Spironolactone
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Dehydroepiandrosterone – Is the Fountain of Youth Drying Out?
Physiol. Res. 52: 397-407, 2003 MINIREVIEW Dehydroepiandrosterone – Is the Fountain of Youth Drying Out? P. CELEC 1,2, L. STÁRKA3 1Faculty of Medicine, 2Faculty of Natural Sciences, Comenius University, Bratislava, Slovakia and 3Institute of Endocrinology, Prague, Czech Republic Received September 15, 2002 Accepted October 7, 2002 Summary Dehydroepiandrosterone (DHEA) and its sulphate-bound form (DHEAS) are important steroids mainly of adrenal origin. Their physiological and pathophysiological functions are not yet fully identified, although a number of various possible features have been hypothesized. Most popular is the description of the “hormone of youth” as the long-term dynamics of DHEA levels are characterized by a sharp age-related decline in the late adulthood and later. Low levels of DHEA are, however, associated not only with the ageing process but also with diabetes mellitus, cardiovascular diseases and some neurological or immunological entities. In the past decade, a number of brief studies have concentrated on these relationships and also on the role of exogenous DHEA in health, disease and human well-being. This article tries to summarize some of the most important facts achieved recently. Key words Dehydroepiandrosterone • Intracrinology • Hormone replacement therapy • Steroids Introduction functions: 1) DHEA is an endogenous metabolite that cannot be patented so that pharmaceutical companies are In 1934 Butenandt and Dannenbaum isolated not interested in supporting research in this field. dehydroepiandrosterone (DHEA) from urine and in 1944 2) DHEA can be described as a “human molecule” Munson and colleagues identified its 3β-sulphate because other investigated species have much lower (DHEAS). Even now, nearly 70 years later, we still do concentrations. -
Compositions Comprising Drospirenone Molecularly
(19) & (11) EP 1 748 756 B1 (12) EUROPEAN PATENT SPECIFICATION (45) Date of publication and mention (51) Int Cl.: of the grant of the patent: A61K 9/00 (2006.01) A61K 9/107 (2006.01) 29.04.2009 Bulletin 2009/18 A61K 9/48 (2006.01) A61K 9/16 (2006.01) A61K 9/20 (2006.01) A61K 9/14 (2006.01) (2006.01) (2006.01) (21) Application number: 05708751.2 A61K 9/70 A61K 31/565 (22) Date of filing: 10.03.2005 (86) International application number: PCT/IB2005/000665 (87) International publication number: WO 2005/087194 (22.09.2005 Gazette 2005/38) (54) COMPOSITIONS COMPRISING DROSPIRENONE MOLECULARLY DISPERSED ZUSAMMENSETZUNGEN AUS DROSPIRENON IN MOLEKULARER DISPERSION DES COMPOSITIONS CONTENANT DROSPIRENONE A DISPERSION MOLECULAIRE (84) Designated Contracting States: (72) Inventors: AT BE BG CH CY CZ DE DK EE ES FI FR GB GR • FUNKE, Adrian HU IE IS IT LI LT LU MC NL PL PT RO SE SI SK TR D-14055 Berlin (DE) Designated Extension States: • WAGNER, Torsten AL BA HR MK YU 13127 Berlin (DE) (30) Priority: 10.03.2004 EP 04075713 (74) Representative: Wagner, Kim 10.03.2004 US 551355 P Plougmann & Vingtoft a/s Sundkrogsgade 9 (43) Date of publication of application: P.O. Box 831 07.02.2007 Bulletin 2007/06 2100 Copenhagen Ø (DK) (60) Divisional application: (56) References cited: 08011577.7 / 1 980 242 EP-A- 1 260 225 EP-A- 1 380 301 WO-A-01/52857 WO-A-20/04022065 (73) Proprietor: Bayer Schering Pharma WO-A-20/04041289 US-A- 5 569 652 Aktiengesellschaft US-A- 5 656 622 US-A- 5 789 442 13353 Berlin (DE) Note: Within nine months of the publication of the mention of the grant of the European patent in the European Patent Bulletin, any person may give notice to the European Patent Office of opposition to that patent, in accordance with the Implementing Regulations. -
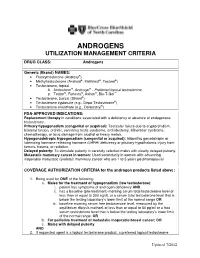
Androgens Utilization Management Criteria
ANDROGENS UTILIZATION MANAGEMENT CRITERIA DRUG CLASS: Androgens Generic (Brand) NAMES: • Fluoxymesterone (Androxy®) • Methyltestosterone (Android®, Methitest®, Testred®) • Testosterone, topical A. Androderm®, Androgel® - Preferred topical testosterone ® ® ® ™ B. Testim , Fortesta , Axiron , Bio-T-Gel • Testosterone, buccal (Striant®) • Testosterone cypionate (e.g., Depo-Testosterone®) • Testosterone enanthate (e.g., Delatestryl®) FDA-APPROVED INDICATIONS: Replacement therapy in conditions associated with a deficiency or absence of endogenous testosterone. Primary hypogonadism (congenital or acquired): Testicular failure due to cryptorchidism, bilateral torsion, orchitis, vanishing testis syndrome, orchidectomy, Klinefelter syndrome, chemotherapy, or toxic damage from alcohol or heavy metals. Hypogonadotropic hypogonadism (congenital or acquired): Idiopathic gonadotropin or luteinizing hormone-releasing hormone (LHRH) deficiency or pituitary-hypothalamic injury from tumors, trauma, or radiation. Delayed puberty: To stimulate puberty in carefully selected males with clearly delayed puberty. Metastatic mammary cancer in women: Used secondarily in women with advancing inoperable metastatic (skeletal) mammary cancer who are 1 to 5 years postmenopausal COVERAGE AUTHORIZATION CRITERIA for the androgen products listed above: 1. Being used for ONE of the following: a. Males for the treatment of hypogonadism (low testosterone): i. patient has symptoms of androgen deficiency AND ii. has a baseline (pre-treatment) morning serum total testosterone level of less than or equal to 300 ng/dL or a serum total testosterone level that is below the testing laboratory’s lower limit of the normal range OR iii. baseline morning serum free testosterone level, measured by the equilibrium dialysis method, of less than or equal to 50 pg/ml or a free serum testosterone level that is below the testing laboratory’s lower limit of the normal range, OR b. -

