The Clinical Use of Thyroid Function Tests
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Laboratory Procedure Manual
Laboratory Procedure Manual Analyte: Thyroid Stimulating Hormone Matrix: Serum Method: Microparticle Enzyme Immunoassay (MEIA) Method No.: Revised: as performed by: Coulston Foundation Alamogordo, New Mexico Contact: Ms. Love Julian 1-505-434-1725 Important Information for Users Coulston periodically refines these laboratory methods. It is the responsibility of the user to contact the person listed on the title page of each write-up before using the analytical method to find out whether any changes have been made and what revisions, if any, have been incorporated. Thyroid Stimulating Hormone NHANES 2001–2002 Public Release Data Set Information This document details the Lab Protocol for NHANES 2001-2002 data. Two laboratories performed this testing during 2001-2002. In order to maintain confidentiality of the participants the quality control summary statistics and graphs were combined to mask the individual analysis dates from the two laboratories. Methods for both labs are included in this release. The method for Lab18 analyte is included in this file. The method for Lab40 is described in a separate file. A tabular list of the released analytes follows: Lab Number Analyte SAS Label lab18 LBXTSH Thyroid Stimulating Hormone Page 2 of 11 Thyroid Stimulating Hormone NHANES 2001-2002 1. Summary of Test Principle and Clinical Relevance IMx Ultrasensitive hTSH II is a Microparticle Enzyme Immunoassay (MEIA) for the quantitative determination of human thyroid stimulating hormone (hTSH) in serum or plasma on the IMx analyzer. The IMx Ultrasensitive hTSH II assay is based on the MEIA technology. The IMx Ultrasensitive hTSH II reagents and sample are added to the reaction cell in the following sequence: The probe/electrode assembly delivers the sample and anti-hTSH coated microparticles to the incubation well of the reaction cell. -

Thyroid Hormones in Fetal Growth and Prepartum Maturation
A J FORHEAD and A L FOWDEN Thyroid hormones and fetal 221:3 R87–R103 Review development Thyroid hormones in fetal growth and prepartum maturation A J Forhead1,2 and A L Fowden1 Correspondence should be addressed 1Department of Physiology, Development and Neuroscience, University of Cambridge, Physiology Building, to A L Fowden Downing Street, Cambridge CB2 3EG, UK Email 2Department of Biological and Medical Sciences, Oxford Brookes University, Oxford OX3 0BP, UK [email protected] Abstract The thyroid hormones, thyroxine (T4) and triiodothyronine (T3), are essential for normal Key Words growth and development of the fetus. Their bioavailability in utero depends on " thyroid hormones development of the fetal hypothalamic–pituitary–thyroid gland axis and the abundance " intrauterine growth of thyroid hormone transporters and deiodinases that influence tissue levels of bioactive " maturation hormone. Fetal T4 and T3 concentrations are also affected by gestational age, nutritional and " neonatal adaptation endocrine conditions in utero, and placental permeability to maternal thyroid hormones, which varies among species with placental morphology. Thyroid hormones are required for the general accretion of fetal mass and to trigger discrete developmental events in the fetal brain and somatic tissues from early in gestation. They also promote terminal differentiation of fetal tissues closer to term and are important in mediating the prepartum maturational effects of the glucocorticoids that ensure neonatal viability. Thyroid hormones act directly through anabolic effects on fetal metabolism and the stimulation of fetal oxygen Journal of Endocrinology consumption. They also act indirectly by controlling the bioavailability and effectiveness of other hormones and growth factors that influence fetal development such as the catecholamines and insulin-like growth factors (IGFs). -
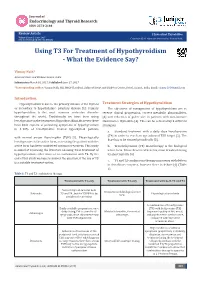
Using T3 for Treatment of Hypothyroidism - What the Evidence Say?
