Therapeutic Class Overview Restless Legs Syndrome
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Sustained Release Tablet Comprising Pramipexole
(19) & (11) EP 2 172 199 A1 (12) EUROPEAN PATENT APPLICATION (43) Date of publication: (51) Int Cl.: 07.04.2010 Bulletin 2010/14 A61K 31/428 (2006.01) A61K 9/20 (2006.01) A61K 9/28 (2006.01) (21) Application number: 09178277.1 (22) Date of filing: 25.07.2003 (84) Designated Contracting States: • Lee, Ernest, J. AT BE BG CH CY CZ DE DK EE ES FI FR GB GR Kalamazoo, MI 49009 (US) HU IE IT LI LU MC NL PT RO SE SI SK TR • Martino, Alice, C. Kalamazoo, MI 49009 (US) (30) Priority: 25.07.2002 US 398427 P • Noack, Robert, M. 25.07.2002 US 398447 P Grand Rapids, MI 49506 (US) 28.08.2002 US 406609 P • Reo, Joseph, P. 18.06.2003 US 479387 P Kalamazoo, MI 49009 (US) • Skoug, Connie, J. (62) Document number(s) of the earlier application(s) in Portage, MI 49024 (US) accordance with Art. 76 EPC: 03771898.8 / 1 536 791 (74) Representative: Summers, Victoria Clare Pfizer Limited (71) Applicant: Pharmacia Corporation European Patent Department Peapack, NJ 07977 (US) Ramsgate Road Sandwich, Kent CT13 9NJ (GB) (72) Inventors: • Amidon, Gregory, E. Remarks: Portage, MI 49024 (US) This application was filed on 08-12-2009 as a • Ganorkar, Loksidh, D. divisional application to the application mentioned Kalamazoo, MI 49009 (US) under INID code 62. • Heimlich, John, M. Portage, MI 49002 (US) (54) Sustained release tablet comprising pramipexole (57) A sustained - release pharmaceutical composi- hydrophilic polymer and astarch having a tensile strength tion in a form of an orally deliverable tablet comprising of at least about 0.15kNcm -2 at a solid fraction represent- an active pharmaceutical agent having solubility not less ative of the tablet. -

Restless Legs Syndrome in Patients with Epilepsy Under Levetiracetam Monotherapy
Original Article / Özgün Makale DODO I: 10.4274/ I: 10.4274/jtsm.xxxjtsm.69188 Journal of Turkish Sleep Medicine 2018;5:12-6 Restless Legs Syndrome in Patients with Epilepsy Under Levetiracetam Monotherapy Levetirasetam Monoterapisi Altında Epilepsi Hastalarında Huzursuz Bacak Sendromu Gülnihal Kutlu, Fatma Genç*, Yasemin Ünal, Dilek Aslan Öztürk, Abidin Erdal*, Yasemin Biçer Gömceli* Muğla Sıtkı Koçman University Faculty of Medicine, Department of Neurology, Muğla, Turkey *University of Health Sciences, Antalya Training and Research Hospital, Clinic of Neurology, Antalya, Turkey Abstract Öz Objective: Restless Legs syndrome (RLS) is a frequent neurological Amaç: Huzursuz Bacak sendromu (HBS) sık görülen bir nörolojik disease. Levetiracetam (LEV) is an effective and broad-spectrum hastalıktır. Levetirasetam (LEV) etkili ve geniş spektrumlu bir antiepileptik anticonvulsant drug. The aim of this study is to investigate the frequency ilaçtır. Bu çalışmanın amacı epilepsi tanısı ile LEV monoterapisi alan of RLS in patients diagnosed with epilepsy who took LEV monotherapy. hastalarda HBS sıklığını araştırmaktır. Materials and Methods: Two neurologists were reviewed the files of Gereç ve Yöntem: Epilepsi polikliniğinde takip edilen 1680 hastanın 1680 patients, who were followed in epilepsy outpatient clinic. One dosyası iki nörolog tarafından gözden geçirildi. En az 6 aydır LEV hundred seven patients under LEV monotherapy for at least six months monoterapisi alan 107 hasta ve 120 sağlıklı kontrol çalışmaya alındı. and 120 healthy controls were included in the study. The criteria for the International Restless Legs Syndrome Study Group were taken into HBS değerlendirmesi için Uluslararası Huzursuz Bacak Sendromu Çalışma consideration for the assessment of RLS. Grubu’nun kriterleri göz önüne alındı. Results: The mean age of patient group was 38.26±17.39 years, while Bulgular: Sağlıklı kontrollerin ortalama yaşı 39,17±16,12 yıl iken, the mean age of healthy controls was 39.17±16.12 years. -