The Effects of Androgens and Antiandrogens on Hormone Responsive Human Breast Cancer in Long-Term Tissue Culture1
[CANCER RESEARCH 36, 4610-4618, December 1976] The Effects of Androgens and Antiandrogens on Hormone responsive Human Breast Cancer in Long-Term Tissue Culture1 Marc Lippman, Gail Bolan, and Karen Huff MedicineBranch,NationalCancerInstitute,Bethesda,Maryland20014 SUMMARY Information characterizing the interaction between an drogens and breast cancer would be desirable for several We have examined five human breast cancer call lines in reasons. First, androgens can affect the growth of breast conhinuous tissue culture for andmogan responsiveness. cancer in animals. Pharmacological administration of an One of these cell lines shows a 2- ho 4-fold stimulation of drogens to rats bearing dimathylbenzanthracene-induced thymidina incorporation into DNA, apparent as early as 10 mammary carcinomas is associated wihh objective humor hr following androgen addition to cells incubated in serum regression (h9, 22). Shionogi h15 cells, from a mouse mam free medium. This stimulation is accompanied by an ac many cancer in conhinuous hissue culture, have bean shown celemation in cell replication. Antiandrogens [cyproterona to be shimulatedby physiological concentrations of andro acetate (6-chloro-17a-acelata-1,2a-methylena-4,6-pregna gen (21), thus suggesting that some breast cancer might be diene-3,20-dione) and R2956 (17f3-hydroxy-2,2,1 7a-tnima androgen responsive in addition to being estrogen respon thoxyastra-4,9,1 1-Inane-i -one)] inhibit both protein and siva. DNA synthesis below control levels and block androgen Evidence also indicates that tumor growth in humans may mediahed stimulation. Prolonged incubahion (greahenhhan be significantly altered by androgens. About 20% of pahianhs 72 hn) in antiandrogen is lethal. -

Specifications of Approved Drug Compound Library
Annexure-I : Specifications of Approved drug compound library The compounds should be structurally diverse, medicinally active, and cell permeable Compounds should have rich documentation with structure, Target, Activity and IC50 should be known Compounds which are supplied should have been validated by NMR and HPLC to ensure high purity Each compound should be supplied as 10mM solution in DMSO and at least 100µl of each compound should be supplied. Compounds should be supplied in screw capped vial arranged as 96 well plate format. -

