The Publications Files/27 Photopharmacology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Spotlights on Our Sister Journals: Chemistryopen 5
On these pages, we feature aselection computer,click on any of the items to of the excellent work that has recently read the full article. Otherwise please been published in our sister journals. see the DOIs for easy online access If you are reading these pages on a through Wiley Online Library. Iodine Adducts A. Reinholdt, T. Vosch, J. Bendix* Modification of s-Donor Properties of TerminalCarbideLigands Investigated Through Carbide–Iodine AdductFormation To give and take:terminal ruthenium carbidecomplexes [(Cy P) X Ru C] (1;X= halide or pseudohalide), form charge-transfer 3 2 2 adducts with I2 exhibitinglarge variation in bond lengths and stretching frequencies. This showsthat the auxiliary ligand sphere on rutheniumenables control over the s-donor properties of car- bide ligands, elucidating their isolobal relationship with carbon monoxide. Angew.Chem. Int. Ed. DOI: 10.1002/anie.201606551 Density Functional Theory J. I. Schweizer, L. Meyer,A.Nadj, M. Diefenbach, M. C. Holthausen* Unraveling the Amine-Induced Disproportionation Reaction of Perchlorinated Silanes—A DFT Study Aneo twist:ADFT study on the amine-induceddisproportionation reactionofSi2Cl6 to neo-Si5Cl12 discloses astepwise rather than a concerted silylene insertion mechanism, which was generally ac- cepted for over half acentury. The resulting pictureappears gener- alizabletothe relatedchloride-induced chemistry recently explored (see graphic). Chem. Eur.J. DOI: 10.1002/chem.201602724 Aza-Diels–Alder Reactions Y. Kumatabara, S. Kaneko, S. Nakata,S.Shirakawa,* K. Maruoka Hydrogen-BondingCatalysis of TetraalkylammoniumSalts in an Aza-Diels–Alder Reaction Under observation:Apiperidine-derived tetraalkylammoniumsalt with anon-coordinating counteranion worked as an effective hydro- gen-bonding catalyst in an aza-Diels–Alder reactionofimines anda Danishefskydiene. -

Annual Report: CY2018 Chempubsoc Europe
1 Annual Report: CY2018 ChemPubSoc Europe Growth, change, awards, and sponsorship More scientists, more publications, more competition. As in the past, growth continued unabated worldwide in 2018 and is also reflected in the performance metrics of the ChemPubSoc Europe / Wiley-VCH publishing program, which now consists of 16 titles. The most recent product, ChemSystemsChem, was announced in Fall 2018. In 2018, the journals that are co-owned by ChemPubSoc Europe societies published nearly 9,000 articles (excluding contributions to the online publication ChemViews Magazine). Compared to the previous year, manuscript submissions grew by 12%, and the number of published articles rose by approximately 5%. A record number of full-text downloads, >8.9 million, was witnessed for the ChemPubSoc Europe journals, with increases in usage compared to the same time last year; notable among them ca. +20–30% for ChemCatChem, ChemElectroChem, ChemMedChem, and ChemPlusChem; and ca. +70% for ChemistrySelect and ChemPhotoChem. Approximately 3% of articles published in ChemPubSoc Europe's hybrid journals in 2018 were open access: ca. 10% at ChemBioChem and ca. 5% at ChemCatChem, Chemistry—A European Journal, ChemMedChem, and ChemPhysChem, respectively. ChemPubSoc Europe's gold open access journal, ChemistryOpen, experienced a ca. 47% growth in submissions compared to 2017. Generational change After the retirement of Peter Gölitz in November 2017, additional responsibility was taken on by Guido Herrmann (VP, Co-Managing Director Wiley-VCH, since April 1, 2017), Eva Wille (VP, Executive Director Wiley-VCH), Neville Compton (Editor-in-Chief of Angewandte Chemie and publisher for the GDCh journals), Haymo Ross (Editor-in-Chief of Chemistry—A European Journal and publisher of the ChemPubSoc Europe journals), Theresa Kueckmann (Editor-in-Chief of Chemistry—An Asian Journal and publisher for the Asian Chemical Editorial Society (ACES) journals), and Greta Heydenrych (development of new journals). -

