ICMR 2017-National Ethical Guidelines for Biomedical And
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

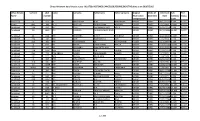
The India Cements Limited
THE INDIA CEMENTS LIMITED UNCLAIMED DIVIDEND FOR THE YEAR 2010-11 TO BE TRANSFERRED TO INVESTOR EDUCATION AND PROTECTION FUND AS REQUIRED UNDER SECTION 124 OF THE COMPANIES ACT 2013 READ WITH THE INVESTOR EDUCATION AND PROTECTION FUND AUTHORITY (ACCOUNTING, AUDIT, TRANSFER AND REFUND) RULES, 2016, AS AMENDED FOLIO / DPID_CLID NAME CITY PINCODE 1201040000010433 KUMAR KRISHNA LADE BHILAI 490006 1201060000057278 Bhausaheb Trimbak Pagar Nasik 422005 1201060000138625 Rakesh Dutt Panvel 410206 1201060000175241 JAI KISHAN MOHATA RAIPUR 492001 1201060000288167 G. VINOD KUMAR JAIN MANDYA 571401 1201060000297034 MALLAPPA LAGAMANNA METRI BELGAUM 591317 1201060000309971 VIDYACHAND RAMNARAYAN GILDA LATUR 413512 1201060000326174 LEELA K S UDUPI 576103 1201060000368107 RANA RIZVI MUZAFFARPUR 842001 1201060000372052 S KAILASH JAIN BELLARY 583102 1201060000405315 LAKHAN HIRALAL AGRAWAL JALNA 431203 1201060000437643 SHAKTI SHARAN SHUKLA BHADOHI 221401 1201060000449205 HARENDRASINH LALUBHA RANA LATHI 365430 1201060000460605 PARASHURAMAPPA A SHIMOGA 577201 1201060000466932 SHASHI KAPOOR BHAGALPUR 812001 1201060000472832 SHARAD GANESH KENI RATNAGIRI 415612 1201060000507881 NAYNA KESHAVLAL DAVE NALLASOPARA (E) 401209 1201060000549512 SANDEEP OMPRAKASH NEVATIA MAHAD 402301 1201060000555617 SYED QUAMBER HUSSAIN MUZAFFARPUR 842001 Page 1 of 301 FOLIO / DPID_CLID NAME CITY PINCODE 1201060000567221 PRASHANT RAMRAO KONDEBETTU BELGAUM 591201 1201060000599735 VANDANA MISHRA ALLAHABAD 211016 1201060000630654 SANGITA AGARWAL CUTTACK 753004 1201060000646546 SUBODH T -

Nominations for Padma Awards 2011
c Nominations fof'P AWARDs 2011 ADMA ~ . - - , ' ",::i Sl. Name';' Field State No ShriIshwarappa,GurapJla Angadi Art Karnataka " Art-'Cinema-Costume Smt. Bhanu Rajopadhye Atharya Maharashtra 2. Designing " Art - Hindustani 3. Dr; (Smt.).Prabha Atre Maharashtra , " Classical Vocal Music 4. Shri Bhikari.Charan Bal Art - Vocal Music 0, nssa·' 5. Shri SamikBandyopadhyay Art - Theatre West Bengal " 6: Ms. Uttara Baokar ',' Art - Theatre , Maharashtra , 7. Smt. UshaBarle Art Chhattisgarh 8. Smt. Dipali Barthakur Art " Assam Shri Jahnu Barua Art - Cinema Assam 9. , ' , 10. Shri Neel PawanBaruah Art Assam Art- Cinema Ii. Ms. Mubarak Begum Rajasthan i", Playback Singing , , , 12. ShriBenoy Krishen Behl Art- Photography Delhi " ,'C 13. Ms. Ritu Beri , Art FashionDesigner Delhi 14. Shri.Madhur Bhandarkar Art - Cinema Maharashtra Art - Classical Dancer IS. Smt. Mangala Bhatt Andhra Pradesh Kathak Art - Classical Dancer 16. ShriRaghav Raj Bhatt Andhra Pradesh Kathak : Art - Indian Folk I 17., Smt. Basanti Bisht Uttarakhand Music Art - Painting and 18. Shri Sobha Brahma Assam Sculpture , Art - Instrumental 19. ShriV.S..K. Chakrapani Delhi, , Music- Violin , PanditDevabrata Chaudhuri alias Debu ' Art - Instrumental 20. , Delhi Chaudhri ,Music - Sitar 21. Ms. Priyanka Chopra Art _Cinema' Maharashtra 22. Ms. Neelam Mansingh Chowdhry Art_ Theatre Chandigarh , ' ,I 23. Shri Jogen Chowdhury Art- Painting \VesfBengal 24.' Smt. Prafulla Dahanukar Art ~ Painting Maharashtra ' . 