HIV-1 Genes Vpr and Nef Synergistically Damage Podocytes, Leading to Glomerulosclerosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ubiquitinated Proliferating Cell Nuclear Antigen Activates Translesion DNA Polymerases and REV1
Ubiquitinated proliferating cell nuclear antigen activates translesion DNA polymerases and REV1 Parie Garg and Peter M. Burgers* Department of Biochemistry and Molecular Biophysics, Washington University School of Medicine, 660 South Euclid, St. Louis, MO 63110 Edited by Jerard Hurwitz, Memorial Sloan–Kettering Cancer Center, New York, NY, and approved November 4, 2005 (received for review July 14, 2005) In response to DNA damage, the Rad6͞Rad18 ubiquitin-conjugat- and requiring additional activation by the Cdc7͞Dbf4 protein ing complex monoubiquitinates the replication clamp proliferating kinase that normally functions in cell cycle progression (5, 12). cell nuclear antigen (PCNA) at Lys-164. Although ubiquitination of It is this complex pathway that mainly contributes to DNA PCNA is recognized as an essential step in initiating postreplication damage induced mutagenesis in eukaryotic cells. Although repair, the mechanistic relevance of this modification has remained normally involved in lagging strand DNA replication, the high- elusive. Here, we describe a robust in vitro system that ubiquiti- fidelity Pol ␦ is also required for damage-induced mutagenesis. nates yeast PCNA specifically on Lys-164. Significantly, only those The functions of Pol and Rev1 appear to be uniquely confined PCNA clamps that are appropriately loaded around effector DNA to mutagenesis. Pol is an error-prone DNA polymerase that can by its loader, replication factor C, are ubiquitinated. This observa- bypass damage (13). Rev1 is a deoxycytidyl transferase that tion suggests that, in vitro, only PCNA present at stalled replication shows the highest catalytic activity opposite template guanines forks is ubiquitinated. Ubiquitinated PCNA displays the same and abasic sites (14, 15). Rev1 is primarily responsible for replicative functions as unmodified PCNA. -

Jimmunol.0901240.Full.Pdf
A Critical Role for REV1 in Regulating the Induction of C:G Transitions and A:T Mutations during Ig Gene Hypermutation This information is current as Keiji Masuda, Rika Ouchida, Yingqian Li, Xiang Gao, of September 24, 2021. Hiromi Mori and Ji-Yang Wang J Immunol published online 8 July 2009 http://www.jimmunol.org/content/early/2009/07/08/jimmuno l.0901240 Downloaded from Supplementary http://www.jimmunol.org/content/suppl/2009/07/07/jimmunol.090124 Material 0.DC1 http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication by guest on September 24, 2021 *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2009 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. Published July 8, 2009, doi:10.4049/jimmunol.0901240 The Journal of Immunology A Critical Role for REV1 in Regulating the Induction of C:G Transitions and A:T Mutations during Ig Gene Hypermutation Keiji Masuda,* Rika Ouchida,* Yingqian Li,†* Xiang Gao,† Hiromi Mori,* and Ji-Yang Wang1* REV1 is a deoxycytidyl transferase that catalyzes the incorporation of deoxycytidines opposite deoxyguanines and abasic sites. -

