Suppression of Non-Homologous End Joining Does Not Rescue DNA Repair Defects
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Plugged Into the Ku-DNA Hub: the NHEJ Network Philippe Frit, Virginie Ropars, Mauro Modesti, Jean-Baptiste Charbonnier, Patrick Calsou
Plugged into the Ku-DNA hub: The NHEJ network Philippe Frit, Virginie Ropars, Mauro Modesti, Jean-Baptiste Charbonnier, Patrick Calsou To cite this version: Philippe Frit, Virginie Ropars, Mauro Modesti, Jean-Baptiste Charbonnier, Patrick Calsou. Plugged into the Ku-DNA hub: The NHEJ network. Progress in Biophysics and Molecular Biology, Elsevier, 2019, 147, pp.62-76. 10.1016/j.pbiomolbio.2019.03.001. hal-02144114 HAL Id: hal-02144114 https://hal.archives-ouvertes.fr/hal-02144114 Submitted on 29 May 2019 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Progress in Biophysics and Molecular Biology xxx (xxxx) xxx Contents lists available at ScienceDirect Progress in Biophysics and Molecular Biology journal homepage: www.elsevier.com/locate/pbiomolbio Plugged into the Ku-DNA hub: The NHEJ network * Philippe Frit a, b, Virginie Ropars c, Mauro Modesti d, e, Jean Baptiste Charbonnier c, , ** Patrick Calsou a, b, a Institut de Pharmacologie et Biologie Structurale, IPBS, Universite de Toulouse, CNRS, UPS, Toulouse, France b Equipe Labellisee Ligue Contre -

DNA Ligase IV Syndrome; a Review Thomas Altmann1 and Andrew R
Altmann and Gennery Orphanet Journal of Rare Diseases (2016) 11:137 DOI 10.1186/s13023-016-0520-1 REVIEW Open Access DNA ligase IV syndrome; a review Thomas Altmann1 and Andrew R. Gennery1,2* Abstract DNA ligase IV deficiency is a rare primary immunodeficiency, LIG4 syndrome, often associated with other systemic features. DNA ligase IV is part of the non-homologous end joining mechanism, required to repair DNA double stranded breaks. Ubiquitously expressed, it is required to prevent mutagenesis and apoptosis, which can result from DNA double strand breakage caused by intracellular events such as DNA replication and meiosis or extracellular events including damage by reactive oxygen species and ionising radiation. Within developing lymphocytes, DNA ligase IV is required to repair programmed DNA double stranded breaks induced during lymphocyte receptor development. Patients with hypomorphic mutations in LIG4 present with a range of phenotypes, from normal to severe combined immunodeficiency. All, however, manifest sensitivity to ionising radiation. Commonly associated features include primordial growth failure with severe microcephaly and a spectrum of learning difficulties, marrow hypoplasia and a predisposition to lymphoid malignancy. Diagnostic investigations include immunophenotyping, and testing for radiosensitivity. Some patients present with microcephaly as a predominant feature, but seemingly normal immunity. Treatment is mainly supportive, although haematopoietic stem cell transplantation has been used in a few cases. Keywords: DNA Ligase 4, Severe combined immunodeficiency, Primordial dwarfism, Radiosensitive, Lymphoid malignancy Background factors include intracellular events such as DNA replica- DNA ligase IV deficiency (OMIM 606593) or LIG4 syn- tion and meiosis, and extracellular events including drome (ORPHA99812), also known as Ligase 4 syn- damage by reactive oxygen species and ionising radi- drome, is a rare autosomal recessive disorder ation. -

Cr2007108.Pdf
npg Michael R Lieber et al. Cell Research (2008) 18:125-133. npg125 © 2008 IBCB, SIBS, CAS All rights reserved 1001-0602/08 $ 30.00 REVIEW www.nature.com/cr Flexibility in the order of action and in the enzymology of the nuclease, polymerases, and ligase of vertebrate non- homologous DNA end joining: relevance to cancer, aging, and the immune system Michael R Lieber1, Haihui Lu1, Jiafeng Gu1, Klaus Schwarz2 1USC Norris Comprehensive Cancer Center, University of Southern California Keck School of Medicine, Rm 5428, Los Angeles, CA 90089-9176, USA; 2Institute for Clinical Transfusion Medicine & Immunogenetics, Institute for Transfusion Medicine, Univer- sity Hospital, Ulm, Germany Nonhomologous DNA end joining (NHEJ) is the primary pathway for repair of double-strand DNA breaks in hu- man cells and in multicellular eukaryotes. The causes of double-strand breaks often fragment the DNA at the site of damage, resulting in the loss of information there. NHEJ does not restore the lost information and may resect ad- ditional nucleotides during the repair process. The ability to repair a wide range of overhang and damage configura- tions reflects the flexibility of the nuclease, polymerases, and ligase of NHEJ. The flexibility of the individual com- ponents also explains the large number of ways in which NHEJ can repair any given pair of DNA ends. The loss of information locally at sites of NHEJ repair may contribute to cancer and aging, but the action by NHEJ ensures that entire segments of chromosomes are not lost. Keywords: nonhomologous DNA end joining (NHEJ), Ku, DNA-PKcs, Artemis, Cernunnos/XLF, ligase IV, XRCC4, poly- merase µ, polymerase λ Cell Research (2008) 18:125-133. -