25. Ms. Yashodhara Dalmia Art - Art History Delhi Art - ChhauDance 26. Shri Makar Dhwaj Darogha Jharkhand Seraikella style 27. Shri Jatin Das Art - Painting Delhi, 28. Shri ManoharDas " Art Chhattisgarh ' 29. , ShriRamesh Deo Art -'Cinema ,Maharashtra Art 'C Hindustani 30. Dr. Ashwini Raja Bhide Deshpande Maharashtra " classical vocalist " , 31. ShriDeva Art - Music Tamil Nadu Art- Manipuri Dance 32. -

14 (2Nd INTERIM DIVIDEND) Details of Unclaimed Dividend Amount As on 31St March, 2019 Dividend Proposed Date of Sr
WOCKHARDT LIMITED - EQUITY DIVIDEND FOR YEAR 2013 - 14 (2nd INTERIM DIVIDEND) Details of Unclaimed Dividend amount as on 31st March, 2019 Dividend Proposed Date of Sr. Folio Number or Amount Name of the Shareholder Address State PINCode Transfer to IEPF No. DP/Client ID Unclaimed in (DD-MON-YYYY) (Rs.) 1 Satguru Capital Andfinancespvtltd 37-40, Subhash Road, 4Th Floor, Sunteck Maharashtra 400057 1100001100017351 1500.00 16-Mar-2021 Centre, Vile Parle (East) Mumbai 2 Gayatri Sampatlal Holani F No 104 Nit Building Surya Nagar Bagadganj Maharashtra 440008 1201060000013183 155.00 16-Mar-2021 Nagpur 3 Hasan Imam 115,Rahmat Colony , Po- Doranda Ranchi- Jharkhand 834002 1201060000159130 50.00 16-Mar-2021 834002 Ranchi 4 Jeni Isak Rangwala Near Kalika Mandir Old Agra Road Nasik Nasik Maharashtra 422002 1201060000346767 500.00 16-Mar-2021 5 Sunil Bhatnagar 124/43 Baghambari Allapur Allahabad Uttar Pradesh 1201060000457541 250.00 16-Mar-2021 6 Basant Kumar Singh 28/3 C.Y. Chintamani Road Darbhanga Colony Uttar Pradesh 1201060000461778 490.00 16-Mar-2021 Allahabad 7 Pareshbhai Vithalbhai Patel A/10 Parswa Nagar Near Ravi Park Vasna Road Gujarat 390015 1201060000479589 175.00 16-Mar-2021 Vadodara 8 Anilkumar Salagram Somani Near Matsyodari Vidyalaya Omshanti Colony, Maharashtra 431204 1201060000490731 50.00 16-Mar-2021 Nutan Vashat,Ambad Ambad 9 Kumar Anil P-16/243 Attarsuiya Allahabad Uttar Pradesh 1201060000502807 50.00 16-Mar-2021 10 Anita Sondhi 103-Sarwal Mandir Morh Jammu Jammu and Kashmir 180001 1201060000584769 650.00 16-Mar-2021 11 Varsha -

21. 08. 2020 * 1 Cause List
21. 08. 2020 * 1 CAUSE LIST HIGH COURT OF DELHI: NEW DELHI No.119/RG/DHC/2020 Dated: 22.04.2020 OFFICE ORDER As per the directions of Hon’ble the Chief Justice, on the recommendations of the Hon’ble Information Technology Committee, and in view of the directions passed by the Hon’ble Supreme Court in the case of Suo Motu Writ (Civil) No.5/2020 dated 6th April 2020 titled “Re: Guidelines for Court Functioning Through Video Conferencing During Covid-19 Pandemic”, this Court has started a Helpline Number “14611” to receive any complaint with regard to deficiency in visual acuity or audibility experienced by participants during the video conferencing proceedings. The helpline number will be manned by the officer nominated by the Registrar (IT) for receiving of any complaint, who, in