Journal of Endocrinology and Thyroid Research ISSN: 2573-2188 Review Article J Endocrinol Thyroid Res Volume 2 Issue 2- June 2017 Copyright © All rights are reserved by Vismay Naik, DOI: 10.19080/JETR.2017.02.555584 Using T3 For Treatment of Hypothyroidism - What the Evidence Say? Vismay Naik* Ashirvad Heart and Diabetes Centre, India Submission: March 01, 2017; Published: June 27, 2017 *Corresponding author: Vismay Naik, MD, MRCP (London), Ashirvad Heart and Diabetes Centre, Botad, Gujarat, India, Email: Introduction Hypothyroidism is due to the primary disease of the thyroid Treatment Strategies of Hypothyroidism or secondary to hypothalamic- pituitary disease [1]. Primary The objectives of management of hypothyroidism are to hypothyroidism is the most common endocrine disorder reverse clinical progression, correct metabolic abnormalities, throughout the world. Traditionally we have been using [3] and reduction of goiter size in patients with autoimmune levothyroxine in the treatment of hypothyroidism. However, there Hashimoto’s thyroiditis [4]. This can be achieved by 3 different have been reports of persisting symptoms of hypothyroidism strategies: in 5-10% of levothyroxine treated hypothyroid patients a. Standard treatment with a daily dose levothyroxine (T4) in order to reach an age adjusted TSH target [5]. The with normal serum thyrotrophin (TSH) [2]. Physiologically dose has to be titrated periodically [3]. levothyronine is the active form, so treating the patient with the active form has been considered optimum treatment. This study b. Triiodothyronine (T3) monotherapy is the biological is aimed at reviewing the literature on using T3 in treatment of hypothyroidism either alone or in combination with T4. By the its short half-life [6] end of this study we hope to answer the question, if the use of T3 active form. -
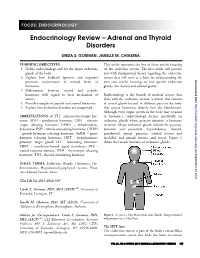
Endocrinology Review – Adrenal and Thyroid Disorders
FOCUS: ENDOCRINOLOGY Endocrinology Review – Adrenal and Thyroid Disorders LINDA S. GORMAN, JANELLE M. CHIASERA LEARNING OBJECTIVES This article represents the first of three articles focusing 1. Define endocrinology and list the major endocrine on the endocrine system. The first article will provide glands of the body. you with fundamental theory regarding the endocrine system that will serve as a basis for understanding the 2. Explain how feedback (positive and negative) Downloaded from promotes maintenance of normal levels of next two articles focusing on two specific endocrine hormones. glands, the thyroid and adrenal glands. 3. Differentiate between steroid and peptide hormones with regard to their mechanism of Endocrinology is the branch of medical science that action. deals with the endocrine system, a system that consists 4. Provide examples of peptide and steroid hormones. of several glands located in different parts of the body http://hwmaint.clsjournal.ascls.org/ 5. Explain how endocrine disorders are categorized. that secrete hormones directly into the bloodstream. Although every organ system in the body may respond ABBREVIATIONS: ACTH - adrenocorticotropic hor- to hormones, endocrinology focuses specifically on mone; ADH - antidiuretic hormone; CRH – cortico- endocrine glands whose primary function is hormone tropin releasing hormone; DHEA – dehydroepian- secretion. Major endocrine glands include the pituitary drosterone; FSH - follicle stimulating hormone; GHRH (anterior and posterior), hypothalamus, thyroid, - growth hormone -

A Randomized, Masked Study of Triiodothyronine Plus Thyroxine Administration in Preterm Infants Less Than 28 Weeks of Gestational Age: Hormonal and Clinical Effects