Mouse Lig4 Conditional Knockout Project (CRISPR/Cas9)
https://www.alphaknockout.com Mouse Lig4 Conditional Knockout Project (CRISPR/Cas9) Objective: To create a Lig4 conditional knockout Mouse model (C57BL/6J) by CRISPR/Cas-mediated genome engineering. Strategy summary: The Lig4 gene (NCBI Reference Sequence: NM_176953 ; Ensembl: ENSMUSG00000049717 ) is located on Mouse chromosome 8. 2 exons are identified, with the ATG start codon in exon 2 and the TAG stop codon in exon 2 (Transcript: ENSMUST00000095476). Exon 2 will be selected as conditional knockout region (cKO region). Deletion of this region should result in the loss of function of the Mouse Lig4 gene. To engineer the targeting vector, homologous arms and cKO region will be generated by PCR using BAC clone RP23-191P3 as template. Cas9, gRNA and targeting vector will be co-injected into fertilized eggs for cKO Mouse production. The pups will be genotyped by PCR followed by sequencing analysis. Note: Null homozygotes die late in gestation with extensive CNS apoptosis, blocked lymphopoeiesis and failure of V(D)J joining. Carrier fibroblasts show elevated chromosome breaks. ~40% of homozygous hypomorphs survive, with retarded growth, reduced PBL and progressive loss of hematopoietic stem cells. Exon 2 covers 100.0% of the coding region. Start codon is in exon 2, and stop codon is in exon 2. The size of intron 1 for 5'-loxP site insertion: 2223 bp. The size of effective cKO region: ~3006 bp. The cKO region does not have any other known gene. Page 1 of 7 https://www.alphaknockout.com Overview of the Targeting Strategy gRNA region Wildtype allele T A 5' gRNA region G 3' 1 2 Targeting vector T A G Targeted allele T A G Constitutive KO allele (After Cre recombination) Legends Exon of mouse Lig4 Homology arm cKO region loxP site Page 2 of 7 https://www.alphaknockout.com Overview of the Dot Plot Window size: 10 bp Forward Reverse Complement Sequence 12 Note: The sequence of homologous arms and cKO region is aligned with itself to determine if there are tandem repeats. -

(XRCC1) Deficiency Enhances Class Switch Recombination and Is
X-ray repair cross-complementing protein 1 (XRCC1) deficiency enhances class switch recombination and is permissive for alternative end joining Li Han1, Weifeng Mao1,2, and Kefei Yu3 Department of Microbiology and Molecular Genetics, Michigan State University, East Lansing, MI 48824 Edited* by Frederick W. Alt, Howard Hughes Medical Institute, Harvard Medical School, Children’s Hospital, Immune Disease Institute, Boston, MA, and approved February 10, 2012 (received for review December 15, 2011) DNA double-strand breaks (DSBs) are essential intermediates in Ig the DNA end, the DNA-dependent protein kinase (DNA-PKcs) gene rearrangements: V(D)J and class switch recombination (CSR). that regulates end joining by phosphorylating other proteins (in- In contrast to V(D)J recombination, which is almost exclusively de- cluding itself), and the ligase complex containing XLF, XRCC4, pendent on nonhomologous end joining (NHEJ), CSR can occur in and DNA ligase 4. Also involved is a growing list of auxiliary NHEJ-deficient cells via a poorly understand backup pathway (or factors, including end processing nucleases (e.g., Artemis) and pathways) often termed alternative end joining (A-EJ). Recently, polymerases (μ and λ), polynucleotide kinases, 53BP1, and many several components of the single-strand DNA break (SSB) repair DNA damage response proteins (ATM, H2AX, Chk1, etc.). machinery, including XRCC1, have been implicated in A-EJ. To de- Although both V(D)J and class switch recombination rely on termine its role in A-EJ and CSR, Xrcc1 was deleted by targeted the generation and repair of DSBs, the dependence on NHEJ mutation in the CSR proficient mouse B-cell line, CH12F3. -