turn, will communicate the same to the Court Master(s) of the concerned Bench. To facilitate lodgement of complaints the Listing Branch shall provide in the cause list, in addition to the helpline number, the mobile number of the court master of the concerned Bench. Furthermore, the cause list will indicate that no grievance will be entertained with regard to connectivity, quality or otherwise, after the video conferencing proceedings are over, save and except, where directions are passed by the concerned Bench to entertain such complaints post conclusion of video conferencing proceedings. By Order Sd/- (Manoj Jain) Registrar General HIGH COURT OF DELHI, NEW DELHI No. R-340/RG/DHC/2020 Dated : 25.05.2020 CIRCULAR SUBJECT: Contacting Court Masters for the limited purpose only. On account of outbreak of COVID-19, regular functioning of this court remains suspended and hearing of urgent matters is presently restricted only to videoconferencing. -

The Association of Physicians of India
The Association of Physicians of India http://www.apiindia.org/contents_txtbk_11.html Home About API JAPI ICP PRF API Textbook of Medicine 74th AGM API House Chapters & Branches Contact REGISTER | LOGIN | FORGOT PASSWORD Awards Orations Lectureships ICP Fellowship Publications Announcements Elections e-Hypertension e-Learning e-Stroke Abstract API Textbook of Medicine - 11th Edition - Contents VOLUME 1 Introduction 1. Introduction Sandhya A Kamath Section 1 : Epidemiology 1. Principles of Epidemiology of Communicable Diseases Jugal Kishore, Tanu Anand 2. Principles of Epidemiology of Non-Communicable Diseases Jugal Kishore, Tanu Anand Section 2 : Clinical Approach 1. Approach to a Febrile Patient DB Kadam 2. Pain - A General Approach Mangesh Tiwaskar 3. Chest Pain Ajaykumar U Mahajan 4. Dyspnoea Udai Lal 5. Cough and Hemoptysis Haridas B Prasad 6. Palpitations Milind Phadke 7. Abdominal Pain Pravin Rathi 8. Lymphadenopathy Vrinda Kulkarni 9. Oedema and Anasarca Sekhar Chakraborty 10. Ascites Neelam Narendra Redkar 11. Jaundice Aniruddha Y Phadke 12. Constipation and Diarrhoea Prabha Sawant 13. Weight Loss and Cachexia A Muruganathan, Gowri Sankar Murugan 14. Altered Sensorium Mrinal Kanti Roy, Sujoy Sarkar 15. Syncope Amar R Pazare 16. Dizziness and Vertigo Sanjiv Maheshwari 17. Approach to Ataxia CS Narayanan 18. Motor Weakness Uma Sundar 19. Sensory Loss Rajinder K Bansal 20. Fever with Rash Yojana Gokhale Section 3 : Infectious Dieseases Part A: General Considerations 1. Basic Considerations of Infections MVS Subbalaxmi 2. Laboratory Diagnosis of Infections Camilla Rodrigues, Anand Shah 3. Syndromic Approach to Infectious Diseases Mahendra Dadke 4. Antimicrobial Therapy: PKPD of Antimicrobials Rajeev Soman 5. Inhibitors of Cell Wall Synthesis Vasudeva Acharya 6. -

State Wise Fellow Address