CASODEX (Bicalutamide)
HIGHLIGHTS OF PRESCRIBING INFORMATION • Gynecomastia and breast pain have been reported during treatment with These highlights do not include all the information needed to use CASODEX 150 mg when used as a single agent. (5.3) CASODEX® safely and effectively. See full prescribing information for • CASODEX is used in combination with an LHRH agonist. LHRH CASODEX. agonists have been shown to cause a reduction in glucose tolerance in CASODEX® (bicalutamide) tablet, for oral use males. Consideration should be given to monitoring blood glucose in Initial U.S. Approval: 1995 patients receiving CASODEX in combination with LHRH agonists. (5.4) -------------------------- RECENT MAJOR CHANGES -------------------------- • Monitoring Prostate Specific Antigen (PSA) is recommended. Evaluate Warnings and Precautions (5.2) 10/2017 for clinical progression if PSA increases. (5.5) --------------------------- INDICATIONS AND USAGE -------------------------- ------------------------------ ADVERSE REACTIONS ----------------------------- • CASODEX 50 mg is an androgen receptor inhibitor indicated for use in Adverse reactions that occurred in more than 10% of patients receiving combination therapy with a luteinizing hormone-releasing hormone CASODEX plus an LHRH-A were: hot flashes, pain (including general, back, (LHRH) analog for the treatment of Stage D2 metastatic carcinoma of pelvic and abdominal), asthenia, constipation, infection, nausea, peripheral the prostate. (1) edema, dyspnea, diarrhea, hematuria, nocturia, and anemia. (6.1) • CASODEX 150 mg daily is not approved for use alone or with other treatments. (1) To report SUSPECTED ADVERSE REACTIONS, contact AstraZeneca Pharmaceuticals LP at 1-800-236-9933 or FDA at 1-800-FDA-1088 or ---------------------- DOSAGE AND ADMINISTRATION ---------------------- www.fda.gov/medwatch The recommended dose for CASODEX therapy in combination with an LHRH analog is one 50 mg tablet once daily (morning or evening). -

Combination Therapy of Antiandrogen and XIAP Inhibitor for Treating Advanced Prostate Cancer
Combination Therapy of Antiandrogen and XIAP Inhibitor for Treating Advanced Prostate Cancer Michael Danquah, Charles B. Duke, Renukadevi Patil, Duane D. Miller & Ram I. Mahato Pharmaceutical Research An Official Journal of the American Association of Pharmaceutical Scientists ISSN 0724-8741 Volume 29 Number 8 Pharm Res (2012) 29:2079-2091 DOI 10.1007/s11095-012-0737-1 1 23 Your article is protected by copyright and all rights are held exclusively by Springer Science+Business Media, LLC. This e-offprint is for personal use only and shall not be self- archived in electronic repositories. If you wish to self-archive your work, please use the accepted author’s version for posting to your own website or your institution’s repository. You may further deposit the accepted author’s version on a funder’s repository at a funder’s request, provided it is not made publicly available until 12 months after publication. 1 23 Author's personal copy Pharm Res (2012) 29:2079–2091 DOI 10.1007/s11095-012-0737-1 RESEARCH PAPER Combination Therapy of Antiandrogen and XIAP Inhibitor for Treating Advanced Prostate Cancer Michael Danquah & Charles B. Duke III & Renukadevi Patil & Duane D. Miller & Ram I. Mahato Received: 4 February 2012 /Accepted: 9 March 2012 /Published online: 27 March 2012 # Springer Science+Business Media, LLC 2012 ABSTRACT Results CBDIV17 was more potent than bicalutamide and Purpose Overexpression of the androgen receptor (AR) and inhibited proliferation of C4-2 and LNCaP cells, IC50 for CBDIV17 anti-apoptotic genes including X-linked inhibitor of apoptosis was ∼12 μMand∼21 μM in LNCaP and C4-2 cells, respectively, protein (XIAP) provide tumors with a proliferative advantage. -