0031-3998/04/5502-0248 PEDIATRIC RESEARCH Vol. 55, No. 2, 2004 Copyright © 2004 International Pediatric Research Foundation, Inc. Printed in U.S.A. A Randomized, Masked Study of Triiodothyronine Plus Thyroxine Administration in Preterm Infants Less Than 28 Weeks of Gestational Age: Hormonal and Clinical Effects PAOLO G. VALERIO, ALEID G. VAN WASSENAER, JAN J.M. DE VIJLDER, AND JOKE H. KOK Department of Neonatology [P.G.V., A.G.v.W., J.H.K.] and Laboratory of Pediatric Endocrinology [J.J.M.d.V.], Academic Medical Center, Emma Children’s Hospital, 1105 AZ Amsterdam, The Netherlands ABSTRACT A randomized, placebo-controlled, masked study was con- effect on cortisol levels. We did not find any effects of T3 or of ducted of the responses of thyroid parameters, cortisol, and the T4 administration on the cardiovascular system. A single injec- cardiovascular system to a single dose of triiodothyronine (T3) tion of T3 (0.5 g/kg) given 22–26 h after birth only leads to a 24 h after birth, followed by a daily dose of thyroxine (T4) during 2-d increase of T3 levels and does not have effects on the Ͻ 6 wk to infants 28 wk gestational age. Thirty-one infants were cardiovascular system. This study does not support the use of T3 assigned to three groups: 1) group A: T3 24 h after birth plus according to our regimen in preterm infants. (Pediatr Res 55: daily T4 during 6 wk; 2) group B: placebo T3 and T4 during 6 wk; 248–253, 2004) and 3) group C: placebo T3 and placebo T4.T4, free T4,T3, free T3, reverse T3, thyroid-stimulating hormone, and cortisol were measured in cord blood and on days 1, 3, 7, 14, 21, 42, and 56. -

Endocrine Abnormalities of the Horse Scott M. Austin, DVM, MS, DACVIM
Endocrine abnormalities of the horse Scott M. Austin, DVM, MS, DACVIM Clinical Associate Professor of Equine Medicine Department of Veterinary Clinical Medicine University of Illinois Summary: Endocrine abnormalities occur frequently in the horse. The clinical presentation of common conditions may have significant overlap resulting in diagnostic confusion. It is important to arrive at an accurate diagnosis, as the successful therapy for endocrine abnormalities is contingent upon the correct diagnosis. Hypothyroidism: Much of the confusion around hypothyroidism is a result of the erroneous association of this condition with obesity, laminitis and infertility. Research that is more recent indicates that hypothyroidism is actually quite rare. In the limited case reports of documented hypothyroidism in horses, the primary clinical signs are lethargy, exercise intolerance, and poor quality haircoat. In horses that had thyroids removed, neither weight gain nor laminitis were seen. Diagnosis: The hypothalamus regulates the production of thyroid hormones through the actions of thyrotropin-releasing hormone (TRH), which stimulates the anterior pituitary gland to release thyroid- stimulating hormone (TSH). TSH then regulates the synthesis and release of thyroid hormones by the thyroid gland. In response to TSH stimulus, triiodothyronine (T3) and thyroxin (T4) are released from the thyroid gland into the bloodstream bound to either thyroglobulins or other proteins such as albumin. T4 has minimal activity and is essentially a prohormone. T3 is the primary active form of the hormone, and only unbound T3 can enter a cell and activate the vital functions attributable to this hormone. The common measurement of total T3 and T4 often provides erroneous values and does not provide a clear picture of thyroid function. -

Vitamin D Status and Its Relationship with Thyroid Function Parameters in Patients with Hypothyroidism
