Fundamentals of Aerospace Medicine, Fourth Edition
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Chapter 23 ENVIRONMENTAL EXTREMES: ALTERNOBARIC
Environmental Extremes: Alternobaric Chapter 23 ENVIRONMENTAL EXTREMES: ALTERNOBARIC RICHARD A. SCHEURING, DO, MS*; WILLIAM RAINEY JOHNSON, MD†; GEOFFREY E. CIARLONE, PhD‡; DAVID KEYSER, PhD§; NAILI CHEN, DO, MPH, MASc¥; and FRANCIS G. O’CONNOR, MD, MPH¶ INTRODUCTION DEFINITIONS MILITARY HISTORY AND EPIDEMIOLOGY Altitude Aviation Undersea Operations MILITARY APPLIED PHYSIOLOGY Altitude Aviation Undersea Operations HUMAN PERFORMANCE OPTIMIZATION STRATEGIES FOR EXTREME ENVIRONMENTS Altitude Aviation Undersea Operations ONLINE RESOURCES FOR ALTERNOBARIC ENVIRONMENTS SUMMARY *Colonel, Medical Corps, US Army Reserve; Associate Professor, Military and Emergency Medicine, Uniformed Services University of the Health Sci- ences, Bethesda, Maryland †Lieutenant, Medical Corps, US Navy; Undersea Medical Officer, Undersea Medicine Department, Naval Medical Research Center, Silver Spring, Maryland ‡Lieutenant, Medical Service Corps, US Navy; Research Physiologist, Undersea Medicine Department, Naval Medical Research Center, Silver Spring, Maryland §Program Director, Traumatic Injury Research Program; Assistant Professor, Military and Emergency Medicine, Uniformed Services University of the Health Sciences, Bethesda, Maryland ¥Colonel, Medical Corps, US Air Force; Assistant Professor, Military and Emergency Medicine, Uniformed Services University of the Health Sciences, Bethesda, Maryland ¶Colonel (Retired), Medical Corps, US Army; Professor and former Department Chair, Military and Emergency Medicine, Uniformed Services University of the Health Sciences, -

Thermoregulatory Correlates of Nausea in Rats and Musk Shrews
www.impactjournals.com/oncotarget/ Oncotarget, Vol. 5, No. 6 Thermoregulatory correlates of nausea in rats and musk shrews Sukonthar Ngampramuan1, Matteo Cerri2, Flavia Del Vecchio2, Joshua J. Corrigan3, Amornrat Kamphee1, Alexander S. Dragic3, John A. Rudd4, Andrej A. Romanovsky3, and Eugene Nalivaiko5 1 Research Center for Neuroscience and Institute of Molecular Bioscience, Mahidol University, Bangkok, Thailand; 2 Department of Biomedical and Motor Sciences, University of Bologna, Bologna, Italy; 3 FeverLab, Trauma Research, St. Joseph’s Hospital and Medical Center, Phoenix, AZ, USA; 4 School of Biomedical Sciences, Chinese University of Hong Kong, Hong Kong, China; 5 School of Biomedical Sciences and Pharmacy, University of Newcastle, Newcastle, NSW, Australia. Correspondence to: Eugene Nalivaiko, email: [email protected] Correspondence to: Andrej A. Romanovsky, email: [email protected] Keywords: nausea, chemotherapy, temperature, hypothermia. Received: December 21, 2013 Accepted: February 21, 2014 Published: February 22 2014 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. ABSTRACT: Nausea is a prominent symptom and major cause of complaint for patients receiving anticancer chemo- or radiation therapy. The arsenal of anti-nausea drugs is limited, and their efficacy is questionable. Currently, the development of new compounds with anti-nausea activity is hampered by the lack of physiological correlates of nausea. Physiological correlates are needed because common laboratory rodents lack the vomiting reflex. Furthermore, nausea does not always lead to vomiting. Here, we report the results of studies conducted in four research centers to investigate whether nausea is associated with any specific thermoregulatory symptoms. -

Medical Aspects of Harsh Environments, Volume 2, Chapter