Polymerase Δ Promotes Chromosomal Rearrangements and Imprecise Double-Strand Break Repair
Polymerase δ promotes chromosomal rearrangements and imprecise double-strand break repair Jacob V. Layera, Lydie Debaizea, Alexandria Van Scoyka, Nealia C. Houseb, Alexander J. Brownc, Yunpeng Liud, Kristen E. Stevensone, Michael Hemannd, Steven A. Robertsc, Brendan D. Priceb, David M. Weinstocka,f,g,1, and Tovah A. Dayh,1 aDepartment of Medical Oncology, Dana-Farber Cancer Institute, Boston, MA 02215; bDepartment of Radiation Oncology, Dana-Farber Cancer Institute, Boston, MA 02215; cSchool of Molecular Biosciences, Washington State University, Pullman, WA 99164; dThe Koch Institute for Integrative Cancer Research at MIT, Massachusetts Institute of Technology, Cambridge, MA 02139; eDepartment of Biostatistics and Computational Biology, Dana-Farber Cancer Institute, Boston, MA 02215; fCancer Biology Program, Broad Institute of MIT and Harvard University, Cambridge, MA 02142; gBiological and Biomedical Sciences Program, Harvard Medical School, Boston, MA 02215; and hDepartment of Biology, Northeastern University, Boston, MA 02115 Edited by James E. Haber, Brandeis University, Waltham, MA, and approved September 9, 2020 (received for review July 10, 2020) Recent studies have implicated DNA polymerases θ (Pol θ) and β and λ, can also be recruited for end-resection and gap-filling (9, (Pol β) as mediators of alternative nonhomologous end-joining 10). The XRCC4/LIGIV complex is recruited and ligates both (Alt-NHEJ) events, including chromosomal translocations. Here strands (11). we identify subunits of the replicative DNA polymerase δ (Pol δ) The third type of repair, alternative NHEJ (Alt-NHEJ), is as promoters of Alt-NHEJ that results in more extensive intrachro- often described as a back-up end-joining process, as it resolves a mosomal mutations at a single double-strand break (DSB) and greater fraction of DSBs when C-NHEJ is compromised (12). -
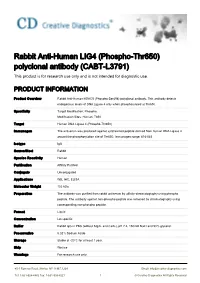
Rabbit Anti-Human LIG4 (Phospho-Thr650) Polyclonal Antibody (CABT-L3791) This Product Is for Research Use Only and Is Not Intended for Diagnostic Use
Rabbit Anti-Human LIG4 (Phospho-Thr650) polyclonal antibody (CABT-L3791) This product is for research use only and is not intended for diagnostic use. PRODUCT INFORMATION Product Overview Rabbit Anti-Human HDAC5 (Phospho-Ser498) polyclonal antibody. This antibody detects endogenous levels of DNA Ligase 4 only when phosphorylated at Thr650. Specificity Target Modification: Phospho. Modification Sites: Human: T650 Target Human DNA Ligase 4 (Phospho-Thr650) Immunogen The antiserum was produced against synthesized peptide derived from human DNA Ligase 4 around the phosphorylation site of Thr650. Immunogen range: 616-665 Isotype IgG Source/Host Rabbit Species Reactivity Human Purification Affinity Purified Conjugate Unconjugated Applications WB, IHC, ELISA Molecular Weight 103 kDa Preparation The antibody was purified from rabbit antiserum by affinity-chromatography using phospho peptide. The antibody against non-phospho peptide was removed by chromatography using corresponding non-phospho peptide. Format Liquid Concentration Lot specific Buffer Rabbit IgG in PBS (without Mg2+ and Ca2+), pH 7.4, 150mM NaCl and 50% glycerol. Preservative 0.02% Sodium Azide Storage Stable at -20°C for at least 1 year. Ship Wet ice Warnings For research use only. 45-1 Ramsey Road, Shirley, NY 11967, USA Email: [email protected] Tel: 1-631-624-4882 Fax: 1-631-938-8221 1 © Creative Diagnostics All Rights Reserved BACKGROUND Introduction The protein encoded by this gene is a DNA ligase that joins single-strand breaks in a double- stranded polydeoxynucleotide in an ATP-dependent reaction. This protein is essential for V(D)J recombination and DNA double-strand break (DSB) repair through nonhomologous end joining (NHEJ). -