Eslicarbazepine Acetate: a New Improvement on a Classic Drug Family for the Treatment of Partial-Onset Seizures
Drugs R D DOI 10.1007/s40268-017-0197-5 REVIEW ARTICLE Eslicarbazepine Acetate: A New Improvement on a Classic Drug Family for the Treatment of Partial-Onset Seizures 1 1 1 Graciana L. Galiana • Angela C. Gauthier • Richard H. Mattson Ó The Author(s) 2017. This article is an open access publication Abstract Eslicarbazepine acetate is a new anti-epileptic drug belonging to the dibenzazepine carboxamide family Key Points that is currently approved as adjunctive therapy and monotherapy for partial-onset (focal) seizures. The drug Eslicarbazepine acetate is an effective and safe enhances slow inactivation of voltage-gated sodium chan- treatment option for partial-onset seizures as nels and subsequently reduces the activity of rapidly firing adjunctive therapy and monotherapy. neurons. Eslicarbazepine acetate has few, but some, drug– drug interactions. It is a weak enzyme inducer and it Eslicarbazepine acetate improves upon its inhibits cytochrome P450 2C19, but it affects a smaller predecessors, carbamazepine and oxcarbazepine, by assortment of enzymes than carbamazepine. Clinical being available in a once-daily regimen, interacting studies using eslicarbazepine acetate as adjunctive treat- with a smaller range of drugs, and causing less side ment or monotherapy have demonstrated its efficacy in effects. patients with refractory or newly diagnosed focal seizures. The drug is generally well tolerated, and the most common side effects include dizziness, headache, and diplopia. One of the greatest strengths of eslicarbazepine acetate is its ability to be administered only once per day. Eslicar- 1 Introduction bazepine acetate has many advantages over older anti- epileptic drugs, and it should be strongly considered when Epilepsy is a common neurological disorder affecting over treating patients with partial-onset epilepsy. -

Chapter 25 Mechanisms of Action of Antiepileptic Drugs
Chapter 25 Mechanisms of action of antiepileptic drugs GRAEME J. SILLS Department of Molecular and Clinical Pharmacology, University of Liverpool _________________________________________________________________________ Introduction The serendipitous discovery of the anticonvulsant properties of phenobarbital in 1912 marked the foundation of the modern pharmacotherapy of epilepsy. The subsequent 70 years saw the introduction of phenytoin, ethosuximide, carbamazepine, sodium valproate and a range of benzodiazepines. Collectively, these compounds have come to be regarded as the ‘established’ antiepileptic drugs (AEDs). A concerted period of development of drugs for epilepsy throughout the 1980s and 1990s has resulted (to date) in 16 new agents being licensed as add-on treatment for difficult-to-control adult and/or paediatric epilepsy, with some becoming available as monotherapy for newly diagnosed patients. Together, these have become known as the ‘modern’ AEDs. Throughout this period of unprecedented drug development, there have also been considerable advances in our understanding of how antiepileptic agents exert their effects at the cellular level. AEDs are neither preventive nor curative and are employed solely as a means of controlling symptoms (i.e. suppression of seizures). Recurrent seizure activity is the manifestation of an intermittent and excessive hyperexcitability of the nervous system and, while the pharmacological minutiae of currently marketed AEDs remain to be completely unravelled, these agents essentially redress the balance between neuronal excitation and inhibition. Three major classes of mechanism are recognised: modulation of voltage-gated ion channels; enhancement of gamma-aminobutyric acid (GABA)-mediated inhibitory neurotransmission; and attenuation of glutamate-mediated excitatory neurotransmission. The principal pharmacological targets of currently available AEDs are highlighted in Table 1 and discussed further below. -