Medical Laboratory Journal, Sep-Oct, 2019; Vol 13: No 5 Original Article Vitamin D Status and its Relationship with Thyroid Function Parameters in Patients with Hypothyroidism Mojtaba Zare Ebrahimabad (MSc) ABSTRACT Department of Biochemistry and Background and Objectives: Vitamin D is an essential secosteroid that plays a Biophysics, Metabolic Disorders Research Center, Faculty of Medicine, crucial role in the homeostasis of a few mineral elements, particularly calcium. Since vitamin Golestan University of Medical D deficiency and thyroid diseases are two important global health problems, we aimed to Sciences, Gorgan, Iran investigate a possible relationship of vitamin D and calcium levels with hypothyroidism in an Hanieh Teymoori (MSc) Department of Biochemistry and Iranian population. Biophysics, Metabolic Disorders Methods: This case-control study was conducted on 175 subjects with Research Center, Faculty of Medicine, hypothyroidism (75 males and 100 females) and 175 euthyroid controls (85 males and 90 Golestan University of Medical Sciences, Gorgan, Iran females) who were referred to a laboratory in Gorgan, Iran. Serum levels of 25- Hamid Reza Joshaghani (PhD) hydroxyvitamin D, calcium, thyroid-stimulating hormone (TSH), free triiodothyronine (free Professor of Clinical Biochemistry, T3) and thyroxine (total T4) were measured in all participants. Laboratory Sciences Research Center (LSRC), Golestan University of Results: Vitamin D and calcium were significantly lower in patients with Medical Sciences, Gorgan, Iran hypothyroidism (P<0.0001). Free T3 and calcium levels differed significantly among Corresponding author: Hamid Reza hypothyroid patients based on their vitamin D status (P<0.0001), but vitamin D levels were Joshaghani Tel: +98-1732436108 within sufficient range in all groups. -

DHEA Sulfate, and Aging: Contribution of the Dheage Study to a Sociobiomedical Issue
Dehydroepiandrosterone (DHEA), DHEA sulfate, and aging: Contribution of the DHEAge Study to a sociobiomedical issue Etienne-Emile Baulieua,b, Guy Thomasc, Sylvie Legraind, Najiba Lahloue, Marc Rogere, Brigitte Debuiref, Veronique Faucounaug, Laurence Girardh, Marie-Pierre Hervyi, Florence Latourj, Marie-Ce´ line Leaudk, Amina Mokranel, He´ le` ne Pitti-Ferrandim, Christophe Trivallef, Olivier de Lacharrie` ren, Stephanie Nouveaun, Brigitte Rakoto-Arisono, Jean-Claude Souberbiellep, Jocelyne Raisonq, Yves Le Boucr, Agathe Raynaudr, Xavier Girerdq, and Franc¸oise Foretteg,j aInstitut National de la Sante´et de la Recherche Me´dicale Unit 488 and Colle`ge de France, 94276 Le Kremlin-Biceˆtre, France; cInstitut National de la Sante´et de la Recherche Me´dicale Unit 444, Hoˆpital Saint-Antoine, 75012 Paris, France; dHoˆpital Bichat, 75877 Paris, France; eHoˆpital Saint-Vincent de Paul, 75014 Paris, France; fHoˆpital Paul Brousse, 94804 Villejuif, France; gFondation Nationale de Ge´rontologie, 75016 Paris, France; hHoˆpital Charles Foix, 94205 Ivry, France; iHoˆpital de Biceˆtre, 94275 Biceˆtre, France; jHoˆpital Broca, 75013 Paris, France; kCentre Jack-Senet, 75015 Paris, France; lHoˆpital Sainte-Perine, 75016 Paris, France; mObservatoire de l’Age, 75017 Paris, France; nL’Ore´al, 92583 Clichy, France; oInstitut de Sexologie, 75116 Paris, France; pHoˆpital Necker, 75015 Paris, France; qHoˆpital Broussais, 75014 Paris, France; and rHoˆpital Trousseau, 75012 Paris, France Contributed by Etienne-Emile Baulieu, December 23, 1999 The secretion and the blood levels of the adrenal steroid dehydro- number of consumers. Extravagant publicity based on fantasy epiandrosterone (DHEA) and its sulfate ester (DHEAS) decrease pro- (‘‘fountain of youth,’’ ‘‘miracle pill’’) or pseudoscientific asser- foundly with age, and the question is posed whether administration tion (‘‘mother hormone,’’ ‘‘antidote for aging’’) has led to of the steroid to compensate for the decline counteracts defects unfounded radical assertions, from superactivity (‘‘keep young,’’ associated with aging. -
In Vitro Effect of Triiodothyronine on the Cyclic Amp, Progesterone and Testosterone Level in Porcine Theca, Granulosa and Luteal Cells