Medical Aspects of Harsh Environments, Volume 2 Chapter 32 PRESSURE CHANGES AND HYPOXIA IN AVIATION R. M. HARDING, BSC, MB BS, PHD* INTRODUCTION THE ATMOSPHERE Structure Composition THE PHYSIOLOGICAL CONSEQUENCES OF RAPID ASCENT TO ALTITUDE Hypoxia Hyperventilation Barotrauma: The Direct Effects of Pressure Change Altitude Decompression Sickness LIFE-SUPPORT SYSTEMS FOR FLIGHT AT HIGH ALTITUDE Cabin Pressurization Systems Loss of Cabin Pressurization Personal Oxygen Equipment SUMMARY *Principal Consultant, Biodynamic Research Corporation, 9901 IH-10 West, Suite 1000, San Antonio, Texas 78230; formerly, Royal Air Force Consultant in Aviation Medicine and Head of Aircrew Systems Division, Department of Aeromedicine and Neuroscience of the UK Centre for Human Science, Farnborough, Hampshire, United Kingdom 984 Pressure Changes and Hypoxia in Aviation INTRODUCTION The physiological consequences of rapid ascent and life-support engineers has established reliable to high altitude are a core problem in the field of techniques for safe flight at high altitudes, as demon- aerospace medicine. Those who live and work in strated by current atmospheric flight in all its forms, mountain terrain experience a limited range of al- military and civilian, from balloon flights to sail planes titudes and have time to adapt to the hypoxia ex- to supersonic aircraft and spacecraft. Although reli- perienced at high terrestrial elevations. In contrast, able cabin pressurization and oxygen delivery systems flyers may be exposed to abrupt changes in baro- have greatly reduced incidents and accidents due to metric pressure and to acute, life-threatening hy- hypoxia in flight, constant vigilance is required for poxia (see also Chapter 28, Introduction to Special their prevention. -

Bluemagazine Caribbeanexplor
38 SABA KITTS /ST. LUXURY LIVEABOARD Caribbean Explorer II The liveaboard experience is luxurious and focused on one thing—maximum diving pleasure. Hard-core divers who don’t mind interacting with a small group out at sea for a week, would love this excursion. By SOLOMON BAKSH Tent Reef is probably the most striking reef in Saba with vibrant sponges, enormous gorgonians and teeming with fish life 39 THE Boat at. Dive. Sleep…well, sleeping my shoes into. That was the last I saw of crew members on board: Tim Heaton, is optional. It’s a liveaboard them until seven days later. Captain, USA; Chris Johnson, Engineer, lifestyle—getting up from your I was the first guest to arrive on board USA; Nichol Schilling, Purser, Germany; Ebed every day for a week with a the boat and was given the best location to Instructors Claire Keany, Scotland; Brett view of a breathtaking sunrise from your set up my gear—right next to the exit. Lockhoff, USA; Joe Lamontage, Canada. window, the ocean always in sight, a hot The person responsible for keeping all of us breakfast and another day of great diving. Amenities well fed was chef, Sarah Dauphinee, USA. It’s the nature of these trips that make The Caribbean Explorer II was well laid Every day was an epicurean delight with them so attractive. Plying the open ocean out. The upper deck housed the galley, air- Sarah serving up Mexican, Mediterranean, to different dive sites every day and over conditioned dining area and sun deck. Italian, Caribbean and BBQ dishes. -

Carbon Monoxide Poisoning
Carbon Monoxide Department of Boating and Waterways www.BoatResponsibly.com Exposure to CO in large amounts or for a long duration results in death. Carbon monoxide (CO) is an odorless, colorless gas in the exhaust produced in gasoline engines. Boats release CO through the exhaust ports of vessels that are either idling or underway. When inhaled, CO replaces oxygen in tissues. What are the symptoms of carbon monoxide poisoning? Symptoms of CO poisoning may include nausea, dizziness, confusion, headache and fainting; however, people often mistakenly attribute these symptoms to too much alcohol, sun, and noise, or to motion sickness from the water or exhaustion. How are people exposed to carbon monoxide in a marine environment? Traditionally, CO poisonings have occurred on houseboats, vessels with overhead canopies or other vessels that have poor ventilation. CO also accumulates onboard a vessel through a process known as the ‘station wagon effect.’ This occurs as air moves around a boat and forms a low pressure area immediately behind the broad, flat transom. CO from the exhaust system enters the low-pressure area and is fed back into the cockpit and into the cabin. Many cases of carbon monoxide inhalation have involved a recreational activity known as ‘teak surfing’. ‘Teak surfing’ involves holding onto the swim platform or transom of an underway vessel to bodysurf on the wake of the vessel. As of January 1, 2005, ‘teak surfing’ and other similar recreational activities are against the law in California. How common is carbon monoxide poisoning in a marine environment? Nationwide, between 1990 and 2004, there were 571 reported boating-related CO poisonings, including 113 deaths; 43 in California alone. -