Delhi 1. Dr. Balram Airan 2. Dr. Kuljeet Singh Anand Professor & Head of Cardio-Thoracic A-118, Swasthya Vihar, & Vascular Surgery & Delhi-110092 Chief of Cardiothoracic Sciences Centre, All India Institute of Medical Sciences, Ansari Nagar, New Delhi-110029. 3. Dr. D.S.Agarwal 4. Dr.Neera Agarwal B-24, Swasthya Vihar LUV-403, Agresen Apartments Delhi-110092. 66-I.P.Extension, Delhi-110092 5. Dr. Sanjay Kumar Agarwal 6. Dr. Sudarshan K.Aggarwal Prof. & Head 10-B, Kasturba Gandhi Marg, Deptt. of Nephrology New Delhi-110001 AIIMS, Ansari Nagar New Delhi-110029 7. Dr.Rajeev Bhushan Ahuja 8. Vice Admiral Retd. (Dr.) Anil Chandra B-18, Swasthya Vihar, Anand Vikas Marg, Senior Consultant Gastroenterology Delhi-110092 & Hepatology C-222, Sarvodaya Enclave Second Floor New Delhi-110017 9. Dr. Ashima Anand 10. Dr. S.K.Angra Principal Investigator A-58, Swasthya Vihar, Exertional Breathlessness Studies Delhi-110092. Laboratory (SERB), V.P. Chest Institute, Delhi University, Delhi-110007 11. Dr. Narendra Kumar Arora 12. Dr.Rajvardhan Azad Executive Director M 18, Saket, The INCEN Trust International, Marg 50, 2nd Floor, F-1/5, New Delhi-100017 Okhla Industrial Area, Phase-I, New Delhi-110020 13. Dr. Arvind Bagga 14. Dr.Sudhir Bahadur, FAMS Professor, A-73, Madhuvan Colony, Division of Nephrology, Vikas Marg, Department of Paediatrics, Delhi – 110092 All India Institute of Medical Sciences, Ansari Nagar, New Delhi-110029 15. Dr. Minu Bajpai 16. Dr. Prema Bali Professor A-5, Greater Kailash, Department of Paediatric Surgery Part II, All India Institute of Medical Sciences, New Delhi-110048 Ansari Nagar, New Delhi-110029 17. -
17.07.2020 J- 1 Pronouncement of Judgement (Applt
17.07.2020 J- 1 PRONOUNCEMENT OF JUDGEMENT (APPLT. JURISDICTION) HON'BLE MR. JUSTICE RAJIV SAHAI ENDLAW HON'BLE MS. JUSTICE ASHA MENON AT THE END OF BOARD 1. W.P.(C) 3792/2020 UDAI SHANKAR SRIVASTAVA ANKUR CHHIBER, ARUN BHARDWAJ VS. UNION OF INDIA ([email protected]) & ORS. ABHISHEK SHARMA, NIKHIL BHARDWAJ PIYUSH GAUR, NARESH KAUSHIK ([email protected]) VARDHMAN KAUSHIK HON’BLE MR. JUSTICE MANOJ KUMAR OHRI AT 10:30 A.M. 1. CRL.A. 333/2020 ROHIT VINAY KUMAR SHARMA VS. STATE M.P.SINGH HIGH COURT OF DELHI REGISTRAR(LISTING) 16.07.2020 17. 07. 2020 * 1 CAUSE LIST ** HIGH COURT OF DELHI: NEW DELHI No.119/RG/DHC/2020 Dated: 22.04.2020 OFFICE ORDER As per the directions of Hon’ble the Chief Justice, on the recommendations of the Hon’ble Information Technology Committee, and in view of the directions passed by the Hon’ble Supreme Court in the case of Suo Motu Writ (Civil) No.5/2020 dated 6th April 2020 titled “Re: Guidelines for Court Functioning Through Video Conferencing During Covid-19 Pandemic”, this Court has started a Helpline Number “14611” to receive any complaint with regard to deficiency in visual acuity or audibility experienced by participants during the video conferencing proceedings. The helpline number will be manned by the officer nominated by the Registrar (IT) for receiving of any complaint, who, in turn, will communicate the same to the Court Master(s) of the concerned Bench. To facilitate lodgement of complaints the Listing Branch shall provide in the cause list, in addition to the helpline number, the mobile number of the court master of the concerned Bench. -

CSI 2020 Scientific Committee!
