Androgen and Prostate Cancer: Is the Hypothesis Dead?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
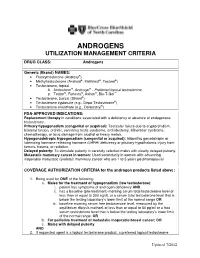
Androgens Utilization Management Criteria
ANDROGENS UTILIZATION MANAGEMENT CRITERIA DRUG CLASS: Androgens Generic (Brand) NAMES: • Fluoxymesterone (Androxy®) • Methyltestosterone (Android®, Methitest®, Testred®) • Testosterone, topical A. Androderm®, Androgel® - Preferred topical testosterone ® ® ® ™ B. Testim , Fortesta , Axiron , Bio-T-Gel • Testosterone, buccal (Striant®) • Testosterone cypionate (e.g., Depo-Testosterone®) • Testosterone enanthate (e.g., Delatestryl®) FDA-APPROVED INDICATIONS: Replacement therapy in conditions associated with a deficiency or absence of endogenous testosterone. Primary hypogonadism (congenital or acquired): Testicular failure due to cryptorchidism, bilateral torsion, orchitis, vanishing testis syndrome, orchidectomy, Klinefelter syndrome, chemotherapy, or toxic damage from alcohol or heavy metals. Hypogonadotropic hypogonadism (congenital or acquired): Idiopathic gonadotropin or luteinizing hormone-releasing hormone (LHRH) deficiency or pituitary-hypothalamic injury from tumors, trauma, or radiation. Delayed puberty: To stimulate puberty in carefully selected males with clearly delayed puberty. Metastatic mammary cancer in women: Used secondarily in women with advancing inoperable metastatic (skeletal) mammary cancer who are 1 to 5 years postmenopausal COVERAGE AUTHORIZATION CRITERIA for the androgen products listed above: 1. Being used for ONE of the following: a. Males for the treatment of hypogonadism (low testosterone): i. patient has symptoms of androgen deficiency AND ii. has a baseline (pre-treatment) morning serum total testosterone level of less than or equal to 300 ng/dL or a serum total testosterone level that is below the testing laboratory’s lower limit of the normal range OR iii. baseline morning serum free testosterone level, measured by the equilibrium dialysis method, of less than or equal to 50 pg/ml or a free serum testosterone level that is below the testing laboratory’s lower limit of the normal range, OR b. -

CASODEX (Bicalutamide)
HIGHLIGHTS OF PRESCRIBING INFORMATION • Gynecomastia and breast pain have been reported during treatment with These highlights do not include all the information needed to use CASODEX 150 mg when used as a single agent. (5.3) CASODEX® safely and effectively. See full prescribing information for • CASODEX is used in combination with an LHRH agonist. LHRH CASODEX. agonists have been shown to cause a reduction in glucose tolerance in CASODEX® (bicalutamide) tablet, for oral use males. Consideration should be given to monitoring blood glucose in Initial U.S. Approval: 1995 patients receiving CASODEX in combination with LHRH agonists. (5.4) -------------------------- RECENT MAJOR CHANGES -------------------------- • Monitoring Prostate Specific Antigen (PSA) is recommended. Evaluate Warnings and Precautions (5.2) 10/2017 for clinical progression if PSA increases. (5.5) --------------------------- INDICATIONS AND USAGE -------------------------- ------------------------------ ADVERSE REACTIONS ----------------------------- • CASODEX 50 mg is an androgen receptor inhibitor indicated for use in Adverse reactions that occurred in more than 10% of patients receiving combination therapy with a luteinizing hormone-releasing hormone CASODEX plus an LHRH-A were: hot flashes, pain (including general, back, (LHRH) analog for the treatment of Stage D2 metastatic carcinoma of pelvic and abdominal), asthenia, constipation, infection, nausea, peripheral the prostate. (1) edema, dyspnea, diarrhea, hematuria, nocturia, and anemia. (6.1) • CASODEX 150 mg daily is not approved for use alone or with other treatments. (1) To report SUSPECTED ADVERSE REACTIONS, contact AstraZeneca Pharmaceuticals LP at 1-800-236-9933 or FDA at 1-800-FDA-1088 or ---------------------- DOSAGE AND ADMINISTRATION ---------------------- www.fda.gov/medwatch The recommended dose for CASODEX therapy in combination with an LHRH analog is one 50 mg tablet once daily (morning or evening). -