The Nef-Infectivity Enigma: Mechanisms of Enhanced Lentiviral Infection Jolien Vermeire§, Griet Vanbillemont§, Wojciech Witkowski and Bruno Verhasselt*
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by PubMed Central 474 Current HIV Research, 2011, 9, 474-489 The Nef-Infectivity Enigma: Mechanisms of Enhanced Lentiviral Infection Jolien Vermeire§, Griet Vanbillemont§, Wojciech Witkowski and Bruno Verhasselt* Department of Clinical Chemistry, Microbiology, and Immunology, Ghent University, Belgium Abstract: The Nef protein is an essential factor for lentiviral pathogenesis in humans and other simians. Despite a multitude of functions attributed to this protein, the exact role of Nef in disease progression remains unclear. One of its most intriguing functions is the ability of Nef to enhance the infectivity of viral particles. In this review we will discuss current insights in the mechanism of this well-known, yet poorly understood Nef effect. We will elaborate on effects of Nef, on both virion biogenesis and the early stage of the cellular infection, that might be involved in infectivity enhancement. In addition, we provide an overview of different HIV-1 Nef domains important for optimal infectivity and briefly discuss some possible sources of the frequent discrepancies in the field. Hereby we aim to contribute to a better understanding of this highly conserved and therapeutically attractive Nef function. Keywords: Nef, HIV, infectivity, viral replication, mutation analysis, envelope protein, cholesterol, proteasome. 1. INTRODUCTION 2. THE MULTIFACETED NEF PROTEIN Despite the globally declining number of new human As early as 1991, infections of rhesus monkeys with nef- immunodeficiency virus (HIV) infections [1] and the hopeful deleted simian immunodeficiency virus (SIV) revealed a observation that cure from HIV infection does not seem dramatic reduction of viral loads and disease progression in impossible [2], the HIV pandemic still remains a very absence of nef [6]. -

HIV-1 Rev Downregulates Tat Expression and Viral Replication Via Modulation of NAD(P)H:Quinine Oxidoreductase 1 (NQO1)
ARTICLE Received 25 Jul 2014 | Accepted 22 Apr 2015 | Published 10 Jun 2015 DOI: 10.1038/ncomms8244 HIV-1 Rev downregulates Tat expression and viral replication via modulation of NAD(P)H:quinine oxidoreductase 1 (NQO1) Sneh Lata1,*, Amjad Ali2,*, Vikas Sood1,2,w, Rameez Raja2 & Akhil C. Banerjea2 HIV-1 gene expression and replication largely depend on the regulatory proteins Tat and Rev, but it is unclear how the intracellular levels of these viral proteins are regulated after infection. Here we report that HIV-1 Rev causes specific degradation of cytoplasmic Tat, which results in inhibition of HIV-1 replication. The nuclear export signal (NES) region of Rev is crucial for this activity but is not involved in direct interactions with Tat. Rev reduces the levels of ubiquitinated forms of Tat, which have previously been reported to be important for its transcriptional properties. Tat is stabilized in the presence of NAD(P)H:quinine oxidoreductase 1 (NQO1), and potent degradation of Tat is induced by dicoumarol, an NQO1 inhibitor. Furthermore, Rev causes specific reduction in the levels of endogenous NQO1. Thus, we propose that Rev is able to induce degradation of Tat indirectly by downregulating NQO1 levels. Our findings have implications in HIV-1 gene expression and latency. 1 Department of Microbiology, University College of Medical Sciences and Guru Teg Bahadur Hospital, Delhi 110095, India. 2 Laboratory of Virology, National Institute of Immunology, New Delhi 110067, India. * These authors contributed equally to this work. w Present address: Translational Health Science and Technology Institute, Faridabad, Haryana 121004, India. Correspondence and requests for materials should be addressed to A.C.B. -

