterectomy than with percutaneous revascularization with distal filters or flow reversal Naren Gupta, MD, PhD,a Matthew A. Corriere, MD, MS,a,c Thomas F. Dodson, MD,a Elliot L. Chaikof, MD, PhD,a Robert J. Beaulieu, BS,b James G. Reeves, MD,a Atef A. Salam, MD,a and Karthikeshwar Kasirajan, MD,a Atlanta, Ga Background: Current data suggest microembolization to the brain may result in long-term cognitive dysfunction despite the absence of immediate clinically obvious cerebrovascular events. We reviewed a series of patients treated electively with carotid endarterectomy (CEA), carotid artery stenting (CAS) with distal filters, and carotid stenting with flow reversal (FRS) monitored continuously with transcranial Doppler scan (TCD) during the procedure to detect microembolization rates. Methods: TCD insonation of the M1 segment of the middle cerebral artery was conducted during 42 procedures (15 CEA, 20 CAS, and 7 FRS) in 41 patients seen at an academic center. One patient had staged bilateral CEA. Ipsilateral microembolic signals (MESs) were divided into three phases: preprotection phase (until internal carotid artery [ICA] cross-shunted or clamped if no shunt was used, filter deployed, or flow reversal established), protection phase (until clamp/shunt was removed, filter removed, or antegrade flow re-established), and postprotection phase (after clamp/ shunt was removed, filter removed, or antegrade flow re-established). Descriptive statistics are reported as mean ؎ SE for continuous variables and N (%) for categorical variables. -

Oxygen Saturation Index
RESEARCH LETTERS We observed that poor psychosocial care had high Department of Pediatrics, Dr SN Medical College, association with malnutrition, and that the interactions Jodhpur, Rajasthan, India. between SAM children and their parents were less optimal *[email protected] than for the controls. The restriction of movement leading REFERENCES to lesser interaction with the surroundings, curtailed 1. Operational Guidelines on Facility Based Management of independence, volition activity, and the ability to ask for or Children with Severe Acute Malnutrition, Ministry of obtain food could lead to malnutrition [4]. If mother is also Health and Family Welfare,Government of India,2011. illiterate, it further increases the chances of developing Available from: http://www.nihf.org/ nchrc –publictions/ severe acute malnutrition [5]. The limitations of this study operational guidelines. Accessed February 25,2014. were small sample size and a hospital-based setting that 2. Ruel MT, Arimond M. Measuring childcare practices: approaches, indicators, and implications for programs. Intl could not delineate the actual home environment. Food Policy Res Inst. 2003;6:1-81. We feel that it is imperative that the psychosocial care 3. Bradley RH, Munfrom DJ, Whiteside L, Caldwell BM, environment of the child suffering with severe acute Casey PH, Kirby R, et al. A reexamination of the malnutrition be thoroughly probed using a questionnaire association between HOME scores and income. Nurs Res. 1994;43:260-6. such as the one suggested in our study, and psychosocial 4. Engle PL, Bentley M, Pelto G. The role of care in nutrition care and rehabilitation should be brought into focus and programmes: current research and a research agenda. -

World Journal of Hepatology
World Journal of W J H Hepatology Submit a Manuscript: https://www.f6publishing.com World J Hepatol 2020 June 27; 12(6): 288-297 DOI: 10.4254/wjh.v12.i6.288 ISSN 1948-5182 (online) ORIGINAL ARTICLE Retrospective Cohort Study Hospital teaching status on the outcomes of patients with esophageal variceal bleeding in the United States Pavan Patel, Laura Rotundo, Evan Orosz, Faiz Afridi, Nikolaos Pyrsopoulos ORCID number: Pavan Patel Pavan Patel, Faiz Afridi, Nikolaos Pyrsopoulos, Division of Gastroenterology and Hepatology, (0000-0001-5682-4939); Laura Rutgers - New Jersey Medical School, Newark, NJ 07101-1709, United States Rotundo (0000-0002-4094-3682); Evan Orosz (0000-0003-2474-5501); Laura Rotundo, Evan Orosz, Department of Medicine, Rutgers - New Jersey Medical School, Faiz Afridi (0000-0002-0172-0486); Newark, NJ 07101-1709, United States Nikolaos Pyrsopoulos (0000-0002-6950-8174). Corresponding author: Nikolaos Pyrsopoulos, FACP, MD, PhD, Chief Doctor, Professor, Division of Gastroenterology and Hepatology, Rutgers – New Jersey Medical School, 185 S. Author contributions: Patel P Orange Avenue, MSB H-535, Newark, NJ 07101-1709, United States. provided conception and design of [email protected] the study, acquisition and analysis of data, and drafting of the manuscript; Rotundo L, Afridi F and Orosz E drafted the manuscript; Pyrsopoulos N Abstract contributed to the manuscript by BACKGROUND providing revision and oversight Acute variceal bleeding is a major complication of portal hypertension and is a of its writing. leading cause of death in patients with cirrhosis. There is limited data on the Institutional review board outcomes of patients with esophageal variceal bleeding in teaching versus statement: This study did not nonteaching hospitals. -