Discover Scuba
Discover Scuba Come explore the amazing underwater world in the Bradford Woods swimming pool with a maximum depth of 5 ft. Participation requirements: -Minimum age of 12 -PADI Liability release -RSTC Medical History form— To be completed prior to camp with personal physician and submitted during registration. Discover Scuba or Medical History Questions? Bob Kessler [email protected] Non-Agency Disclosure and Acknowledgment Agreement In European Union and European Free Trade Association countries use alternative form. Please read carefully and fill in all blanks before signing. I understand and agree that PADI Members (“Members”), including _______________________________store/resort and/or any individual PADI Instructors and Divemasters associated with the program in which I am participat- ing, are licensed to use various PADI Trademarks and to conduct PADI training, but are not agents, employees or franchisees of PADI Americas, Inc, or its parent, subsidiary and affiliated corporations (“PADI”). I further understand that Member business activities are independent, and are neither owned nor operated by PADI, and that while PADI establishes the standards for PADI diver train- ing programs, it is not responsible for, nor does it have the right to control, the operation of the Members’ business activities and the day-to day conduct of PADI programs and supervision of divers by the Members or their associated staff. I further understand and agree on behalf of myself, my heirs and my estate that in the event of an injury or death during this activity, neither I nor my es- tate shall seek to hold PADI liable for the actions, inactions or negligence of _________________________________________store/resort and/or the instructors and divemasters associated with the activity. -

Medical Release Form
MEDICAL STATEMENT Participant Record (Confidential Information) Please read carefully before signing. This is a statement in which you are informed of some potential risks disease, a current cold or congestion, epilepsy, a severe medical involved in scuba diving and of the conduct required of you during problem or who is under the influence of alcohol or drugs should not the Shark Dive program. Your signature on this statement is required dive. If you have asthma, heart disease, other chronic medical for you to participate in the Shark Dive program offered by conditions or you are taking medications on a regular basis, you should consult your doctor and the instructor before participating in __________________________from Hampton Dive Center and this program, and on a regular basis thereafter upon completion. You Instructor will also learn from the instructor the important safety rules regarding breathing and equalization while scuba diving. Improper use of scuba Atlantis Marine World LLC located in the city of Riverhead, equipment can result in serious injury. You must be thoroughly state/province of New York. instructed in its use under direct supervision of a qualified professional to use it safely. Read this statement prior to signing it. You must complete this Medical Statement, which includes the medical questionnaire section, Medical Statement and Guidelines for Recreational Scuba Diver’s to enroll in the Shark Dive program. If you are a minor, you must Physical Examination to take to your physician are attached to this have this Statement signed by a parent or guardian. form. Diving is an exciting and demanding activity. -
For Presenting Injury Data Using ICD-10-CM External Cause of Injury Codes