Opportunistic Intruders: How Viruses Orchestrate ER Functions to Infect Cells
REVIEWS Opportunistic intruders: how viruses orchestrate ER functions to infect cells Madhu Sudhan Ravindran*, Parikshit Bagchi*, Corey Nathaniel Cunningham and Billy Tsai Abstract | Viruses subvert the functions of their host cells to replicate and form new viral progeny. The endoplasmic reticulum (ER) has been identified as a central organelle that governs the intracellular interplay between viruses and hosts. In this Review, we analyse how viruses from vastly different families converge on this unique intracellular organelle during infection, co‑opting some of the endogenous functions of the ER to promote distinct steps of the viral life cycle from entry and replication to assembly and egress. The ER can act as the common denominator during infection for diverse virus families, thereby providing a shared principle that underlies the apparent complexity of relationships between viruses and host cells. As a plethora of information illuminating the molecular and cellular basis of virus–ER interactions has become available, these insights may lead to the development of crucial therapeutic agents. Morphogenesis Viruses have evolved sophisticated strategies to establish The ER is a membranous system consisting of the The process by which a virus infection. Some viruses bind to cellular receptors and outer nuclear envelope that is contiguous with an intri‑ particle changes its shape and initiate entry, whereas others hijack cellular factors that cate network of tubules and sheets1, which are shaped by structure. disassemble the virus particle to facilitate entry. After resident factors in the ER2–4. The morphology of the ER SEC61 translocation delivering the viral genetic material into the host cell and is highly dynamic and experiences constant structural channel the translation of the viral genes, the resulting proteins rearrangements, enabling the ER to carry out a myriad An endoplasmic reticulum either become part of a new virus particle (or particles) of functions5. -
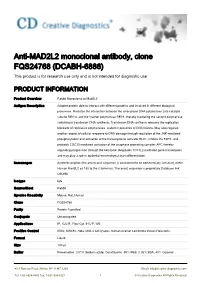
Anti-MAD2L2 Monoclonal Antibody, Clone FQS24768 (DCABH-6886) This Product Is for Research Use Only and Is Not Intended for Diagnostic Use
Anti-MAD2L2 monoclonal antibody, clone FQS24768 (DCABH-6886) This product is for research use only and is not intended for diagnostic use. PRODUCT INFORMATION Product Overview Rabbit Monoclonal to Mad2L2 Antigen Description Adapter protein able to interact with different proteins and involved in different biological processes. Mediates the interaction between the error-prone DNA polymerase zeta catalytic subunit REV3L and the inserter polymerase REV1, thereby mediating the second polymerase switching in translesion DNA synthesis. Translesion DNA synthesis releases the replication blockade of replicative polymerases, stalled in presence of DNA lesions. May also regulate another aspect of cellular response to DNA damage through regulation of the JNK-mediated phosphorylation and activation of the transcriptional activator ELK1. Inhibits the FZR1- and probably CDC20-mediated activation of the anaphase promoting complex APC thereby regulating progression through the cell cycle. Regulates TCF7L2-mediated gene transcription and may play a role in epithelial-mesenchymal transdifferentiation. Immunogen Synthetic peptide (the amino acid sequence is considered to be commercially sensitive) within Human Mad2L2 aa 150 to the C-terminus. The exact sequence is proprietary.Database link: Q9UI95 Isotype IgG Source/Host Rabbit Species Reactivity Mouse, Rat, Human Clone FQS24768 Purity Protein A purified Conjugate Unconjugated Applications IP, ICC/IF, Flow Cyt, IHC-P, WB Positive Control K562, SW480, Hela, Molt-4 cell lysates, human ovarian carcinoma tissue, Hela cells, Format Liquid Size 100 μl Buffer Preservative: 0.01% Sodium azide; Constituents: 59% PBS, 0.05% BSA, 40% Glycerol 45-1 Ramsey Road, Shirley, NY 11967, USA Email: [email protected] Tel: 1-631-624-4882 Fax: 1-631-938-8221 1 © Creative Diagnostics All Rights Reserved Preservative 0.01% Sodium Azide Storage Store at +4°C short term (1-2 weeks). -

DNA Polymerase Ι Compensates for Fanconi Anemia Pathway Deficiency by Countering DNA Replication Stress
DNA polymerase ι compensates for Fanconi anemia pathway deficiency by countering DNA replication stress Rui Wanga, Walter F. Lenoirb,c, Chao Wanga, Dan Sua, Megan McLaughlinb, Qianghua Hua, Xi Shena, Yanyan Tiana, Naeh Klages-Mundta,c, Erica Lynna, Richard D. Woodc,d, Junjie Chena,c, Traver Hartb,c, and Lei Lia,c,e,1 aDepartment of Experimental Radiation Oncology, The University of Texas MD Anderson Cancer Center, Houston, TX 77030; bDepartment of Bioinformatics and Computational Biology, The University of Texas MD Anderson Cancer Center, Houston, TX 77030; cThe University of Texas MD Anderson Cancer Center University of Texas Health Science Center at Houston Graduate School of Biomedical Sciences, Houston, TX 77030; dDepartment of Epigenetics and Molecular Carcinogenesis, The University of Texas MD Anderson Cancer Center, Houston, TX 77030; and eLife Sciences Institute, Zhejiang University, Hangzhou, China 310058 Edited by Wei Yang, NIH, Bethesda, MD, and approved November 12, 2020 (received for review May 8, 2020) Fanconi anemia (FA) is caused by defects in cellular responses to proteins, required in homologous recombination (FANCD1/ DNA crosslinking damage and replication stress. Given the con- BRCA2, FANCO/RAD51C, FANCJ/BARD1, and FANCR/ stant occurrence of endogenous DNA damage and replication fork RAD51) (22–26). stress, it is unclear why complete deletion of FA genes does not In addition to the direct role in crosslinking damage repair, have a major impact on cell proliferation and germ-line FA patients FA pathway components are linked to the protection of repli- are able to progress through development well into their adult- cation fork integrity during replication interruption that is not hood. -