Scientific Committee Chairman’s Message Dear Friends, Greetings from CSI 2020 Scientific Committee! It’s inconceivable how things have changed and what we have lost this year. But challenging times also have a way of uncovering silver linings. We present you a week long conference CSI 2020 at Ahmedabad in a hybrid platform. Virtual conferences might lack the intimacy of a physical gathering, but it’s still possible for attendees to connect with each other. Please acknowledge that these are weird times and the experience you get from a virtual conference may be a little different. Yet this format provides opportunities as well and we have attempted to provide you the scientific content in an appealing manner which will certainly satisfy your intellectual curiosity. It is my proud privilege to be the Chair Scientific committee CSI 2020 Ahmedabad. We were able to assemble a group of vibrant cardiologists from all across India who worked tirelessly during the past months to formulate the scientific program. I am thankful for their exceptional support and contributions in planning the scientific program and have no hesitation to give all credits they richly deserve. Designing the scientific programme for the largest congregation of cardiologists in India is certainly not an easy task. Such a program should reflect the current direction of advances happening in the practice of cardiology. It should also update the knowledge base of the attending delegates. We felt that a CSI conference in addition should facilitate research initiatives addressing unique issues faced by cardiologists in India. Research methodology workshop with world famous cardiology researchers will attract young cardiologists to the sphere of cardiovascular research. -

Mamcos Final
For Circulation to Members e-Synergy Maulana Azad Medical College Old Students Association’s e-News Letter President Treasurer Secretary Dr. Sanjay Sood Dr. M.L. Sachdeva Dr. Ashwini Dalmiya M: 9811683807 M: 9818015188 M: 9811542055 Room : 309, 3rd Floor, Main College Building, Maulana Azad Medical College, MAY 2019 Bahadur Shah Zafar Marg, New Delhi-110002 Ph.: 23237029, Telefax: 91-11-23237029 email:[email protected], Website: www.mamcos.org e-Synergy From the Dean’s Desk, Dr. Sanjay Tyagi M.D. (Medicine), DM (Cardiology) FAMS, FICA, FESC, FACC (USA) DEAN Maulana Azad Medical College & Associated Hospitals • Govind Ballabh Pant Institute of Postgraduates • Medical Education & Research • Lok Nayak Hospital • Guru Nanak Eye Center Bahadur Shah Zafar Marg New Delhi-110002 (India) Ph. : +91-11-23231478, 23231438 Fax : +91-11- 23235574 Extn. : 101-102 E-mail : [email protected] It is indeed a great pleasure to extend my greetings and best wishes to MAMCOS on this wonderful initiative to launch a e-newsletter. This is a great moment that offers an opportunity to share knowledge, encourage professional networking and connect to all generations of Maulanians worldwide. Moving forwards the next logical step in the evolution of this initiative would be for this newsletter to become a great link across various associations and chapters of MAMC Alumni in different parts of the world. I extend my heartiest greetings to each one of you. (Dr. Sanjay Tyagi) President’s Pen... In the Diamond jubilee Year of MAMC I am privilegedand honoured to address you as the President of MAMCOS. Dear Friends MAMCOS is aunique Alumnus Organization which has grown in great strength over the years on the foresight and hard work of its founders, Past presidents and dedication of its dynamic Executive members. -

10596/2018 and 10605/2018, No Writ Petition Relatin
09.11.2020 DELETION NOTE 1.W.P.(C) 8162/2020 LISTED BEFORE HON'BLE DB-I AT ITEM NO 10 IS DELETED AS THE SAME IS LISTED BEFORE HON'BLE DB-II. 2.W.P.(CRL) 1830/2020 LISTED BEFORE HON'BLE DB-III AT ITEM NO 3 IS DELETED AS THE SAME IS LISTED BEFORE HON'BLE DB-V. 3.W.P.(C)7890/2019 LISTED BEFORE HON'BLE DB-VII AT ITEM NO 2 IS DELETED AS THE SAME IS LISTED BEFORE HON'BLE MR. JUSTICE J.R. MIDHA (SINGLE BENCH). NOTE THIS IS FOR INFORMATION OF ALL THE ADVOCATES/LITIGANTS THAT W.E.F. 19.10.2020 ALL FRESH PETITIONS/APPEALS SHALL BE ACCOMPANIED WITH THE REQUISITE ADVOCATES WELFARE STAMP OF RS. 25/-. THE CASES WHICH ARE NOT ACCOMPANIED WITH THE ADVOCATES WELFARE STAMP OF RS. 25/- AS PROVIDED IN SECTION 27 OF THE ADVOCATES WELFARE FUND ACT, 2001 SHALL BE RETURNED UNDER OBJECTION. REGISTRAR(FILING) Pursuant to the directions given by Hon'ble Mr. Justice J.R.Midha in W.P.