Clinical Review, Adverse Events
Clinical Review, Adverse Events Drug: Carbamazepine NDA: 16-608, Tegretol 20-712, Carbatrol 21-710, Equetro Adverse Event: Stevens-Johnson Syndrome Reviewer: Ronald Farkas, MD, PhD Medical Reviewer, DNP, ODE I 1. Executive Summary 1.1 Background Carbamazepine (CBZ) is an anticonvulsant with FDA-approved indications in epilepsy, bipolar disorder and neuropathic pain. CBZ is associated with Stevens-Johnson syndrome (SJS) and Toxic Epidermal Necrolysis (TEN), closely related serious cutaneous adverse drug reactions that can be permanently disabling or fatal. Other anticonvulsants, including phenytoin, phenobarbital, and lamotrigine are also associated with SJS/TEN, as are members of a variety of other drug classes, including nonsteriodal anti-inflammatory drugs and sulfa drugs. The incidence of CBZ-associated SJS/TEN has been considered “extremely rare,” as noted in current U.S. drug labeling. However, recent publications and postmarketing data suggest that CBZ- associated SJS/TEN occurs at a much higher rate in some Asian populations, about 2.5 cases per 1,000 new exposures, and that most of this increased risk is in individuals carrying a specific human leukocyte antigen (HLA) allele, HLA-B*1502. This HLA-B allele is present in about 5- to 20% of many, but not all, Asian populations, and is also present in about 2- to 4% of South Asians/Indians. The allele is also present at a lower frequency, < 1%, in several other ethnic groups around the world (although likely due to distant Asian ancestry). About 10% of U.S. Asians carry HLA-B*1502. HLA-B*1502 is generally not present in the U.S. -

Parasite Linked to Dementia, Cognitive Impairment
May 2008 • www.clinicalneurologynews.com News 5 Parasite Linked to Dementia, Cognitive Impairment ARTICLES BY AMY ROTHMAN that 5 (12.5%) of treatment-naive patients but other lesions also can be related, and are SCHONFELD diagnosed with neurocysticercosis met located anywhere in the brain. Contributing Writer DSM IV criteria for dementia, significant- Humans become infected with neuro- ly more than the normal control group (P cysticercosis through consumption of food C HICAGO — Untreated central nervous less than .05). Major memory impairment or water contaminated with the feces of a system infection with the parasitic neuro- was found in 23 (57.5%). On a battery of NDRADE Taenia solium tapeworm carrier. The adult cysticercosis may present as cognitive im- cognitive tests that evaluated memory, at- A tapeworms are found only in the intestine pairment ranging from mild deficit to tention, praxis, and executive function, all of humans. Once the tapeworm lays its IAMPI DE full-blown dementia. those with neurocysticercosis demon- C eggs, the larvae may invade tissue and Neurocysticercosis is the most common strated one or more cognitive deficits, a through the bloodstream infect skeletal parasitic infection of the CNS. Even physi- significantly higher rate than observed for ANIEL muscles, the eyes, brain, and spinal cord. A . D R cians may be unaware of infection’s ad- the normal controls (P less than .05). In- D person can be infested by T. solium and be verse effects on cognition, according to Dr. terestingly, when compared with patients a carrier, but not develop cysticercosis. Daniel Ciampi de Andrade. with cryptogenic epilepsy, neurocysticer- Dr. -

Frequent Difficulties in the Treatment of Restless Legs Syndrome – Case Report and Literature Review
Psychiatr. Pol. 2015; 49(5): 921–930 PL ISSN 0033-2674 (PRINT), ISSN 2391-5854 (ONLINE) www.psychiatriapolska.pl DOI: http://dx.doi.org/10.12740/PP/35395 Frequent difficulties in the treatment of restless legs syndrome – case report and literature review Dominika Narowska 1, Milena Bożek 2, Katarzyna Krysiak 3, Jakub Antczak3, Justyna Holka-Pokorska1, Wojciech Jernajczyk3, Adam Wichniak1 1 Third Department of Psychiatry, Institute of Psychiatry and Neurology in Warsaw 2 First Department of Psychiatry, Institute of Psychiatry and Neurology in Warsaw 3 Department of Clinical Neurophysiology, Sleep Disorders Centre, Institute of Psychiatry and Neurology in Warsaw Summary Restless legs syndrome (RLS) is one of the most common sleep disorders. The purpose of this paper is a case description of the patient suffering from RLS, concurrent with numer- ous clinical problems. In our patient, during long-term therapy with a dopamine agonist (ropinirole), the phenomenon of the augmentation, defined as an increase in the severity of the RLS symptoms, was observed. The quality of life of the patient was significantly dete- riorated. Due to the augmentation of RLS symptoms the dopaminergic drug was gradually withdrawn, and the gabapentin as a second-line drug for the treatment of RLS was introduced. Because of the large increase of both insomnia and RLS symptoms during the reduction of ropinirole dose, clonazepam was temporarily introduced. In addition, in the neurological as- sessment of the distal parts of the lower limb sensory disturbances of vibration were found. The neurographic study confirmed axonal neuropathy of the sural nerves, which explained an incomplete response to dopaminergic medications. -