Sister Chromatid, but Not NHEJ-Mediated Inter-Chromosomal Telomere
Downloaded from genome.cshlp.org on October 6, 2021 - Published by Cold Spring Harbor Laboratory Press Sister chromatid, but not NHEJ-mediated inter-chromosomal telomere fusions, occur independently of DNA ligases 3 and 4 Kate Liddiard,1 Brian Ruis,2 Taylor Takasugi,2 Adam Harvey,2 Kevin E. Ashelford, 1 Eric A. Hendrickson2¶ and Duncan M. Baird1¶ ¶ Joint senior authors 1Institute of Cancer and Genetics, School of Medicine, Cardiff University, Heath Park, Cardiff, CF14 4XN, United Kingdom. 2 Department of Biochemistry, Molecular Biology, and Biophysics, University of Minnesota Medical School, Minneapolis, MN 55455, USA. Corresponding author: Duncan Baird, Institute of Cancer and Genetics, School of Medicine, Cardiff University, Heath Park, Cardiff, CF14 4XN, UK. Email: [email protected] Running title: A- and C-NHEJ of dysfunctional human telomeres Keywords: Telomere, genome instability, DNA repair, inter-chromosomal, intra- chromosomal, non-homologous end-joining (NHEJ), DNA ligase, microhomology, crisis, double-stranded DNA break (DSB) 1 Downloaded from genome.cshlp.org on October 6, 2021 - Published by Cold Spring Harbor Laboratory Press Abstract Telomeres shorten with each cell division and can ultimately become substrates for non-homologous end-joining repair, leading to large-scale genomic rearrangements of the kind frequently observed in human cancers. We have characterised over 1400 telomere fusion events at the single-molecule level, using a combination of high- throughput sequence analysis together with experimentally-induced telomeric double-stranded DNA breaks. We show that a single chromosomal dysfunctional telomere can fuse with diverse non-telomeric genomic loci, even in the presence of an otherwise stable genome, and that fusion predominates in coding regions. -

Alternative Okazaki Fragment Ligation Pathway by DNA Ligase III
Genes 2015, 6, 385-398; doi:10.3390/genes6020385 OPEN ACCESS genes ISSN 2073-4425 www.mdpi.com/journal/genes Review Alternative Okazaki Fragment Ligation Pathway by DNA Ligase III Hiroshi Arakawa 1,* and George Iliakis 2 1 IFOM-FIRC Institute of Molecular Oncology Foundation, IFOM-IEO Campus, Via Adamello 16, Milano 20139, Italy 2 Institute of Medical Radiation Biology, University of Duisburg-Essen Medical School, Essen 45122, Germany; E-Mail: [email protected] * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +39-2-574303306; Fax: +39-2-574303231. Academic Editor: Peter Frank Received: 31 March 2015 / Accepted: 18 June 2015 / Published: 23 June 2015 Abstract: Higher eukaryotes have three types of DNA ligases: DNA ligase 1 (Lig1), DNA ligase 3 (Lig3) and DNA ligase 4 (Lig4). While Lig1 and Lig4 are present in all eukaryotes from yeast to human, Lig3 appears sporadically in evolution and is uniformly present only in vertebrates. In the classical, textbook view, Lig1 catalyzes Okazaki-fragment ligation at the DNA replication fork and the ligation steps of long-patch base-excision repair (BER), homologous recombination repair (HRR) and nucleotide excision repair (NER). Lig4 is responsible for DNA ligation at DNA double strand breaks (DSBs) by the classical, DNA-PKcs-dependent pathway of non-homologous end joining (C-NHEJ). Lig3 is implicated in a short-patch base excision repair (BER) pathway, in single strand break repair in the nucleus, and in all ligation requirements of the DNA metabolism in mitochondria. In this scenario, Lig1 and Lig4 feature as the major DNA ligases serving the most essential ligation needs of the cell, while Lig3 serves in the cell nucleus only minor repair roles. -