(C) 10596/2018 and 10605/2018, no writ petition relating to an industrial dispute shall be listed unless the petitioner discloses the “Exceptional circumstances” in the synopsis as well as in the opening paras of the writ petition for exercising writ jurisdiction. If the writ-petitioner does not disclose the “exceptional circumstances” in the writ petition, the Registry will return such petition under objection. HIGH COURT OF DELHI AT NEW DELHI No.: 573/RG/DHC/2020 Dated: 23.10.2020 OFFICE ORDER All the Advocates/parties-in-person are hereby informed that with effect from 02.11.2020 all caveats shall be permitted to be lodged through e-filing module only. -
Direct Allotment Data for Plot Status ALLOTED, RESTORED,CANCELLED,RESUME,DEACTIVE Plots As on 20/07/2015
Direct Allotment data for plot status ALLOTED, RESTORED,CANCELLED,RESUME,DEACTIVE plots as on 20/07/2015. Urban Estate sectorid plot name surname fathername father surname Original Mode Of Allotment Sub Plot Name number Reservation Allotment Date Category Status CategoryCode Code Panchkula 6 472 A MALHOTRA A.N MALHOTRA GENER DIREC 28/11/1975 2.00K ALLOT Karnal 8P2 381 A . K KAUSHAL HARI KISHAN KAUSHAL GENER DIREC 6/6/1996 10.0M RESTO Faridabad 21A 430 A C JOLLY LACHHMAN DASS JOLLY GENER DIREC 16/05/1973 1.00K ALLOT Faridabad 55 1245 A C SHARMA HAR BHAGWAN DASS GENER DIREC 15/11/1994 14.0M ALLOT Faridabad 31 634 A K KHURANA SH P R KHURANA GENER DIREC 2/11/1994 4.00M RESTO Faridabad 21A 740 A K JAIN BANWARI LAL JAIN GENER DIREC 2/7/1974 1.00K ALLOT Faridabad 21A 762 A K CHATURVEDI J K CHATURVEDI HGSER DIREC 11/1/1977 1.00K ALLOT Faridabad 8 833 A L AHUJA TARA CHAND AHUJA GENER DIREC 27/02/1981 10.0M ALLOT Faridabad 37 143 A L KHURANA RAM DITTA MAL GENER DIREC 9/10/1980 6.00M ALLOT Faridabad 21A 250P A M SEHGAL B R SEHGAL GENER DIREC 22/08/1974 1.00K ALLOT Faridabad 21A 770 A M ABDUL HAMID MOHAMMED HAMID GENER DIREC 2/7/1974 1.00K ALLOT Faridabad 28 1111 A N ARORA MELA RAM GENER DIREC 2/4/1980 10.0M RESTO Panchkula 6 157 A N CHAUDHARY V D CHAUDHARY GENER DIREC 22/01/1974 2.00K ALLOT Faridabad 15A 947 A P KASHYAP RAJ BAL GENER DIREC 10/9/1981 10.0M RESTO Faridabad 19 1327P A P SINGH BALWANT SINGH GENER DIREC 13/05/1975 10.0M ALLOT Panchkula 4MDC 338 A P SANWARIA D R SANWARIA GENER DIREC 5/4/1991 1.00K ALLOT Panchkula 4 289 A P SINGH JOGINDER SINGH GENER DIREC 28/01/1986 14.0M ALLOT Panchkula 17 377 A R KAKKAR PIRMAL DASS GENER DIREC 14/11/1975 10.0M ALLOT Faridabad 21A 540 A S GUPTA BHAGWAN DASS GUPTA HGSER DIREC 2/7/1974 1.00K ALLOT Faridabad 21A 764P A S VAIDYA B.S. -
ICMR Guidelines (2017)
NATIONAL ETHICAL GUIDELINES FOR BIOMEDICAL AND HealTH Research INVOLVING HUMAN PARTicipanTS INDIAN COUNCIL OF MEDICAL RESEARCH 2017 Published by: Director-General Indian Council of Medical Research New Delhi 110 029 www.icmr.nic.in ISBN: 978-81-910091-94 October, 2017 Price: ₹ 500.00 © Copyright Indian Council of Medical Research The use of content from this book is permitted for all non-commercial purposes like education, training and dissemination of information, including translation, quotation and reproduction, in any medium, but the content must not be changed and full acknowledgement of the source must be clearly stated. Indian Council of Medical Research (ICMR) shall not be held liable for any damages whatsoever as a result of the use or application of the contents of this document. ICMR reserves the right to update and change the contents without notice and accepts no liability for any errors or omissions in this regard. Any alteration to the original content brought about by display or access through different media and for any inaccurate advice or information that is provided by sources reached via linkages or references to this document is not the responsibility of ICMR. Design and layout: Tejeswini Padma, Kalyani Thakur, Rajib K Hazam and Monesh B Vishwakarma TABLE OF CONTENTS Message from Hon’ble Union Minister for Health and Family Welfare, Government of India ix Foreword by DG ICMR and Secretary DHR x Message from President, Medical Council of India xi Preface by Chairperson, Central Ethics Committee on Human Research xii