PROPOSED FRAMEWORK for Presenting Injury Data using ICD-10-CM External Cause of Injury Codes NONFATAL UNINTENTIONAL MOTOR VEHICLE-TRAFFIC OCCUPANT INJURY RATES, UNITED STATES, 2012 2000 1500 1000 500 RATE PER 100,000 POPULATION RATE MALE FEMALE 0 00–04 yrs 05–09 yrs 10–14 yrs 15–19 yrs 20–24 yrs AGE GROUP U.S. Department of Health and Human Services Centers for Disease Control and Prevention Proposed Framework for Presenting Injury Data using ICD-10-CM External Cause of Injury Codes Joseph L Annest, PhD, MS,1 Holly Hedegaard, MD, MSPH,2 Li-Hui Chen, PhD,2 Margaret Warner, PhD,2 Equater (Ann) Smalls1 March 2014 A Collaboration of CDC’s National Center for Injury Prevention and Control,1 Atlanta, GA and National Center for Health Statistics,2 Hyattsville, MD Proposed Framework for Presenting Injury Data using ICD-10-CM External Cause of Injury Codes is a publication of The National Center for Injury Prevention and Control and the National Center for Health Statistics within the Centers for Disease Control and Prevention. Centers for Disease Control and Prevention Thomas R. Frieden, MD, MPH, Director National Center for Injury Prevention and Control Daniel M. Sosin, MD, MPH, FACP, Acting Director National Center for Health Statistics Charles J. Rothwell, MBA, MS, Director Suggested citation: Annest, J., Hedegaard, H., Chen, L., Warner, M., and Small, E. (2014). Proposed Framework for Presenting Injury Data using ICD-10-CM External Cause of Injury Codes. Atlanta, GA: National Center for Injury Prevention and Control, National Center for Health Statistics, Centers for Disease Control and Prevention. -

What Is Motion Sickness?
What is Motion Sickness? SYMPTOMS Originally adapted with permission from a publication by the American Academy of Otolaryngology—Head and Neck Surgery, Alexandria, Virginia, with edits by Dr. Jeremy Hinton. CONFLICTING SIGNALS Motion sickness is the most common medical problem associated with travel. Symptoms appear when the central nervous system WHAT IS MOTION SICKNESS? receives conflicting messages from the visual system and Some people experience nausea and even vomiting when riding in an the vestibular system airplane, automobile, or amusement park ride. This is called motion in the inner ears. sickness. Motion sickness is often caused by multi-axial motion and acceleration, especially if the eyes are seeing one thing while the body experiences another. An example of this would be if a person was sitting in the back seat of a car looking out the side window while the car ARTICLE accelerates down a hill and turns a corner at the same time. The sensation is often temporary, but for many it continues for a prolonged period of time, resulting in extreme discomfort and anxiety. Early symptoms of motion sickness may include nausea, increased salivation, belching, feeling clammy (diapohoretic), hyperventilating, and 091 a feeling of general unease. Because hyperventilation and progressive nausea are so unsettling, many people will report a feeling of impending doom that can lead to serious complications such as difficulty breathing, blood pressure drops (especially orthostatic hypotension), and even DID THIS ARTICLE passing out (syncope). Motion HELP YOU? sickness itself will not cause these SUPPORT VEDA @ symptoms, but can lead to a person feeling overwhelmed. VESTIBULAR.ORG Many people experience motion sickness when riding on a boat or ship. -
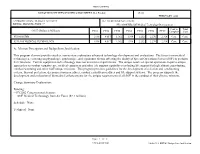
A. Mission Description and Budget Item Justification
UNCLASSIFIED RDT&E BUDGET ITEM JUSTIFICATION SHEET (R-2 Exhibit) DATE FEBRUARY 2002 APPROPRIATION / BUDGET ACTIVITY R-1 ITEM NOMENCLATURE RDT&E, DEFENSE-WIDE / 7 PE1160407BB SOF Medical Technology Development Cost to Total COST (Dollars in Millions) FY01 FY02 FY03 FY04 FY05 FY06 FY07 Complete Cost PE1160407BB 1.996 4.017 1.962 1.994 2.232 2.270 2.314 Cont. Cont. S275 SOF MEDICAL TECHNOLOGY 1.996 4.017 1.962 1.994 2.232 2.270 2.314 Cont. Cont. A. Mission Description and Budget Item Justification This program element provides studies, non-system exploratory advanced technology development and evaluations. The focus is on medical technologies, centering on physiologic, psychologic, and ergonomic factors affecting the ability of Special Operations Forces (SOF) to perform their missions. Current equipment and technology does not meet force requirements. The unique nature of special operations requires unique approaches to combat casualty care, medical equipment and other life support capabilities including life support for high altitude parachuting, combat swimming and other SOF unique missions. This program provides