(12) United States Patent (10) Patent No.: US 8,486,621 B2 Luo Et Al
USOO8486.621B2 (12) United States Patent (10) Patent No.: US 8,486,621 B2 Luo et al. (45) Date of Patent: Jul. 16, 2013 (54) NUCLEICACID-BASED MATRIXES 2005. O130180 A1 6/2005 Luo et al. 2006/0084607 A1 4/2006 Spirio et al. (75) Inventors: ity, N. (US); Soong Ho 2007/01482462007/0048759 A1 3/20076/2007 Luo et al. m, Ithaca, NY (US) 2008.0167454 A1 7, 2008 Luo et al. 2010, O136614 A1 6, 2010 Luo et al. (73) Assignee: Cornell Research Foundation, Inc., 2012/0022244 A1 1, 2012 Yin Ithaca, NY (US) FOREIGN PATENT DOCUMENTS (*) Notice: Subject to any disclaimer, the term of this WO WO 2004/057023 A1 T 2004 patent is extended or adjusted under 35 U.S.C. 154(b) by 808 days. OTHER PUBLICATIONS Lin et al. (J Biomech Eng. Feb. 2004;126(1):104-10).* (21) Appl. No.: 11/464,184 Li et al. (Nat Mater. Jan. 2004:3(1):38-42. Epub Dec. 21, 2003).* Ma et al. (Nucleic Acids Res. Dec. 22, 1986;14(24):9745-53).* (22) Filed: Aug. 11, 2006 Matsuura, et al. Nucleo-nanocages: designed ternary oligodeoxyribonucleotides spontaneously form nanosized DNA (65) Prior Publication Data cages. Chem Commun (Camb). 2003; (3):376-7. Li, et al. Multiplexed detection of pathogen DNA with DNA-based US 2007/01 17177 A1 May 24, 2007 fluorescence nanobarcodes. Nat Biotechnol. 2005; 23(7): 885-9. Lund, et al. Self-assembling a molecular pegboard. JAm ChemSoc. Related U.S. Application Data 2005; 127(50): 17606-7. (60) Provisional application No. 60/722,032, filed on Sep. -

Parkinson's Disease Current Awareness Bulletin
Parkinson’s Disease Current Awareness Bulletin February 2018 A number of other bulletins are also available – please contact the Academy Library for further details If you would like to receive these bulletins on a regular basis please contact the library. For any references where there is a link to the full text please use your NHS Athens username & password to access If you would like any of the full references from those that do not have links we will source them for you. Contact us: Academy Library 824897/98 Email: [email protected] Title: Motor imagery training with augmented cues of motor learning on cognitive functions in patients with Parkinsonism Citation: International Journal of Therapy and Rehabilitation; 2018; vol. 25 (no. 1); p. 13 Author(s): Lama Saad El Din Mahmoud; Nawal Abd EL Raouf Abu Shady; Ehab Shaker Hafez Objective: Patients with Parkinsonism demonstrate impairments in cognitive functions, such as deficit in attention, planning, and working memory. The objective was to investigate the effect of motor imagery training with augmented cues of motor learning on cognitive functions in patients with Parkinsonism. Methods: A total of 30 patients from both sexes participated in this study. All of the patients had been diagnosed as idiopathic Parkinson patients experiencing cognitive dysfunction. The patients were randomly divided into two equal groups: the study group (n=15) received motor imagery training with augmented cues of motor learning and the specifically designed intervention. The control group (n=15) received conventional treatment (cognitive remediation therapy). The treatment took place three times a week for 6 weeks (18 sessions). -
Abstract Introduction Objectives Methods
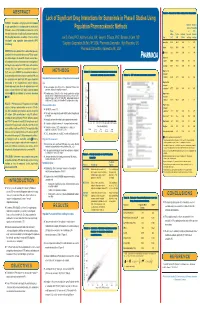
ABSTRACT Table 3. Summary of Drug Interaction Evaluation Lack of Significant Drug Interactions for Sumanirole in Phase II Studies Using PURPOSE: Sumanirole is a highly D -selective dopamine 2 Number of Number of receptor agonist that is in development for the treatment of Population Pharmacokinetic Methods Subjects Observations Parkinson's disease (PD). Metabolism of sumanirole and in Change on With vitro data indicate that clinically significant pharmacokinetic in Mean % of the Univariate Concomit- Concomit- (PK) drug-drug interactions are unlikely. This was further Joel S. Owen, PhD1, Kathryn Liolios, MA1, Gwyn A. D'Souza, PhD2, Barbara J. Carel, MS3 Drug CL/F SEM P Value ant Drug ant Drug investigated using population pharmacokinetic (PPK) 1 2 Amantadine 0.434 440.1 0.629 71 407 methodology. Cognigen Corporation, Buffalo, NY, USA; Pharmacia Corporation, High Wycombe, UK; 3Pharmacia Corporation, Kalamazoo, MI, USA Aspirin 0.601 196.3 0.349 77 496 METHODS: Data were obtained from 2 double-blind, placebo- β-Blockers* 2.22 154.1 0.066 22 144 controlled trials of sumanirole alone in early PD and sumani- role with levodopa in advanced PD. Patients received twice- Hypotensive † daily extended-release oral sumanirole doses ranging from 2 agents 0.0943 1124.1 0.882 128 815 to 48 mg/d. A one-compartment PPK model, with creatinine Levodopa‡ 0.907 100.0 0.281 111 200 clearance (CrCL) and gender as covariates of clearance Organic anion (CL/F), was used in NONMEM® to characterize the influence METHODS Figure 1. Sumanirole concentrations versus time transport of concomitantly administered drugs on sumanirole PK. -