Flow Versus Pressure Triggering in Mechanically Ventilated Acute Respiratory Failure Patients Magdy M
198 Original article Flow versus pressure triggering in mechanically ventilated acute respiratory failure patients Magdy M. Khalila, Nevine M. Elfattaha, Mohsen M. El-Shafeyb, Nermine M. Riada, Raed A. Aidb, Alaa M. Ananyc Background The effects of fl ow triggering (FT) compared the PT group (P < 0.001). In patients with obstructive with pressure triggering (PT) on breathing effort have pulmonary disorders, combined pulmonary disorders, and been the focus of several studies, and discrepant results less severe disease (APACHE II <32.5), there was no have been reported; yet, it remains an area of confl ict that signifi cant difference between both PT and FT groups in warrants further studies. these parameters. Objective The aim of this work is to compare fl ow versus Conclusion FT may be considered to be better than PT in ventilating patients with acute respiratory failure. PT in ventilating acute respiratory failure patients with a restrictive pattern and those with higher severity scoring. In Patients and methods One hundred patients with acute obstructive and mixed ventilatory impairment, use of either respiratory failure of pulmonary origin were assigned of them does not make a difference. Egypt J Broncho 2015 randomly to two groups: 50 patients ventilated with PT 9:198–210 and 50 patients ventilated with FT. The primary end points © 2015 Egyptian Journal of Bronchology. were weaning duration, evaluation of patient/machine synchronization, total duration of ventilation and ICU stay as Egyptian Journal of Bronchology 2015 9:198–210 well time under sedation and occurrence of complications. Keywords: mechanical ventilation, respiratory failure, triggering Mortality was considered the secondary end point. -