Wiley Article Publication Charges for Hybrid Open Updated: 17 March 2021
Wiley Article Publication Charges for Hybrid Open Updated: 17 March 2021 Online Full Arti ISSN Journal Title USD $ 1467-6281 Abacus 2.500 1553-2712 Academic Emergency Medicine 3.000 1467-629X Accounting & Finance 3.000 1911-3838 Accounting Perspectives 2.500 1399-6576 Acta Anaesthesiologica Scandinavica 3.800 2053-2733 Acta Crystallographica Section A: Foundations and Advances 3.750 2052-5206 Acta Crystallographica Section B: Structural Science, Crystal Engineering and Mater 3.750 2053-2296 Acta Crystallographica Section C: Structural Chemistry 3.600 2059-7983 Acta Crystallographica Section D: Structural Biology 3.850 1755-6724 Acta Geologica Sinica (English Edition) 3.000 1600-0404 Acta Neurologica Scandinavica 4.000 1600-0412 Acta Obstetricia et Gynecologica Scandinavica 4.000 1755-3768 Acta Ophthalmologica 3.950 1651-2227 Acta Paediatrica: Nurturing the Child 3.300 1748-1716 Acta Physiologica 3.700 1600-0447 Acta Psychiatrica Scandinavica 3.600 1463-6395 Acta Zoologica 3.000 1360-0443 Addiction 3.700 1369-1600 Addiction Biology 3.700 2161-0029 Adultspan Journal 2.500 2701-0198 Advanced Biology 3.800 2578-0727 Advanced Control for Applications 2.500 2199-160X Advanced Electronic Materials 4.200 1614-6840 Advanced Energy Materials 5.000 1527-2648 Advanced Engineering Materials 4.100 1616-3028 Advanced Functional Materials 5.000 2192-2659 Advanced Healthcare Materials 4.200 1521-4095 Advanced Materials 5.000 2196-7350 Advanced Materials Interfaces 4.200 2365-709X Advanced Materials Technologies 4.200 2195-1071 Advanced Optical Materials -
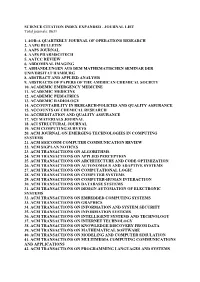
SCIENCE CITATION INDEX EXPANDED - JOURNAL LIST Total Journals: 8631
SCIENCE CITATION INDEX EXPANDED - JOURNAL LIST Total journals: 8631 1. 4OR-A QUARTERLY JOURNAL OF OPERATIONS RESEARCH 2. AAPG BULLETIN 3. AAPS JOURNAL 4. AAPS PHARMSCITECH 5. AATCC REVIEW 6. ABDOMINAL IMAGING 7. ABHANDLUNGEN AUS DEM MATHEMATISCHEN SEMINAR DER UNIVERSITAT HAMBURG 8. ABSTRACT AND APPLIED ANALYSIS 9. ABSTRACTS OF PAPERS OF THE AMERICAN CHEMICAL SOCIETY 10. ACADEMIC EMERGENCY MEDICINE 11. ACADEMIC MEDICINE 12. ACADEMIC PEDIATRICS 13. ACADEMIC RADIOLOGY 14. ACCOUNTABILITY IN RESEARCH-POLICIES AND QUALITY ASSURANCE 15. ACCOUNTS OF CHEMICAL RESEARCH 16. ACCREDITATION AND QUALITY ASSURANCE 17. ACI MATERIALS JOURNAL 18. ACI STRUCTURAL JOURNAL 19. ACM COMPUTING SURVEYS 20. ACM JOURNAL ON EMERGING TECHNOLOGIES IN COMPUTING SYSTEMS 21. ACM SIGCOMM COMPUTER COMMUNICATION REVIEW 22. ACM SIGPLAN NOTICES 23. ACM TRANSACTIONS ON ALGORITHMS 24. ACM TRANSACTIONS ON APPLIED PERCEPTION 25. ACM TRANSACTIONS ON ARCHITECTURE AND CODE OPTIMIZATION 26. ACM TRANSACTIONS ON AUTONOMOUS AND ADAPTIVE SYSTEMS 27. ACM TRANSACTIONS ON COMPUTATIONAL LOGIC 28. ACM TRANSACTIONS ON COMPUTER SYSTEMS 29. ACM TRANSACTIONS ON COMPUTER-HUMAN INTERACTION 30. ACM TRANSACTIONS ON DATABASE SYSTEMS 31. ACM TRANSACTIONS ON DESIGN AUTOMATION OF ELECTRONIC SYSTEMS 32. ACM TRANSACTIONS ON EMBEDDED COMPUTING SYSTEMS 33. ACM TRANSACTIONS ON GRAPHICS 34. ACM TRANSACTIONS ON INFORMATION AND SYSTEM SECURITY 35. ACM TRANSACTIONS ON INFORMATION SYSTEMS 36. ACM TRANSACTIONS ON INTELLIGENT SYSTEMS AND TECHNOLOGY 37. ACM TRANSACTIONS ON INTERNET TECHNOLOGY 38. ACM TRANSACTIONS ON KNOWLEDGE DISCOVERY FROM DATA 39. ACM TRANSACTIONS ON MATHEMATICAL SOFTWARE 40. ACM TRANSACTIONS ON MODELING AND COMPUTER SIMULATION 41. ACM TRANSACTIONS ON MULTIMEDIA COMPUTING COMMUNICATIONS AND APPLICATIONS 42. ACM TRANSACTIONS ON PROGRAMMING LANGUAGES AND SYSTEMS 43. ACM TRANSACTIONS ON RECONFIGURABLE TECHNOLOGY AND SYSTEMS 44. -