The Management of Restless Legs Syndrome in Adults in Primary Care
The Management of Restless Legs Syndrome in Adults in Primary Care Victoria Birchall /Susan McKernan Midlands and Lancashire CSU December 2015 (Review date November 2018) VERSION CONTROL Version Number Date Amendments made 1.0 December Version 1. Approved 2015 Contents VERSION CONTROL ........................................................................................................... 2 1. INTRODUCTION ........................................................................................................... 3 2. PURPOSE AND SUMMARY ......................................................................................... 3 3. SCOPE .......................................................................................................................... 3 4. GUIDANCE .................................................................................................................... 3 5. REFERENCES .............................................................................................................. 8 6. ACKNOWLEDGEMENTS .............................................................................................. 8 Please access documents via the LMMG website to ensure the correct version is in use. 1. INTRODUCTION Restless Legs Syndrome (RLS), also known as Willis-Ekborn disease, is a common sensory motor neurological disorder which causes a characteristic, overwhelming and irresistible urge to move the limbs, usually the legs but can also additionally affect the arms – in addition to uncomfortable, abnormal sensations which -
![APTIOM (Eslicarbazepine Acetate) Is (S)-10-Acetoxy-10,11-Dihydro-5H Dibenz[B,F]Azepine-5-Carboxamide](https://docslib.b-cdn.net/cover/5440/aptiom-eslicarbazepine-acetate-is-s-10-acetoxy-10-11-dihydro-5h%C2%AD-dibenz-b-f-azepine-5-carboxamide-1265440.webp)
APTIOM (Eslicarbazepine Acetate) Is (S)-10-Acetoxy-10,11-Dihydro-5H Dibenz[B,F]Azepine-5-Carboxamide
HIGHLIGHTS OF PRESCRIBING INFORMATION Monitor and discontinue if another cause cannot be established. (5.2, 5.3, These highlights do not include all the information needed to use 5.4) APTIOM safely and effectively. See full prescribing information for • Hyponatremia: Monitor sodium levels in patients at risk or patients APTIOM. experiencing hyponatremia symptoms. (5.5) • Neurological Adverse Reactions: Monitor for dizziness, disturbance in gait APTIOM® (eslicarbazepine acetate) tablets, for oral use and coordination, somnolence, fatigue, cognitive dysfunction, and visual Initial U.S. Approval: 2013 changes. Use caution when driving or operating machinery. (5.6) • Withdrawal of APTIOM: Withdraw APTIOM gradually to minimize the ---------------------------RECENT MAJOR CHANGES------------------------- risk of increased seizure frequency and status epilepticus. (2.6, 5.7, 8.1) Indications and Usage (1) 9/2017 • Dosage and Administration (2) 9/2017 Drug Induced Liver Injury: Discontinue APTIOM in patients with jaundice Warnings and Precautions (5) 9/2017 or evidence of significant liver injury. (5.8) • Hematologic Adverse Reactions: Consider discontinuing. (5.10) ----------------------------INDICATIONS AND USAGE-------------------------- APTIOM is indicated for the treatment of partial-onset seizures in patients 4 ------------------------------ADVERSE REACTIONS------------------------------ years of age and older. (1) • Most common adverse reactions in adult patients receiving APTIOM (≥4% and ≥2% greater than placebo): dizziness, somnolence, nausea, headache, ----------------------DOSAGE AND ADMINISTRATION---------------------- diplopia, vomiting, fatigue, vertigo, ataxia, blurred vision, and tremor. (6.1) • Adult Patients: The recommended initial dosage of APTIOM is 400 mg • Adverse reactions in pediatric patients are similar to those seen in adult once daily. For some patients, treatment may be initiated at 800 mg once patients. daily if the need for seizure reduction outweighs an increased risk of adverse reactions.