ENDOCRINE REGULATIONS, Vol. 32, 93 – 98, 1998 93 IN VITRO EFFECT OF TRIIODOTHYRONINE ON THE CYCLIC AMP, PROGESTERONE AND TESTOSTERONE LEVEL IN PORCINE THECA, GRANULOSA AND LUTEAL CELLS E.L. GREGORASZCZUK, J. GALAS Laboratory of Animal Endocrinology and Tissue Culture, Department of Animal Physiology, Institute of Zoology, Jagiellonian University, Krakow, Poland Objective. To investigate the influence of thyroid hormone on steroid production and cAMP accumulation in porcine theca (Tc) and granulosa cells (Gc) isolated from preovulatory follicles as well as in luteal cells isolated during the mid-developing luteal phase. Methods. Granulosa and theca cells separated from pig ovarian follicles and pieces of corpora lutea were cultured in the incubation medium M199 with 5 % calf serum. After the addition of triiodothyronine (T3) and 3-isobutyl-1-methyl xanthine (IBMX) to the culture medium cAMP, progesterone and testosterone were estimated with the aid of specific RIA. Results. T 3 added to the culture media stimulated the steroid secretion and cAMP accumulation in all cell types investigated. In theca cells, T3 alone increased androgen production by 2 fold and the addition of IBMX further augmented the steroidogenesis by 2.2 fold. In granulosa cell culture, IBMX had no effect either on the basal or T3 stimulated progesterone secretion and cAMP accumu- lation. In luteal cell culture, IBMX added alone increased progesterone secretion and cAMP accu- mulation in the same manner as T3. Further augmentation of progesterone secretion (1.3-fold) and cAMP accumulation (1.1-fold) was observed after the addition of IBMX together with T3. Conclusion. The influence of thyroid hormone on cyclic nucleotide release by ovarian cells may suggest the involvement of cAMP-dependent mechanism in the realization of T3 action in ovarian cells. -

The Relationship Between Vitamin D Deficiency and Thyroid Function in the First Trimester of Pregnancy
Original Article The relationship between Vitamin D deficiency and thyroid function in the first trimester of pregnancy Farahnaz Rostami 1, Lida Moghaddam-Benaem2, Navid Ghasemi 3, Sedighe Hantoushzadeh 4* 1Department of Midwifery & Reproductive Health, Faculty of Medical Sciences, Tarbiat Modares University, Al-e-Ahmad Highway, Tehran, Iran. 2 Department of Reproductive Health & Midwifery, Faculty of Medical Sciences, Tarbiat Modares University, Tehran, Iran. 3 Department of medicine, faculty of Medical Sciences Tehran, Islamic Azad University, Tehran, Iran.4 Maternal, fetal & Neonatal Research Center, Tehran University of Medical Sciences, Tehran, Iran. Abstract Aims and Objective: There are few studies about the relationship between vitamin D deficiency and thyroid hormone levels in pregnancy. This study aimed to assess the relation serum vitamin D levels with thyroid hormones in the first trimester of pregnancy in Iran. Methods: In this case-control research 430 pregnant women (215 mothers with vitamin D deficiency, and 215 without this deficiency) attending prenatal clinics in Tehran, Iran were studied. 25 hydroxy vitamin D levels and thyroid function tests [free tetraiodothyronine (FT4), thyroid stimulating hormone (TSH), and free triiodothyronine (FT3)] were measured in all mothers. Data were analyzed using SPSS version 22 software. Kolmogorov-Smirnov test was used for normality testing of continuous variables; Student T-Test, and Mann-Whitney U test were used to compare the continuous parametric and nonparametric variables respectively in the 2 study groups; Linear regression model was used to assess the effect of potentially effective variables besides vitamin D on thyroid function tests. Results: In Mann-Whitney U test performed, T4 levels (mean± SD) were significantly higher in vitamin D deficiency group compared with the control group (20.8 ±32.5 vs.14.4 ± 24.1 ng/dl, P-value: 0.04), but there were no significant differences between the 2 study groups regarding TSH, and free T3 levels. -