COVID-19—The Potential Beneficial Therapeutic Effects of Spironolactone During SARS-Cov-2 Infection
pharmaceuticals Review COVID-19—The Potential Beneficial Therapeutic Effects of Spironolactone during SARS-CoV-2 Infection Katarzyna Kotfis 1,* , Kacper Lechowicz 1 , Sylwester Drozd˙ zal˙ 2 , Paulina Nied´zwiedzka-Rystwej 3 , Tomasz K. Wojdacz 4, Ewelina Grywalska 5 , Jowita Biernawska 6, Magda Wi´sniewska 7 and Miłosz Parczewski 8 1 Department of Anesthesiology, Intensive Therapy and Acute Intoxications, Pomeranian Medical University in Szczecin, 70-111 Szczecin, Poland; [email protected] 2 Department of Pharmacokinetics and Monitored Therapy, Pomeranian Medical University, 70-111 Szczecin, Poland; [email protected] 3 Institute of Biology, University of Szczecin, 71-412 Szczecin, Poland; [email protected] 4 Independent Clinical Epigenetics Laboratory, Pomeranian Medical University, 71-252 Szczecin, Poland; [email protected] 5 Department of Clinical Immunology and Immunotherapy, Medical University of Lublin, 20-093 Lublin, Poland; [email protected] 6 Department of Anesthesiology and Intensive Therapy, Pomeranian Medical University in Szczecin, 71-252 Szczecin, Poland; [email protected] 7 Clinical Department of Nephrology, Transplantology and Internal Medicine, Pomeranian Medical University, 70-111 Szczecin, Poland; [email protected] 8 Department of Infectious, Tropical Diseases and Immune Deficiency, Pomeranian Medical University in Szczecin, 71-455 Szczecin, Poland; [email protected] * Correspondence: katarzyna.kotfi[email protected]; Tel.: +48-91-466-11-44 Abstract: In March 2020, coronavirus disease 2019 (COVID-19) caused by SARS-CoV-2 was declared Citation: Kotfis, K.; Lechowicz, K.; a global pandemic by the World Health Organization (WHO). The clinical course of the disease is Drozd˙ zal,˙ S.; Nied´zwiedzka-Rystwej, unpredictable but may lead to severe acute respiratory infection (SARI) and pneumonia leading to P.; Wojdacz, T.K.; Grywalska, E.; acute respiratory distress syndrome (ARDS). -

Adverse Effects of Anabolic-Androgenic Steroids: a Literature Review
healthcare Review Adverse Effects of Anabolic-Androgenic Steroids: A Literature Review Giuseppe Davide Albano 1,†, Francesco Amico 1,†, Giuseppe Cocimano 1, Aldo Liberto 1, Francesca Maglietta 2, Massimiliano Esposito 1, Giuseppe Li Rosi 3, Nunzio Di Nunno 4, Monica Salerno 1,‡ and Angelo Montana 1,*,‡ 1 Legal Medicine, Department of Medical, Surgical and Advanced Technologies, “G.F. Ingrassia”, University of Catania, 95123 Catania, Italy; [email protected] (G.D.A.); [email protected] (F.A.); [email protected] (G.C.); [email protected] (A.L.); [email protected] (M.E.); [email protected] (M.S.) 2 Department of Clinical and Experimental Medicine, University of Foggia, 71122 Foggia, Italy; [email protected] 3 Department of Law, Criminology, Magna Graecia University of Catanzaro, 88100 Catanzaro, Italy; [email protected] 4 Department of History, Society and Studies on Humanity, University of Salento, 73100 Lecce, Italy; [email protected] * Correspondence: [email protected]; Tel.: +39-095-3782153 † These authors contributed equally to this work. ‡ These authors share last authorship. Abstract: Anabolic-androgenic steroids (AASs) are a large group of molecules including endoge- nously produced androgens, such as testosterone, as well as synthetically manufactured derivatives. AAS use is widespread due to their ability to improve muscle growth for aesthetic purposes and athletes’ performance, minimizing androgenic effects. AAS use is very popular and 1–3% of US inhabitants have been estimated to be AAS users. However, AASs have side effects, involving all organs, tissues and body functions, especially long-term toxicity involving the cardiovascular system Citation: Albano, G.D.; Amico, F.; and the reproductive system, thereby, their abuse is considered a public health issue. -