Y-Family DNA Polymerases in Escherichia Coli
Y-family DNA polymerases in Escherichia coli The MIT Faculty has made this article openly available. Please share how this access benefits you. Your story matters. Citation Jarosz, Daniel F. et al. “Y-family DNA Polymerases in Escherichia Coli.” Trends in Microbiology 15.2 (2007): 70–77. Web. 13 Apr. 2012. © 2007 Elsevier Ltd. As Published http://dx.doi.org/10.1016/j.tim.2006.12.004 Publisher Elsevier Version Final published version Citable link http://hdl.handle.net/1721.1/70041 Terms of Use Article is made available in accordance with the publisher's policy and may be subject to US copyright law. Please refer to the publisher's site for terms of use. Review TRENDS in Microbiology Vol.15 No.2 Y-family DNA polymerases in Escherichia coli Daniel F. Jarosz1, Penny J. Beuning2,3, Susan E. Cohen2 and Graham C. Walker2 1 Department of Chemistry, Massachusetts Institute of Technology, Cambridge, MA 02139, USA 2 Department of Biology, Massachusetts Institute of Technology, Cambridge, MA 02139, USA 3 Department of Chemistry and Chemical Biology, Northeastern University, Boston, MA 02115, USA The observation that mutations in the Escherichia coli that is also lexA-independent [4]. This might have genes umuC+ and umuD+ abolish mutagenesis induced particularly important implications for bacteria living by UV light strongly supported the counterintuitive under conditions of nutrient starvation. The SOS response notion that such mutagenesis is an active rather than also seems to be oscillatory at the single-cell level, and this passive process. Genetic and biochemical studies have oscillation is dependent on the umuDC genes [5]. -

Ubiquitin and Ubiquitin-Like Proteins Are Essential Regulators of DNA Damage Bypass
cancers Review Ubiquitin and Ubiquitin-Like Proteins Are Essential Regulators of DNA Damage Bypass Nicole A. Wilkinson y, Katherine S. Mnuskin y, Nicholas W. Ashton * and Roger Woodgate * Laboratory of Genomic Integrity, National Institute of Child Health and Human Development, National Institutes of Health, 9800 Medical Center Drive, Rockville, MD 20850, USA; [email protected] (N.A.W.); [email protected] (K.S.M.) * Correspondence: [email protected] (N.W.A.); [email protected] (R.W.); Tel.: +1-301-435-1115 (N.W.A.); +1-301-435-0740 (R.W.) Co-first authors. y Received: 29 August 2020; Accepted: 29 September 2020; Published: 2 October 2020 Simple Summary: Ubiquitin and ubiquitin-like proteins are conjugated to many other proteins within the cell, to regulate their stability, localization, and activity. These modifications are essential for normal cellular function and the disruption of these processes contributes to numerous cancer types. In this review, we discuss how ubiquitin and ubiquitin-like proteins regulate the specialized replication pathways of DNA damage bypass, as well as how the disruption of these processes can contribute to cancer development. We also discuss how cancer cell survival relies on DNA damage bypass, and how targeting the regulation of these pathways by ubiquitin and ubiquitin-like proteins might be an effective strategy in anti-cancer therapies. Abstract: Many endogenous and exogenous factors can induce genomic instability in human cells, in the form of DNA damage and mutations, that predispose them to cancer development. Normal cells rely on DNA damage bypass pathways such as translesion synthesis (TLS) and template switching (TS) to replicate past lesions that might otherwise result in prolonged replication stress and lethal double-strand breaks (DSBs). -