Cell Cycle- and DNA Repair Pathway-Specific Effects of Apoptosis on Tumor Suppression
Cell cycle- and DNA repair pathway-specific effects of apoptosis on tumor suppression Steven S. Fostera, Saurav Dea, Linda K. Johnsonb, John H. J. Petrinia,1, and Travis H. Strackera,c,1 aMolecular Biology Program, Sloan-Kettering Institute, New York, NY 10021; bCenter of Comparative Medicine and Pathology, Memorial Sloan-Kettering Cancer Center, New York, NY 10021; and cOncology Programme, Institute for Research in Biomedicine, 08028 Barcelona, Spain Edited by James E. Haber, Brandeis University, Waltham, MA, and approved May 8, 2012 (received for review January 12, 2012) The DNA damage response comprises DNA repair, cell-cycle check- required for subsequent activation of ATM, an apical kinase in point control, and DNA damage-induced apoptosis that collectively the DDR (2). ATM and related kinases are estimated to modify promote genomic integrity and suppress tumorigenesis. Previ- more than 700 substrates in response to DNA damage on con- ously, we have shown that the Chk2 kinase functions indepen- sensus SQ/TQ sites (6, 7). Among these substrates are key regu- dently of the Mre11 complex (Mre11, Rad50, and Nbs1) and ATM lators of cell-cycle checkpoints, DNA repair factors, and proteins in apoptosis and suppresses tumorigenesis resulting from hypo- that regulate apoptosis and senescence, accounting for the broad morphic alleles of Mre11 or Nbs1. Based on this work, we have physiological impact of DDR functions (8). proposed that Chk2 limits the oncogenic potential of replication- Arguably one of the most important ATM substrates is the associated DNA damage. Here we further address the role of Chk2 tumor suppressor p53. p53 controls the G1/S cell-cycle check- and damage-induced apoptosis in suppressing the oncogenic po- point and is required for both apoptosis and senescence in various cellular contexts (9). -

End-Joining Repair of Double-Strand Breaks in Drosophila Melanogaster Is Largely DNA Ligase IV Independent
Copyright 2004 by the Genetics Society of America DOI: 10.1534/genetics.104.033902 End-Joining Repair of Double-Strand Breaks in Drosophila melanogaster Is Largely DNA Ligase IV Independent Mitch McVey,*,†,1 Dora Radut* and Jeff J. Sekelsky*,‡ *Department of Biology, †SPIRE Program and ‡Program in Molecular Biology and Biotechnology, University of North Carolina, Chapel Hill, North Carolina 27599 Manuscript received July 23, 2004 Accepted for publication August 26, 2004 ABSTRACT Repair of DNA double-strand breaks can occur by either nonhomologous end joining or homologous recombination. Most nonhomologous end joining requires a specialized ligase, DNA ligase IV (Lig4). In Drosophila melanogaster, double-strand breaks created by excision of a P element are usually repaired by a homologous recombination pathway called synthesis-dependent strand annealing (SDSA). SDSA requires strand invasion mediated by DmRad51, the product of the spn-A gene. In spn-A mutants, repair proceeds through a nonconservative pathway involving the annealing of microhomologies found within the 17-nt overhangs produced by P excision. We report here that end joining of P-element breaks in the absence of DmRad51 does not require Drosophila LIG4. In wild-type flies, SDSA is sometimes incomplete, and repair is finished by an end-joining pathway that also appears to be independent of LIG4. Loss of LIG4 does not increase sensitivity to ionizing radiation in late-stage larvae, but lig4 spn-A double mutants do show heightened sensitivity relative to spn-A single mutants. Together, our results suggest that a LIG4- independent end-joining pathway is responsible for the majority of double-strand break repair in the absence of homologous recombination in flies. -
Two Hits in One: Whole Genome Sequencing Unveils LIG4 Syndrome
Fadda et al. BMC Medical Genetics (2016) 17:84 DOI 10.1186/s12881-016-0346-7 CASE REPORT Open Access Two hits in one: whole genome sequencing unveils LIG4 syndrome and urofacial syndrome in a case report of a child with complex phenotype Abeer Fadda1, Fiza Butt2, Sara Tomei3, Sara Deola3, Bernice Lo3, Amal Robay4, Alya Al-Shakaki4, Noor Al-Hajri4, Ronald Crystal5, Marios Kambouris6,7, Ena Wang3, Francesco M. Marincola3, Khalid A. Fakhro3,4 and Chiara Cugno3,8* Abstract Background: Ligase IV syndrome, a hereditary disease associated with compromised DNA damage response mechanisms, and Urofacial syndrome, caused by an impairment of neural cell signaling, are both rare genetic disorders, whose reports in literature are limited. We describe the first case combining both disorders in a specific phenotype. Case presentation: We report a case of a 7-year old girl presenting with a complex phenotype characterized by multiple congenital abnormalities and dysmorphic features, microcephaly, short stature, combined immunodeficiency and severe vesicoureteral reflux. Whole Genome Sequencing was performed and a novel ligase IV homozygous missense c.T1312C/p.Y438H mutation was detected, and is believed to be responsible for most of the clinical features of the child, except vesicoureteral reflux which has not been previously described for ligase IV deficiency. However, we observed a second rare damaging (nonsense) homozygous mutation (c.C2125T/p.R709X) in the leucine-rich repeats and immunoglobulin-like domains 2 gene that encodes a protein implicated in neural cell signaling and oncogenesis. Interestingly, this mutation has recently been reported as pathogenic and causing urofacial syndrome, typically displaying vesicoureteral reflux.