Steroid Sulfatase Stimulates Intracrine Androgen Synthesis and Is a Therapeutic Target for Advanced Prostate Cancer
Author Manuscript Published OnlineFirst on September 14, 2020; DOI: 10.1158/1078-0432.CCR-20-1682 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Steroid sulfatase stimulates intracrine androgen synthesis and is a therapeutic target for advanced prostate cancer Cameron M. Armstrong1*, Chengfei Liu1*, Liangren Liu1,2*, Joy C. Yang1, Wei Lou1, Ruining Zhao1,3, Shu Ning1, Alan P. Lombard1, Jinge Zhao1, Leandro S D'Abronzo1, Christopher P. Evans1,4, Pui-Kai Li5, Allen C. Gao1, 4, 6,7 Running title: Targeting steroid sulfatase for advanced prostate cancer Key words: Prostate cancer, steroid sulfatase, resistance, intracrine androgen synthesis, adrenal androgens 1Department of Urologic Surgery, University of California Davis, CA, USA 2Present address: Department of Urology, West China Hospital, Sichuan University, China 3Present address: Department of Urology, General Hospital of Ningxia Medical University, China 4UC Davis Comprehensive Cancer Center, University of California Davis, CA, USA 5Division of Medicinal Chemistry and Pharmacognosy, College of Pharmacy, The Ohio State University, Columbus, OH, USA 6VA Northern California Health Care System, Sacramento, CA, USA 7Corresponding author: Allen Gao, University of California Davis, 4645 2nd Avenue, Sacramento, CA 95817, USA. Phone: 916-734-8718, email: [email protected] *These authors contributed equally to the work. Conflict of interest: PKL and ACG are co-inventors of a patent application of the selected small molecule inhibitors of steroid sulfatase. 1 Downloaded from clincancerres.aacrjournals.org on October 1, 2021. © 2020 American Association for Cancer Research. Author Manuscript Published OnlineFirst on September 14, 2020; DOI: 10.1158/1078-0432.CCR-20-1682 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. -

Steroids and Other Appearance and Performance Enhancing Drugs (Apeds) Research Report
Research Report Revised Febrero 2018 Steroids and Other Appearance and Performance Enhancing Drugs (APEDs) Research Report Table of Contents Steroids and Other Appearance and Performance Enhancing Drugs (APEDs) Research Report Introduction What are the different types of APEDs? What is the history of anabolic steroid use? Who uses anabolic steroids? Why are anabolic steroids misused? How are anabolic steroids used? What are the side effects of anabolic steroid misuse? How does anabolic steroid misuse affect behavior? What are the risks of anabolic steroid use in teens? How do anabolic steroids work in the brain? Are anabolic steroids addictive? How are anabolic steroids tested in athletes? What can be done to prevent steroid misuse? What treatments are effective for anabolic steroid misuse? Where can I get further information about steroids? References Page 1 Steroids and Other Appearance and Performance Enhancing Drugs (APEDs) Research Report Esta publicación está disponible para su uso y puede ser reproducida, en su totalidad, sin pedir autorización al NIDA. Se agradece la citación de la fuente, de la siguiente manera: Fuente: Instituto Nacional sobre el Abuso de Drogas; Institutos Nacionales de la Salud; Departamento de Salud y Servicios Humanos de los Estados Unidos. Introduction Appearance and performance enhancing drugs (APEDs) are most often used by males to improve appearance by building muscle mass or to enhance athletic performance. Although they may directly and indirectly have effects on a user’s mood, they do not produce a euphoric high, which makes APEDs distinct from other drugs such as cocaine, heroin, and marijuana. However, users may develop a substance use disorder, defined as continued use despite adverse consequences. -

Receptor Af®Nity and Potency of Non-Steroidal Antiandrogens: Translation of Preclinical ®Ndings Into Clinical Activity
Prostate Cancer and Prostatic Diseases (1998) 1, 307±314 ß 1998 Stockton Press All rights reserved 1365±7852/98 $12.00 http://www.stockton-press.co.uk/pcan Review Receptor af®nity and potency of non-steroidal antiandrogens: translation of preclinical ®ndings into clinical activity GJCM Kolvenbag1, BJA Furr2 & GRP Blackledge3 1Medical Affairs, Zeneca Pharmaceuticals, Wilmington, DE, USA; 2Therapeutic Research Department, and 3Medical Research Department, Zeneca Pharmaceuticals, Alderley Park, Maccles®eld, Cheshire, UK The non-steroidal antiandrogens ¯utamide (Eulexin1), nilutamide (Anandron1) and bicalutamide (Casodex1) are widely used in the treatment of advanced prostate cancer, particularly in combination with castration. The naturally occurring ligand 5a-DHT has higher binding af®nity at the androgen receptor than the non-steroidal antiandrogens. Bicalutamide has an af®nity two to four times higher than 2-hydroxy¯utamide, the active metabolite of ¯utamide, and around two times higher than nilutamide for wild-type rat and human prostate androgen receptors. Animal studies have indicated that bicalutamide also exhi- bits greater potency in reducing seminal vesicle and ventral prostate weights and inhibiting prostate tumour growth than ¯utamide. Although preclinical data can give an indication of the likely clinical activity, clinical studies are required to determine effective, well-tolerated dosing regimens. As components of combined androgen blockade (CAB), controlled studies have shown survival bene®ts of ¯utamide plus a luteinising hormone-releasing hormone analogue (LHRH-A) over LHRH-A alone, and for nilutamide plus orchiectomy over orchiectomy alone. Other studies have failed to show such survival bene®ts, including those comparing ¯utamide plus orchiectomy with orchiectomy alone, and nilutamide plus LHRH-A with LHRH-A alone. -