0 WILEY and MAYNOOTH UNIVERSITY WILEY READ AND
WILEY and MAYNOOTH UNIVERSITY ________________________________________ WILEY READ AND PUBLISH AGREEMENT ________________________________________ 0 THIS AGREEMENT is made on the 15th day of March, 2021 BETWEEN: John Wiley & Sons, Inc., a New York corporation, 111 River Street, Hoboken, New Jersey 07030, and its affiliates Wiley Periodicals LLC, John Wiley & Sons, Ltd, John Wiley & Sons Australia, Ltd, Wiley-VCH GmbH, John Wiley & Sons A/S, collectively “Wiley” or “Publisher” AND National University of Ireland Maynooth, Maynooth University, whose principal address is at Maynooth, Co Kildare, Ireland (“Maynooth University”), acting on its own behalf and as non-exclusive agent on behalf of the other Members of the Consortium. RECITALS WHEREAS Maynooth University has been appointed by Members of the Consortium, as their non-exclusive agent, to enter into agreements on the Members’ behalf for accessing electronic educational and research resources; AND WHEREAS the Publisher provides Wiley Online Library which is an electronic collection of online journals, books, and research resources, covering life, health, social, and physical sciences, and the Publishing Privilege that gives authors the option to publish articles on an open access basis in select Wiley journals.; AND WHEREAS Maynooth University wishes to enter into this Agreement in order for Members of the Consortium to be authorised to access and use the Licensed Material; AND WHEREAS the Consortium and the Publisher share the goal to transition to an open access model and the transition to full open access will include continued access to the Publisher’s journal content, AND WHEREAS the parties are desirous to contract on the basis of the terms and conditions of this Agreement. -

Novartis Chemistry Lectureship 20112012
Angewandte. Angewandte News Chemie Novartis Chemistry Lectureship Barcelona, and was appointed professor there in 2011–2012 1986. Giralt is a member of the Editorial Advisory Awarded … Boards of ChemBioChem and Chemistry Open, and The Novartis Chemistry Lectureship is awarded to the International Advisory Boards of Chemistry— scientists in recognition of outstanding contribu- An Asian Journal and ChemMedChem. Giralts tions to organic and computational chemistry, research interests are in the fields of peptide including applications to biology. We congratulate synthesis, molecular recognition, and structure the recipients featured here, as well as Daniel determination, in particular using NMR spectros- Kahne (Harvard University) and Melanie S. San- copy. He has reported on 15N relaxation NMR ford (University of Michigan), who was recently studies of prolyl oligopeptidase in ChemBio- featured in this section.[1] Chem,[4a] and has discussed shuttle-mediated drug Yujiro Hayashi (Tokyo University of Science) delivery to the brain in a Review in Angewandte studied at Tokyo University and was awarded his Chemie.[4b] PhD in 1992 for work supervised by Koichi Tomislav Rovis (Colorado State University, Narasaka. He was a postdoctoral fellow with Fort Collins, USA) studied at the University of Y. Hayashi Elias J. Corey at Harvard University from 1994– Toronto, and earned his PhD in 1998 directed by 1996, and has been full professor at Tokyo Uni- Mark Lautens. From 1998–2000, he was a postdoc- versity of Science since 2006. Hayashi is on the toral fellow with David A. Evans at Harvard Academic Advisory Board of Advanced Synthesis University, and in 2000, he joined the faculty of & Catalysis and the International Advisory Board Colorado State University, where he currently of the European Journal of Organic Chemistry. -