Research Article Endothelial Dysfunction of Patients with Peripheral Arterial Disease Measured by Peripheral Arterial Tonometry
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Crossref Hindawi Publishing Corporation International Journal of Vascular Medicine Volume 2016, Article ID 3805380, 6 pages http://dx.doi.org/10.1155/2016/3805380 Research Article Endothelial Dysfunction of Patients with Peripheral Arterial Disease Measured by Peripheral Arterial Tonometry Kimihiro Igari, Toshifumi Kudo, Takahiro Toyofuku, and Yoshinori Inoue Division of Vascular and Endovascular Surgery, Department of Surgery, Tokyo Medical and Dental University, 1-5-45 Yushima, Bunkyo-ku, Tokyo 113-8519, Japan Correspondence should be addressed to Kimihiro Igari; [email protected] Received 16 July 2016; Revised 17 September 2016; Accepted 27 September 2016 Academic Editor: Thomas Schmitz-Rixen Copyright © 2016 Kimihiro Igari et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Objective. Endothelial dysfunction plays a key role in atherosclerotic disease. Several methods have been reported to be useful for evaluating the endothelial dysfunction, and we investigated the endothelial dysfunction in patients with peripheral arterial disease (PAD) using peripheral arterial tonometry (PAT) test in this study. Furthermore, we examined the factors significantly correlated with PAT test. Methods. We performed PAT tests in 67 patients with PAD. In addition, we recorded the patients’ demographics, including comorbidities, and hemodynamical status, such as ankle brachial pressure index (ABI). Results. In a univariate analysis, the ABI value ( = 0.271, = 0.029) and a history of cerebrovascular disease ( = 0.208, = 0.143) were found to significantly correlatewithPATtest,whichcalculatedthereactivehyperemiaindex(RHI).Inamultivariateanalysis,onlytheABIvalue significantly and independently correlated with RHI ( = 0.254, = 0.041). -
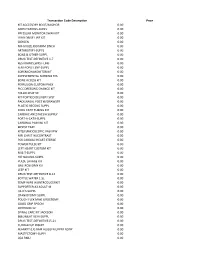
Transaction Code Description
Transaction Code Description Price KIT ACCESSORY BOOT/ANCHOR 0.00 AMPUTATIONS-SUPPL 0.00 PRESSURE MONITOR SWAN KIT 0.00 LVAD DRIVE LINE KIT 0.00 OXYGEN 0.00 NU-GAUZE,IODAFRM 1INCH 0.00 ARTHROTMY-SUPPL 0.00 BONE & OTHER-SUPPL 0.00 DRUG TEST-DEFINITIVE 1-7 0.00 RESTRAINTS,WRST-LMB 0.00 FEM-POPLIT.BYP-SUPPL 0.00 SORENSON MONITOR KIT 0.00 SUPPLEMENTAL NURSING SYS 0.00 BONE ACCESS KIT 0.00 PERFUSION CUSTOM PACK 0.00 PICC DRESSING CHANGE KIT 0.00 FOLLOLWUP 30 0.00 KIT PORTICO DELIVERY SYST 0.00 PACK,NASAL POST W/DRAWSTR 0.00 PLASTIC RECONS-SUPPL 0.00 COOL CATH TUBING KIT 0.00 CARDIAC ANESTHESIA SUPPLY 0.00 PORT-A-CATH-SUPPL 0.00 CARDINAL PAIN INJ KIT 0.00 BIOPSY TRAY 0.00 KIT(LF)ENDOSCOPIC VASVIEW 0.00 MRI CHEST W/CONTRAST 0.00 PCK CARDIAC HEART STERILE 0.00 POWER PULSE KIT 0.00 LEFT HEART CUSTOM KIT 0.00 M & T-SUPPL 0.00 HIP NAILING-SUPPL 0.00 PULSE LAVAGE KIT 0.00 GASTROSTOMY KIT 0.00 LEEP KIT 0.00 DRUG TEST-DEFINITIVE 8-14 0.00 BOTTLE WATER 1.5L 0.00 TEMP WIRE W/INTRODUCERKIT 0.00 SUPPORTER,A3 ADULT-M 0.00 I & D'S-SUPPL 0.00 CRANIOTOMY-SUPPL 0.00 POUCH FLEX MAXI UROSTOMY 0.00 GOOD GRIP SPOON 0.00 OXYHOOD 12- 0.00 SPINAL CARE KIT JACKSON 0.00 BI&UNILAT VEIN-SUPPL 0.00 DRUG TEST-DEFINITIVE15-21 0.00 CUDDLECUP INSERT 0.00 BLANKET (LF) BAIR HUGGER UPPER BODY 0.00 MASTECTOMY-SUPPL 0.00 LOA RMU 0.00 PACK LINQ 0.00 CHOLECYSTECTOM-SUPPL 0.00 RES BWL,SIG,AP-SUPPL 0.00 TRAY BIOPSY GENERAL UTIL 0.00 KIT(LF)CUSTOM SYRINGE ANGIO 0.00 OXISENSOR(LF)PEDI (PINK) 0.00 THORACIC SURG-SUPPL 0.00 NU-GAUZE PLAIN 1/2INCH 0.00 NU-GAUZE,IODAFRM 1/4INCH 0.00 PICC -