Sex Steroids in Androgen-Secreting Adrenocortical Tumors
European Journal of Endocrinology (2008) 159 641–647 ISSN 0804-4643 CLINICAL STUDY Sex steroids in androgen-secreting adrenocortical tumors: clinical and hormonal features in comparison with non-tumoral causes of androgen excess Catarina B d’Alva1, Gwenaelle Abiven-Lepage1,2, Vivian Viallon2,3, Lionel Groussin1,2,4, Marie Annick Dugue2,5, Xavier Bertagna1,2,4,6 and Jeroˆme Bertherat1,2,4,7 1Assistance Publique-Hoˆpitaux de Paris, Hoˆpital Cochin, Service d’Endocrinologie, Paris, France, 2Universite´ Paris Descartes, Paris, France, 3Assistance Publique-Hoˆpitaux de Paris, Hoˆpital Cochin, Service de Biostatistiques, Paris, France, 4INSERM U 567, CNRS UMR 8104, Institut Cochin, Paris, France, 5Assistance Publique-Hoˆpitaux de Paris, Hoˆpital Cochin, Service d’Hormonologie, Paris, France, 6Adrenal Cancer INCa-COMETE Network, Paris, France and 7Center for Rare Adrenal Diseases, Hoˆpital Cochin, Paris, France (Correspondence should be addressed to J Bertherat at Service d’Endocrinologie, Hoˆpital Cochin, 27, rue du Faubourg Saint-Jacques, 75014 Paris, France; Email: [email protected]) Abstract Objective: Adrenocortical tumors (ACT) account for no more than 0.2% of the causes of androgen excess (AE). Conversely, these rare tumors have a very poor prognosis. It is difficult and important to exclude this diagnosis whenever there is AE. Design: Retrospective investigation of androgen profiles in a large consecutive series of androgen- secreting (AS) ACT to assess their relative diagnostic value. Methods: A total of 44 consecutive female patients with ACT-AS and a comparison group of 102 women with non-tumor causes of AE (NTAE). Results: Patients with ACT-AS were older than the ones with NTAE (37.7 vs 24.8 years; P!0.001) and the prevalence of hirsutism, acne, and oligo/amenorrhea were not different. -

Androgen (Testosterone) Deficiency
FFactact Sheet Androgen (Testosterone) Deficiency What are androgens? Hormones are chemical messengers made by glands in the body that are carried in the blood to act on other organs in the body. Hormones are needed for growth, reproduction and well-being. 2 hormones from the pituitary - e n Luteinising (LH) and Follicle o Stimulating (FSH) - act on the r Androgens are male sex hormones that increase at e t testis to stimulate production s o puberty and are needed for a boy to develop into of testosterone and sperm. t s e a sexually mature adult who can reproduce. The T most important androgen is testosterone. 2 hormones from the pituitary - e n Luteinising (LH) and Follicle o Stimulating (FSH) - act on the r What is testosterone? e t testis to stimulate production s o Testosterone is the most important androgen of testosterone and sperm. t s e (male sex hormone) in men and it is needed T for normal reproductive and sexual function. Testosterone is important for the physical changes that happen during male puberty, such as development of the penis and testes, and for the Hypothalamus features typical of adult men such as facial and Pituitary body hair and a masculine physique. Testosterone also acts on cells in the testes to make sperm. Testis Testosterone is also important for overall good health. It helps the growth of bones and muscles, and affects mood and libido (sex drive). Some testosterone is changed into oestrogen, the female How do hormones control the testes? sex hormone, and this is important for bone health in men. -