David Peralta (Editor-In-Chief, Chemmedchem, a Chemistry Europe Journal)
Lecture Title: Publishing Ethics: Best practices in writing manuscripts Speaker: David Peralta (Editor-in-Chief, ChemMedChem, A Chemistry Europe Journal) Abstract: What constitutes plagiarism? To what extent is graphic optimization allowed? How do I properly cite other work? How should authorship be determined? What graphics/data from other papers can I use in my own manuscript? If you've had such questions, this talk is for you. We'll discuss ethical guidelines within the world of scientific publishing. We'll go through some of the most important rules students and professors should remember to make sure their research is written, published, and shared in an ethical manner. As such, we'll look at some examples of the most common unethical practices and also discuss what the repercussions are when such violations occur. We'll also explain how one can quickly and legally share one's published output. David Peralta studied chemistry and German culture and language at the Ateneo de Manila University, Philippines (BSc Chem 2006, MSc Chem 2009). There, he taught various courses in chemistry and science and society while finishing his MSc degree, focusing on organic, analytical, and biochemistry. In 2009, he moved to Germany for his PhD at the German Cancer Research Center (DKFZ), in the research group of Prof. Tobias Dick, working on redox biochemistry. In 2015, he earned his Dr. rer. nat. in biosciences/biochemistry from the DKFZ and the Ruprecht-Karls-Universität Heidelberg. Shortly before his doctoral defense, he joined Wiley-VCH in 2014 as an Assistant Editor for both ChemMedChem and ChemistryOpen, and later also ChemistrySelect. -
YEARBOOK 2021 | 1 Editorial
EFMC Yearbook 2021 Medicinal Chemistry and Chemical Biology in Europe EFMC-ISMC International Symposium on Medicinal Chemistry Virtual Event Aug. 29-Sept. 2, 2021 SESSIONS AND SESSION NEXT GENERATION DRUGS FOR HEART CONFIRMED PLENARY LECTURES COORDINATORS FAILURE Alleyn Plowright, Wren Therapeutics, UK Phil Baran, The Scripps Research Institute, US CHEMICAL BIOLOGY Karin Briner, Novartis, US RECENT ADVANCES IN ANTICANCER DRUG Jean-Paul Clozel, Idorsia, CH CARBOHYDRATE RECOGNITION AND DRUG DISCOVERY Stefan Knapp, Goethe University Frankfurt, DE DESIGN Roberto di Santo, Sapienza University of Rome, IT Alexander Titz, Helmholtz Institute for Pharmaceutical Sciences, DE TARGETING FIBROTIC DISEASES WITH SMALL MOLECULES EFMC AWARD LECTURES CHEMICAL APPROACHES TO STEM CELL Boehringer Ingelheim, DE DIFFERENTIATION (ICBS Session) THE NAUTA PHARMACOCHEMISTRY AWARD Colin Pouton, Monash University, AU TISSUE AND CELL SPECIFIC DRUG DELIVERY FOR MEDICINAL CHEMISTRY AND CHEMICAL (EUFEPS Session) BIOLOGY CHEMICAL PROBES FOR TARGET DISCOVERY Sébastien Papot, University of Poitiers, FR Ad P. Ijzerman, Leiden University, NL AND VALIDATION Gyorgy Keseru, Hungarian Academy of Sciences, HU TECHNOLOGIES IN MEDICINAL CHEMISTRY MOLECULAR IMAGING TOOLS FOR CHEMICAL Malin Lemurell, AstraZeneca, SE BIOLOGY APPLICATION OF ARTIFICIAL INTELLIGENCE Valle Palomo, CIB, ES IN DRUG DISCOVERY PROJECTS Christopher Swain, Cambridge MedChem AWARD FOR NEW TECHNOLOGIES IN DRUG PHOTOCHEMISTRY IN DRUG DISCOVERY: Consulting, UK DISCOVERY PHOTOPHARMACOLOGY, PHOTOTOXICITY Gisbert Schneider, ETH Zürich, CH AND SYNTHESIS (ACSMEDI Session) BIOCATALYSIS & LATE STAGE Timothy Henderson, MSD, US & Amjad Ali, MSD, US FUNCTIONALISATION Radka Snajdrova, Novartis, CH EFMC PARTNER PRIZES SMALL MOLECULES TARGETING RNA FUNCTION AND PROCESSING Maria Duca, University of Côte d'Azur, FR Jean-Paul Renaud, Urania Therapeutics, FR John E. Macor, Sanofi, US TARGET DECONVOLUTION STRATEGIES IN THE KLAUS GROHE AWARD DRUG DISCOVERY EXPANDING CHEMICAL SPACE THROUGH Stephan A. -