8 Implantable Membrane Oxygenator
Artificial Lung 8 . Cardiopulmonary Bypass - oxgenator 1 Cardiopulmonary Bypass § Cardiopulmonary bypass (CPB), also called heart-lung bypass, allows the temporary replacement of the gas exchange function of the lungs and the blood-pumping function of the heart § The terms pump-oxygenator and heart–lung machine graphically describe the equipment used § By extension, the term is also applies to surgical procedures which take place primarily on the external aspects of the heart, such as creating new routes for blood to reach the distal coronary arteries from the aorta 3 Cardiopulmonary Bypass § As usually employed for cardiac surgery, the heart–lung machine is part of a total, venoarterial cardiopulmonary bypass circuit à meaning that all the venous blood returning to the right heart cavities is collected in the extracorporeal circuit à circulated through the gas exchange device, from where it is pumped back into the arterial tree à thereby “bypassing” the heart cavities and the pulmonary circulation 5 Cardiopulmonary Bypass Scheme of standard operating conditions during cardiopulmonary bypass 6 Cardiopulmonary Bypass 7 Artificial Lung Artificial Lung vs. Natural Lung 8 Artificial Lung vs. Natural Lung § In the natural lungs, the factors underlying exchange across the alveolo-capillary barrier and transport by the blood can be grouped into four classes:- ú The ventilation of the lungs (the volume flow rate of gas) and the composition of the gas mixture to which mixed venous (pulmonary artery) blood will be exposed 9 Artificial Lung vs. Natural Lung § In the natural lungs, the factors underlying exchange across the alveolo-capillary barrier and transport by the blood can be grouped into four classes:- ú The permeability of the materials which separate the gas phase from the blood phase in the pulmonary alveoli 10 Artificial Lung vs. -

Left Atrial to Femoral Artery Full Cardiopulmonary Bypass: a Novel Technique for Descending and Thoracoabdominal Aortic Surgery
Published online: 2019-12-09 Original Article 19 Left Atrial to Femoral Artery Full Cardiopulmonary Bypass: A Novel Technique for Descending and Thoracoabdominal Aortic Surgery Dimitra Papanikolaou, MD1 Chris Savio, BS, CCP1 Mohammad A. Zafar, MBBS1 Leon Freudzon, MD1 Jinlin Wu, MD1 Mohamed Abdelbaky, MD1 Keith J. Pelletier, MBA, MHS, CCP1 Joelle Buntin, MSN, RN, RN-BC1 Thais Faggion Vinholo, BS, MSc1 Bulat A. Ziganshin, MD, PhD1,2 Brian Schwartz, MS, CCP1 John A. Elefteriades, MD, PhD (Hon)1 1 Aortic Institute at Yale-New Haven Hospital, Yale University School Address for correspondence John A. Elefteriades, MD, Aortic Institute of Medicine, New Haven, Connecticut at Yale-New Haven, Yale University School of Medicine, Clinic Building 2 Department of Surgical Diseases, Kazan State Medical University, CB 317, 789 Howard Avenue, New Haven, CT 06519 Kazan, Russia (e-mail: [email protected]). Int J Angiol 2020;29:19–26. Abstract Left atrial-femoral artery (LA-FA) bypass with a centrifugal pump and no oxygenator is commonly used for descending and thoracoabdominal aortic (DTAA) operations, mitigating the deleterious effects of cross-clamping. We present our initial experience performing DTAA replacement under LA-FA (left-to-left) cardiopulmonary bypass (CPB) with an oxygenator. DTAA replacement under LA-FA bypass with an oxygenator was performed in 14 consecutive patients (CPB group). The pulmonary vein and femoral artery (or distal aorta) were cannulated and the full CPB machine were used, including oxygenator, roller pump, pump suckers, and kinetically enhanced drainage. The CPB group was compared with 50 consecutive patients who underwent DTAA replacement utilizing traditional LA-FA bypass without an oxygenator (LA-FA group). -