COVID-19—The Potential Beneficial Therapeutic Effects of Spironolactone During SARS-Cov-2 Infection
pharmaceuticals Review COVID-19—The Potential Beneficial Therapeutic Effects of Spironolactone during SARS-CoV-2 Infection Katarzyna Kotfis 1,* , Kacper Lechowicz 1 , Sylwester Drozd˙ zal˙ 2 , Paulina Nied´zwiedzka-Rystwej 3 , Tomasz K. Wojdacz 4, Ewelina Grywalska 5 , Jowita Biernawska 6, Magda Wi´sniewska 7 and Miłosz Parczewski 8 1 Department of Anesthesiology, Intensive Therapy and Acute Intoxications, Pomeranian Medical University in Szczecin, 70-111 Szczecin, Poland; [email protected] 2 Department of Pharmacokinetics and Monitored Therapy, Pomeranian Medical University, 70-111 Szczecin, Poland; [email protected] 3 Institute of Biology, University of Szczecin, 71-412 Szczecin, Poland; [email protected] 4 Independent Clinical Epigenetics Laboratory, Pomeranian Medical University, 71-252 Szczecin, Poland; [email protected] 5 Department of Clinical Immunology and Immunotherapy, Medical University of Lublin, 20-093 Lublin, Poland; [email protected] 6 Department of Anesthesiology and Intensive Therapy, Pomeranian Medical University in Szczecin, 71-252 Szczecin, Poland; [email protected] 7 Clinical Department of Nephrology, Transplantology and Internal Medicine, Pomeranian Medical University, 70-111 Szczecin, Poland; [email protected] 8 Department of Infectious, Tropical Diseases and Immune Deficiency, Pomeranian Medical University in Szczecin, 71-455 Szczecin, Poland; [email protected] * Correspondence: katarzyna.kotfi[email protected]; Tel.: +48-91-466-11-44 Abstract: In March 2020, coronavirus disease 2019 (COVID-19) caused by SARS-CoV-2 was declared Citation: Kotfis, K.; Lechowicz, K.; a global pandemic by the World Health Organization (WHO). The clinical course of the disease is Drozd˙ zal,˙ S.; Nied´zwiedzka-Rystwej, unpredictable but may lead to severe acute respiratory infection (SARI) and pneumonia leading to P.; Wojdacz, T.K.; Grywalska, E.; acute respiratory distress syndrome (ARDS). -

20Mg Spironolactone I.P…..50Mg
For the use only of a Registered Medical Practitioner or Hospital or a Laboratory. This package insert is continually updated: Please read carefully before using a new pack Frusemide and Spironolactone Tablets Lasilactone® 50 COMPOSITION Each film coated tablet contains Frusemide I.P. …….. 20mg Spironolactone I.P…..50mg THERAPEUTIC INDICATIONS Lasilactone® contains a short-acting diuretic and a long-acting aldosterone antagonist. It is indicated in the treatment of resistant oedema where this is associated with secondary hyperaldosteronism; conditions include chronic congestive cardiac failure and hepatic cirrhosis. Treatment with Lasilactone® should be reserved for cases refractory to a diuretic alone at conventional doses. This fixed ratio combination should only be used if titration with the component drugs separately indicates that this product is appropriate. The use of Lasilactone® in the management of essential hypertension should be restricted to patients with demonstrated hyperaldosteronism. It is recommended that in these patients also, this combination should only be used if titration with the component drugs separately indicates that this product is appropriate. POSOLOGY AND METHOD OF ADMINISTRATION For oral administration. The dose must be the lowest that is sufficient to achieve the desired effect. Adults: 1-4 tablets daily. Children: The product is not suitable for use in children. Elderly: Frusemide and Spironolactone may both be excreted more slowly in the elderly. Tablets are best taken at breakfast and/or lunch with a generous amount of liquid (approx. 1 glass). An evening dose is not recommended, especially during initial treatment, because of the increased nocturnal output of urine to be expected in such cases. -

Effect of Dehydroepiandrosterone and Testosterone Supplementation on Systemic Lipolysis
ORIGINAL ARTICLE Effect of Dehydroepiandrosterone and Testosterone Supplementation on Systemic Lipolysis Ana E. Espinosa De Ycaza, Robert A. Rizza, K. Sreekumaran Nair, and Michael D. Jensen Division of Endocrinology, Endocrine Research Unit, Mayo Clinic, Rochester, Minnesota 55905 Downloaded from https://academic.oup.com/jcem/article/101/4/1719/2804555 by guest on 24 September 2021 Context: Dehydroepiandrosterone (DHEA) and T hormones are advertised as antiaging, antiobe- sity products. However, the evidence that these hormones have beneficial effects on adipose tissue metabolism is limited. Objective: The objective of the study was to determine the effect of DHEA and T supplementation on systemic lipolysis during a mixed-meal tolerance test (MMTT) and an iv glucose tolerance test (IVGTT). Design: This was a 2-year randomized, double-blind, placebo-controlled trial. Setting: The study was conducted at a general clinical research center. Participants: Sixty elderly women with low DHEA concentrations and 92 elderly men with low DHEA and bioavailable T concentrations participated in the study. Interventions: Elderly women received 50 mg DHEA (n ϭ 30) or placebo (n ϭ 30). Elderly men received 75 mg DHEA (n ϭ 30),5mgT(nϭ 30), or placebo (n ϭ 32). Main Outcome Measures: In vivo measures of systemic lipolysis (palmitate rate of appearance) during a MMTT or IVGTT. Results: At baseline there was no difference in insulin suppression of lipolysis measured during MMTT and IVGTT between the treatment groups and placebo. For both sexes, a univariate analysis showed no difference in changes in systemic lipolysis during the MMTT or IVGTT in the DHEA group and T group when compared with placebo. -