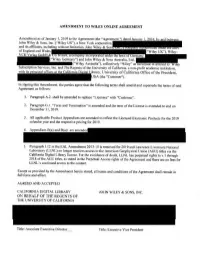
On Behalf of the Regents of the University of California
AMENllMENT TO WILEY ONLINE AGREEMENT Amendment as of January 1, 2019 to the Agreement (the " Agreement " John Wi ley & Sons, Jnc. ("Wiley US"), a New York corporation, and its affiliates, including without limitation, John Wiley & Son of England and Wales, VCH Verla GmbH & o. a , a company mcorporate un er l 1e aws o ("Wiley Germany") and John Wiley & Sons Australia, Ltd., (.. Wiley Australia"), collectively ''Wiley" as successor m interest to I ey Subscription Services, Inc. and The Regents of the University of California, a non-profit academic institution, with its rinci al offices at !he California Di ital Library, University of California Office of the President, SA (the "Customer"). In signing this Amendment, the parties agree that the following terms shall amend and supersede the tenns of said Agreement as follows: I. Paragraph A.2. shall be amended to replace "Licensee" with "Customer''. 2. Paragraph G. I. "Term and Termination" is amended and the tenn of the License is extended to end on December 31, 2019. 3. All applicable Product Appendices are amended to reflect the Licensed Electronic Products for the 201 9 calendar year and the respective pricing for 2019. 5. Paragraph J.12 in the EAL Amendment 2013-15 is removed for 2019 and Lawrence Livermore National Laboratory (LLNL) no longer receives access to the American Geophysical Union (AGU) titles via the California Digital Library license. For the avoidance of doubt, LLNL has perpetual rights to v. I through 2018 of the AGU titles, as stated in the Perpetual Access rights of the Agreement and there are no fees for LLNL's continued access lo the content. -

Spotlights on Our Sister Journals: Chem. Asian J. 10/2016
On these pages, we feature aselection computer,click on any of the items to of the excellent work that has recently read the full article. Otherwise please been published in our sister journals. see the DOIs for easy online access If you are reading these pages on a through Wiley Online Library. Anion Recognition M. Albrecht,* H. Yi,O.Kçksal, G. Raabe, F. Pan, A. Valkonen, K. Rissanen CF3:AnElectron-Withdrawing Substituent for Aromatic Anion Acceptors?“Side-On” versus“On-Top” Binding of Halides The place to be! Asubtle interplay of electronic effects at the aro- matic system and at aromatic Hatoms in connection with the polar- izability of the anion controlsthe position of anions in respecttoCF3 substituted aromatics. Chem. Eur.J. DOI: 10.1002/chem.201600249 Protein-Protein Interactions A. López, F. Herranz-Trillo, M. Kotev,M.Gairí, V. Guallar,P.Bernadó, O. Millet, T. Tarragó, E. Giralt* Active-Site-DirectedInhibitors of Prolyl Oligopeptidase Abolish Its Conformational Dynamics Aspoke on the wheels:Acombined approach based on NMR and SAXS experiments complemented by MD simulations has shown that active-site-directed inhibitors of prolyl oligopeptidase (POP) abolish the open/closed conformationalequilibrium. Probably,abol- ishing conformational dynamics by inhibitors causes significant alter- ations to molecular recognition events of POP. ChemBioChem DOI: 10.1002/cbic.201600102 Nanocrystals N. Pradhan* Red-Tuned Mn d–d Emission in Doped Semiconductor Nanocrystals Iprefer it in red:Emissiontuned from yellow to red can be ob- tained from Mn2+-doped semiconductor nanocrystals. By changing the environmentofthe Mn dopant in the crystal lattice,the Mn con- centration and the surfaceligands,the ligand-field splitting, and ChemPhysChem therefore also the Mn d–d emission, can be tuned. -