High-Frequency Ventilator Device Trade Name
SUMMARY OF SAFETY AND EFFECTIVENESS DATA I. General Information Device Generic Name: High-Frequency Ventilator Device Trade Name: SensorMedics Model 3100B High- Frequency Oscillatory Ventilator Sponsor Name and Address: SensorMedics Corporation 22705 Savi Ranch Parkway Yorba Linda, CA 92887-4645 PMA Number: P890057/S14 Date of Panel Recommendation: July 16, 2001 Date of Notice of Approval: September 24, 2001 II. Indications for Use The SensorMedics 3100B is indicated for use in the ventilatory support and treatment of selected patients 35 kilograms and greater with acute respiratory failure. III. Contraindications This Model 3100B has no specific contraindications. IV. Device Description The Model 3100B consists of six subsystems, and is used with an external air/oxygen blender and an external humidifier. The six subsystems are: (1) pneumatic logic and control; (2) patient circuit; (3) oscillator subsystem; (4) airway pressure monitor; (5) electronic control and alarm subsystem; and (6) electrical power supply. During use with a patient in acute respiratory failure, the Model 3100B maintains a positive mean airway pressure, upon which pressure oscillations are superimposed at a rate between approximately 3 and 15 per second. The pressure oscillations achieve ventilation of the patient. Page 1 of 15 Pneumatic Logic and Control The pneumatic logic and control subsystem receives pressurized, blended gas from the external air/oxygen blender. The subsystem includes three controls: 1. A bias flow control sets the continuous rate at which the blended gas flows from the external blender, through the bias flow tube and the patient circuit, and past the tracheal tube connection port. The bias flow can be set as high as 60 L/min. -

The Mayo Gibbon Heart-Lung Bypass Machine in the Marc
Mayo Clinic Proceedings Legacy December 2014 Pioneers in Cardiac Surgery: The Mayo Gibbon Heart-Lung Bypass Machine This preliminary report shared the results from animal studies, but by May of that same year, Mayo Clinic had initiated use of the apparatus for human subjects and reported on the outcome in 8 cases.2 These patients had the following conditions: (1) ventricular septal defect, (2) Tetralogy of Fallot, or (3) persistent common atrioventricular canal. Four of the patients survived the surgery, one died shortly after the procedure, two died 3 hours postoperatively, and one died 6 days postoperatively.2 Mayo Clinic continued to study and develop successful surgical treatments in cardiology throughout the ensuing years. More than 60 years have passed since these first attempts, and success in cardiac surgery is directly related to these courageous research pioneers and patients. 1,2,3 This historical line of research in In the March 13, 1955, issue of The Proceedings cardiology also represents another successful of the Staff Meetings of the Mayo Clinic, Dr collaboration between the field of medicine John W. Kirklin and colleagues shared a and industry. International Business Machines preliminary report of their research from the (IBM) aided in the design and development of previous 3 years which tackled the challenges the Mayo Gibbon Heart-Lung Bypass of cardiac surgery. While other types of Machine.1,2,3 surgeries have their own impediments, cardiac surgery is dominated by the need to keep a References patient alive during the procedure while 1. Jones RE, Donald DE, Swan HJ, Harshbarger HG, maintaining the function of the circulatory Kirklin JW, Wood EH. -

New York State Surgical and Invasive Procedure Protocol (NYSSIPP)
State of New York Department of Health Office of Health Systems Management Division of Primary and Acute Care Services New York State Surgical and Invasive Procedure Protocol for Hospitals ~ Diagnostic and Treatment Centers Ambulatory Surgery Centers ~ Individual Practitioners Antonia C. Novello, M.D., M.P.H., Dr.P.H. Commissioner of Health Hon. George E. Pataki Governor – State of New York September 2006 Surgical and Invasive Procedure Protocol September 2006 NEW YORK STATE SURGICAL AND INVASIVE PROCEDURE PROTOCOL (FOR THE PREVENTION OF WRONG PATIENT, WRONG SITE, WRONG SIDE & WRONG INVASIVE PROCEDURE EVENTS) I. STATEMENT OF PURPOSE The State of New York is committed to providing its residents access to quality health care. Hon. George E. Pataki, Governor and Antonia C. Novello M.D., M.P.H., Dr.P.H., Commissioner of Health, continue to work toward a system that reduces medical and surgical errors by commitment to a safe and protected patient care environment. Key to achieving this goal is promoting a culture of safety and strengthening open communication among health care providers, individual practitioners and the patients they serve. One of the goals of Governor Pataki and Commissioner Novello, is the elimination of wrong patient, wrong site, wrong side and wrong invasive procedures, through the development of comprehensive systems that ensure the correct procedure is done on the correct patient on the correct site. Increased practitioner awareness combined with strong provider protocols and standardization will enhance the patient safety measures currently in place. The New York State Surgical and Invasive Procedure Protocol (NYSSIPP) developed by the Procedural and Surgical Site Verification Panel (PSSVP) is intended for all patient care settings and for all individual practitioners.