An Unexpected Target for Androgen Deprivation Therapy with Prognosis and Diagnostic Implications
Author Manuscript Published OnlineFirst on October 11, 2013; DOI: 10.1158/0008-5472.CAN-13-1462 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. 1 Androgen glucuronidation: an unexpected target for androgen deprivation therapy with prognosis and diagnostic implications. Laurent Grosse1, Sophie Pâquet1, Patrick Caron1, Ladan Fazli2, Paul S. Rennie2, Alain Bélanger3 and Olivier Barbier1 1Laboratory of Molecular Pharmacology, CHU-Québec Research Centre and Faculty of Pharmacy, Laval University, Québec, Canada 2 Vancouver Prostate Centre at VGH, University of British Columbia, Vancouver, British Columbia, Canada. 3CHU-Québec Research Centre and Faculty of Medicine, Laval University, Québec, Canada Running title: Ablation therapy improves androgen glucuronidation in PCa Keywords: Prostate cancer, androgen ablation therapy, glucuronidation, biomarker, drug target. Financial support: This study was supported by grants from the Canadian Institutes of Health Research (CIHR), the Terry Fox foundation and the Canadian Foundation for Innovation. S. Pâquet is holder of scholarships from CIHR and the Fonds pour la Recherche en Santé du Québec (FRSQ). L. Grosse is supported by a scholarship from the Fonds pour l’Enseignement et la Recherche (FER) from the Faculty of Pharmacy, Laval University (Québec). O. Barbier is holder of salary grants from the CIHR (New Investigator Award #MSH95330) and FRSQ (Junior 2 Scholarship). Address correspondence to: Olivier Barbier, Ph.D. Laboratory of Molecular Pharmacology CHU-Québec Research Centre 2705, boulevard Laurier Québec (QC) G1V 4G2, Canada Phone: 418 654 2296 Fax: 418 654 2769 Email: [email protected] Conflict of interests: Authors have nothing to disclose. Downloaded from cancerres.aacrjournals.org on September 26, 2021. -

Reproductive DHEA-S
Reproductive DHEA-S Analyte Information - 1 - DHEA-S Introduction DHEA-S, DHEA sulfate or dehydroepiandrosterone sulfate, it is a metabolite of dehydroepiandrosterone (DHEA) resulting from the addition of a sulfate group. It is the sulfate form of aromatic C19 steroid with 10,13-dimethyl, 3-hydroxy group and 17-ketone. Its chemical name is 3β-hydroxy-5-androsten-17-one sulfate, its summary formula is C19H28O5S and its molecular weight (Mr) is 368.5 Da. The structural formula of DHEA-S is shown in (Fig.1). Fig.1: Structural formula of DHEA-S Other names used for DHEA-S include: Dehydroisoandrosterone sulfate, (3beta)-3- (sulfooxy), androst-5-en-17-one, 3beta-hydroxy-androst-5-en-17-one hydrogen sulfate, Prasterone sulfate and so on. As DHEA-S is very closely connected with DHEA, both hormones are mentioned together in the following text. Biosynthesis DHEA-S is the major C19 steroid and is a precursor in testosterone and estrogen biosynthesis. DHEA-S originates almost exclusively in the zona reticularis of the adrenal cortex (Fig.2). Some may be produced by the testes, none is produced by the ovaries. The adrenal gland is the sole source of this steroid in women, whereas in men the testes secrete 5% of DHEA-S and 10 – 20% of DHEA. The production of DHEA-S and DHEA is regulated by adrenocorticotropin (ACTH). Corticotropin-releasing hormone (CRH) and, to a lesser extent, arginine vasopressin (AVP) stimulate the release of adrenocorticotropin (ACTH) from the anterior pituitary gland (Fig.3). In turn, ACTH stimulates the adrenal cortex to secrete DHEA and DHEA-S, in addition to cortisol.