guidelines for the development of selection and conditioning criteria, thermal protection, decompression procedures, combat casualty procedures and life support systems. The program supports the development and evaluation of biomedical enhancements for the unique requirements of all SOF in the conduct of their diverse missions. Change Summary Explanation: Funding: -- FY2002 Congressional Actions: SOF Medical Technology from Air Force ($2.1 million) Schedule: None. Technical: None Page: 1 of 2 UNCLASSIFIED Exhibit R-2, RDT&E Budget Item Justification UNCLASSIFIED RDT&E BUDGET ITEM JUSTIFICATION SHEET (R-2 Exhibit) DATE FEBRUARY 2002 APPROPRIATION / BUDGET ACTIVITY R-1 ITEM NOMENCLATURE RDT&E, DEFENSE-WIDE / 7 PE1160407BB SOF Medical Technology Development B. -
Medical Aspects of Harsh Environments, Volume 2, Chapter
Medical Aspects of Harsh Environments, Volume 2 Chapter 34 MILITARY SPACEFLIGHT F. ANDREW GAFFNEY, MD*; AND JAMES P. BAGIAN, MD† INTRODUCTION ORBITAL MECHANICS AND FREE FALL LIVING IN SPACE Life Support Physiological Adaptation to Microgravity Space Radiation RETURN TO GRAVITY FUTURE MILITARY SPACE MISSIONS AND INTERPLANETARY EXPLORATION SUMMARY *Colonel, US Air Force Reserve, Medical Corps; Senior Flight Surgeon and Astronaut; Division of Cardiology, Vanderbilt University School of Medicine, Nashville, Tennessee †Colonel, US Air Force Reserve, Medical Corps; Senior Flight Surgeon and Astronaut; Director, Department of Veterans Affairs, National Center for Patient Safety, Ann Arbor, Michigan 48106 1028 Military Spaceflight INTRODUCTION Support of life in space is surely the most demand- microgravity and (2) readaptation on return to Earth ing technical challenge undertaken by humankind, or another celestial body’s gravity field. Their dis- and requires close collaboration among physicians, cussion concluded with the telling observation that physiologists, engineers, and professionals with a “We can only guess the facts here: experiments must variety of other skills. This chapter is designed to help be the final answer.”1 the reader develop a basic understanding not only of More than 1 decade later (12 Apr 1961 and 20 Feb the challenges of life support in the space environ- 1962, respectively), the brief orbital flights of Yuri ment but also of the medical issues related to health Gagarin (1 h, 48 min) and John Glenn (4 h, 55 min) maintenance in physiological readaptation on return showed that human orbital flight was indeed pos- to the planetary surface. The topics should be of in- sible. -

Safety Activity Checkpoints 2021 Edition @ April 1, 2021
- 2021 SAFETY ACTIVITY CHECKPOINTS 2021 EDITION @ APRIL 1, 2021 Table of Contents Introduction ........................................................................................................................................................ 4 Standard Safety Guidelines ............................................................................................................................... 4 Coronavirus Safety in Girl Scouts ...................................................................................................................... 7 Have an Emergency Action Plan (EAP) ............................................................................................................. 8 Understanding Which Activities Are Not Permitted .......................................................................................... 12 Chartered Aircraft Trips and Aviation ............................................................................................................... 14 Other Actions Girls and Volunteers Should Not Take ...................................................................................... 14 First Aid ........................................................................................................................................................... 14 Overall Health, Well Being and Inclusivity ........................................................................................................ 17 Transporting Girls ...........................................................................................................................................