Product Monograph Casodex®
PRODUCT MONOGRAPH Pr CASODEX® bicalutamide tablets 50mg Tablets Non-Steroidal Antiandrogen AstraZeneca Canada Inc. Date of Revision: 1004 Middlegate Road July 13, 2017 Mississauga, Ontario L4Y 1M4 www.astrazeneca.ca Control No. 205811 CASODEX® is a registered trademark of AstraZeneca UK Limited, used under license by AstraZeneca Canada Inc. COPYRIGHT 1995-2017 ASTRAZENECA CANADA INC. Page 1 of 32 TABLE OF CONTENTS TABLE OF CONTENTS .........................................................................................................2 PART I: HEALTH PROFESSIONAL INFORMATION .......................................................3 SUMMARY PRODUCT INFORMATION......................................................................3 INDICATIONS AND CLINICAL USE ...........................................................................3 CONTRAINDICATIONS.................................................................................................3 WARNINGS AND PRECAUTIONS ...............................................................................4 ADVERSE REACTIONS .................................................................................................8 DRUG INTERACTIONS ...............................................................................................12 DOSAGE AND ADMINISTRATION ...........................................................................13 OVERDOSAGE..............................................................................................................14 ACTION AND CLINICAL PHARMACOLOGY..........................................................14 -

Nandrolone Induces a Stem Cell-Like Phenotype in Human
www.nature.com/scientificreports OPEN Nandrolone induces a stem cell-like phenotype in human hepatocarcinoma-derived cell line inhibiting mitochondrial respiratory activity Francesca Agriesti 1, Tiziana Tataranni1, Consiglia Pacelli2, Rosella Scrima2, Ilaria Laurenzana1, Vitalba Ruggieri1, Olga Cela2, Carmela Mazzoccoli1, Monica Salerno3, Francesco Sessa2, Gabriele Sani4,5, Cristoforo Pomara3, Nazzareno Capitanio2 & Claudia Piccoli 1,2* Nandrolone is a testosterone analogue with anabolic properties commonly abused worldwide, recently utilized also as therapeutic agent in chronic diseases, cancer included. Here we investigated the impact of nandrolone on the metabolic phenotype in HepG2 cell line. The results attained show that pharmacological dosage of nandrolone, slowing cell growth, repressed mitochondrial respiration, inhibited the respiratory chain complexes I and III and enhanced mitochondrial reactive oxygen species (ROS) production. Intriguingly, nandrolone caused a signifcant increase of stemness-markers in both 2D and 3D cultures, which resulted to be CxIII-ROS dependent. Notably, nandrolone negatively afected diferentiation both in healthy hematopoietic and mesenchymal stem cells. Finally, nandrolone administration in mice confrmed the up-regulation of stemness-markers in liver, spleen and kidney. Our observations show, for the frst time, that chronic administration of nandrolone, favoring maintenance of stem cells in diferent tissues would represent a precondition that, in addition to multiple hits, might enhance risk of carcinogenesis raising warnings about its abuse and therapeutic utilization. Nandrolone (ND), a synthetic testosterone analogue, is one of the most commonly abused anabolic androgenic steroids (AAS) worldwide. For its improved anabolic properties ND is widely clinically applied in treatment of chronic diseases associated with catabolic state such as burns, cornea healing and osteoporosis1. -

Disposition and Metabolic Profile of the Weak Androgen
APPLIED MEDICINE: CLINICAL PATHOLOGY AND DERMATOLOGY Disposition and Metabolic Profile of the Weak Androgen Dehydroepiandrosterone After Administration as Part of a Nutritional Supplement to Exercised Horses Rick M. Arthur, DVM†; Heather K. Knych, DVM, PhD, Diplomate ACVCP*; and Scott D. Stanley, PhD After oral administration of a nutritional supplement containing dehydroepiandrosterone (DHEA), horses are capable of producing detectable levels of testosterone, which can result in a positive regulatory finding. Authors’ addresses: School of Veterinary Medicine (Arthur), K.L. Maddy Equine Analytical Chemistry Laboratory (Knych, Stanley), University of California, Davis, CA 95616; e-mail: [email protected]. *Corresponding author; †presenting author. © 2013 AAEP. 1. Introduction various times up to 48 hours after drug administra- Dehydroepiandrosterone (DHEA) is a weak andro- tion. Plasma concentrations of DHEA, testoster- gen as well as a precursor to the much more potent one, and pregnenolone as well as their sulfated androgen, testosterone. Although DHEA is not conjugates were measured by means of liquid chro- specifically banned from administration to race- matography-mass spectrometry. horses, the potential for metabolism to substances such as testosterone that are not permitted in racing 3. Results and Discussion make its presence in nutritional supplements fed to Peak plasma concentrations of DHEA, DHEA sul- horses a regulatory concern. In the current study, fate, and testosterone sulfate were 10.1 Ϯ 8.84 ng/ we sought to describe the metabolic profile after Ϯ Ϯ administration of a nutritional supplement contain- ml, 25.7 10.2, and 0.670 1.17, respectively. ing precursors to non-permitted androgens to exer- All compounds were below the limit of detection by cised female horses.