Assessment the Levels of 25(OH) Vitamin D and Ferritin in Patients with Hypothyroid
European Journal of Molecular & Clinical Medicine ISSN 2515-8260 Volume 07, Issue 08, 2020 Assessment The Levels Of 25(OH) Vitamin D And Ferritin In Patients With Hypothyroid Amera Kamal Mohammed1, Thanaa Abdulmahdi2, Zainab Nasser Nabat3 1Department of Clinical Laboratory Sciences., College of Pharmacy, University of Kirkuk, 52001, Kirkuk, Iraq .ORCID ID: 0000-0002-8984-6824 , 2Babylon Technical Institute, Al-Furat Al-Awsat Technical University, 51015, Babylon, Iraq. ORCID ID: 0000-0002-9661-8280, 3Babylon Technical Institute, Al-Furat Al-Awsat Technical University, 51015, Babylon, Iraq. [email protected]. [email protected]. Abstract :Background: Thyroid hormones are essential and have various effects. For instance, they maintain normal growth and regulate metabolism. Hypothyroidism is a condition where the body doesn’t make enough thyroid hormones and people with hypothyroidism usually have a slower metabolism. The serum ferritin levels and vitamin D levels have been changed in patients with Hypothyroidism. Objective: a study has been carried out to investigate the association among thyroid disorder and the levels of both vitamin D and ferritin. Materials and Method: The BMI was calculated using the formula BMI= weight (kg)/ height2 (m)2. Vitamin D (25-hydroxyvitamin D), ferritin, T3, T4 and TSH levels were measured using the ELFA (Enzyme Linked Fluorescent Assay, Model: bioMérieux). the results were analysed using SPSS package (version 18). Results: The results indicated that the age of participants played an ignorable role in this investigation, while significant increases (P<0.05) differences were noticed between the patients and controls in terms of BMI, 25(OH) vit D, ferritin, TSH, T3 and T4. -

For Oral Administration
CONTRAINDICATIONS Adults Levothyroxine is contraindicated in patients with untreated subclinical (suppressed serum In adult patients with primary (thyroidal) hypothyroidism, serum TSH levels (using a sensitive TSH level with normal T3 and T4 levels) or overt thyrotoxicosis of any etiology and in patients assay) alone may be used to monitor therapy. The frequency of TSH monitoring during with acute myocardial infarction. Levothyroxine is contraindicated in patients with levothyroxine dose titration depends on the clinical situation but it is generally recommended uncorrected adrenal insufficiency since thyroid hormones may precipitate an acute adrenal at 6–8 week intervals until normalization. For patients who have recently initiated crisis by increasing the metabolic clearance of glucocorticoids (see PRECAUTIONS). levothyroxine therapy and whose serum TSH has normalized or in patients who have had their FOR ORAL ADMINISTRATION LEVOXYL® is contraindicated in patients with hypersensitivity to any of the inactive dosage or brand of levothyroxine changed, the serum TSH concentration should be measured ingredients in LEVOXYL® tablets (see DESCRIPTION, Inactive Ingredients). after 8–12 weeks. When the optimum replacement dose has been attained, clinical (physical Inactive Ingredients examination) and biochemical monitoring may be performed every 6–12 months, depending Microcrystalline cellulose, croscarmellose sodium and magnesium stearate. The following WARNINGS on the clinical situation, and whenever there is a change in the patient’s status. It is are the coloring additives per tablet strength: WARNING: Thyroid hormones, including LEVOXYL®, either alone or with other recommended that a physical examination and a serum TSH measurement be performed at least annually in patients receiving LEVOXYL® (see WARNINGS, PRECAUTIONS, and DOSAGE I I therapeutic agents, should not be used for the treatment of obesity or for weight loss.