Detailled CV
Detailed CV Birth: December 6, 1940, St. Ulrich, Italy Marital status: married with Anne Marie Hellrigl, 1 child Address: Max-Planck-Institute of Biochemistry Bioorganic Chemistry Am Klopferspitz 18 D-82152 Martinsried Tel: +49-(0)89 / 8578-3905; [email protected]; www.biochem.mpg.de/en/rg/moroder/ Academic education 1959 - 1965 Chemistry at the University of Padova, Italy; graduate training in peptide chemistry in the laboratories of Prof. E. Scoffone 1965: Doctorate in Chemistry with summa cum laude: On the synthesis of the N-terminal eicosapeptide of ribonuclease A. Professional activities 1965 - 1967 Research assistant at the Institute of Organic Chemistry, University of Padova, Italy. 1968 - 1969 Research associate at the Protein Research Laboratory (Prof. K. Hofmann), University of Pittsburgh. 1975 - 1991 Staff scientist at the Max-Planck-Institute of Biochemistry, Department of Peptide Chemistry, Martinsried, Germany. 1971 Habilitation in Chemistry of Natural Products, Padova, Italy 1988 Habilitation at the Technical University of Munich, Faculty of Chemistry, Biology and Geology. 1990 Visiting Professor, Protein Research Institute, University of Osaka, Japan 1991- Head of the Laboratory of Bioorganic Chemistry, Institute of Biochemistry, Martinsried, Germany. 1992 Visiting Professor, University of Padova, Italy 1994- Apl. Professor, Technical University of Munich 1997 Visiting Professor, University of Neaples 1997-1998 Professor of Biochemistry and Biotechnology, TU München Awards 1995 Max-Bergmann-Medal 2004 Josef Rudinger Award 2008 Dimitrios Theodoropoulos Memorial Lecturer 2011 Doctor honoris causa, University of Cergy-Pontoise, Paris 2018 Akabori Memorial Award 2018 2020 Ernesto Scoffone Award Author and coauthor of 669 publications (491 in peer-reviewed journals and 178 as contributions to proceedings and books) Co-Editor of the 5-volume treatise Houben-Weyl, Methods of Organic Chemistry, Synthesis of Peptides and Peptidomimetics (Goodman, M.; Felix, A.; Moroder, L.; Toniolo, C., eds.) E 22a-e, Georg Thieme Verlag, Stuttgart, 2002/2003. -

Source Publication List for Web of Science
SOURCE PUBLICATION LIST FOR WEB OF SCIENCE SCIENCE CITATION INDEX EXPANDED Updated July 2017 Journal Title Publisher ISSN E-ISSN Country Language 2D Materials IOP PUBLISHING LTD 2053-1583 2053-1583 ENGLAND English 3 Biotech SPRINGER HEIDELBERG 2190-572X 2190-5738 GERMANY English 3D Printing and Additive Manufacturing MARY ANN LIEBERT, INC 2329-7662 2329-7670 UNITED STATES English 4OR-A Quarterly Journal of Operations Research SPRINGER HEIDELBERG 1619-4500 1614-2411 GERMANY English AAPG BULLETIN AMER ASSOC PETROLEUM GEOLOGIST 0149-1423 1558-9153 UNITED STATES English AAPS Journal SPRINGER 1550-7416 1550-7416 UNITED STATES English AAPS PHARMSCITECH SPRINGER 1530-9932 1530-9932 UNITED STATES English AATCC Journal of Research AMER ASSOC TEXTILE CHEMISTS COLORISTS-AATCC 2330-5517 2330-5517 UNITED STATES English AATCC REVIEW AMER ASSOC TEXTILE CHEMISTS COLORISTS-AATCC 1532-8813 1532-8813 UNITED STATES English Abdominal Radiology SPRINGER 2366-004X 2366-0058 UNITED STATES English ABHANDLUNGEN AUS DEM MATHEMATISCHEN SEMINAR DER UNIVERSITAT HAMBURG SPRINGER HEIDELBERG 0025-5858 1865-8784 GERMANY German ABSTRACTS OF PAPERS OF THE AMERICAN CHEMICAL SOCIETY AMER CHEMICAL SOC 0065-7727 UNITED STATES English Academic Pediatrics ELSEVIER SCIENCE INC 1876-2859 1876-2867 UNITED STATES English Accountability in Research-Policies and Quality Assurance TAYLOR & FRANCIS LTD 0898-9621 1545-5815 UNITED STATES English Acoustics Australia SPRINGER 1839-2571 1839-2571 AUSTRALIA English Acta Bioethica UNIV CHILE, CENTRO INTERDISCIPLINARIO ESTUDIOS BIOETICA 1726-569X