A Novel Ebola Virus VP40 Matrix Protein-Based Screening for Identification of Novel Candidate Medical Countermeasures
viruses Communication A Novel Ebola Virus VP40 Matrix Protein-Based Screening for Identification of Novel Candidate Medical Countermeasures Ryan P. Bennett 1,† , Courtney L. Finch 2,† , Elena N. Postnikova 2 , Ryan A. Stewart 1, Yingyun Cai 2 , Shuiqing Yu 2 , Janie Liang 2, Julie Dyall 2 , Jason D. Salter 1 , Harold C. Smith 1,* and Jens H. Kuhn 2,* 1 OyaGen, Inc., 77 Ridgeland Road, Rochester, NY 14623, USA; [email protected] (R.P.B.); [email protected] (R.A.S.); [email protected] (J.D.S.) 2 NIH/NIAID/DCR/Integrated Research Facility at Fort Detrick (IRF-Frederick), Frederick, MD 21702, USA; courtney.fi[email protected] (C.L.F.); [email protected] (E.N.P.); [email protected] (Y.C.); [email protected] (S.Y.); [email protected] (J.L.); [email protected] (J.D.) * Correspondence: [email protected] (H.C.S.); [email protected] (J.H.K.); Tel.: +1-585-697-4351 (H.C.S.); +1-301-631-7245 (J.H.K.) † These authors contributed equally to this work. Abstract: Filoviruses, such as Ebola virus and Marburg virus, are of significant human health concern. From 2013 to 2016, Ebola virus caused 11,323 fatalities in Western Africa. Since 2018, two Ebola virus disease outbreaks in the Democratic Republic of the Congo resulted in 2354 fatalities. Although there is progress in medical countermeasure (MCM) development (in particular, vaccines and antibody- based therapeutics), the need for efficacious small-molecule therapeutics remains unmet. Here we describe a novel high-throughput screening assay to identify inhibitors of Ebola virus VP40 matrix protein association with viral particle assembly sites on the interior of the host cell plasma membrane. -

MAD2L2 Monoclonal ANTIBODY
For Research Use Only MAD2L2 Monoclonal ANTIBODY www.ptgcn.com Catalog Number:67100-1-Ig Basic Information Catalog Number: GenBank Accession Number: CloneNo.: 67100-1-Ig BC015244 2A4C2 Size: GeneID (NCBI): Recommended Dilutions: 1000 μg/ml 10459 WB 1:5000-1:20000 Source: Full Name: IHC 1:500-1:2000 Mouse MAD2 mitotic arrest deficient-like 2 (yeast) Isotype: Calculated MW: IgG2b 211aa,24 kDa Purification Method: Observed MW: Protein A purification 24 kDa Immunogen Catalog Number: AG28233 Applications Tested Applications: Positive Controls: IHC, WB, ELISA WB : HeLa cells; Species Specificity: IHC : human lymphoma tissue; Human, mouse, rat Note-IHC: suggested angen retrieval with TE buffer pH 9.0; (*) Alternavely, angen retrieval may be performed with citrate buffer pH 6.0 MAD family, together with BUB and Mps1,Cdc20k, play roles in the mitotic spindle checkpoint. MAD2L2 is one of the MAD family. It can mediate the second Background Information polymerase switching in translation DNA synthesis by mediating the interaction between the error-prone DNA polymerase zeta catalytic subunit REV3L and the inserter polymerase REV1. Through regulation of the JNK-mediate phosphorylation and activation of the transcriptional activator ELK1, MAD2L2 involves in cellular response to DNA damage. Also it has role in the progression of cell cycle and peithelial-mesenchymal transdifferentiation. Storage: Storage Store at -20ºC. Stable for one year after shipment. Storage Buffer: PBS with 0.1% sodium azide and 50% glycerol pH 7.3. Aliquoting is unnecessary for -20ºC storage For technical support and original validation data for this product please contact: This product is exclusively available under T: 4006900926 E: [email protected] W: ptgcn.com Proteintech Group brand and is not available to purchase from any other manufacturer. -

Lentivirus and Lentiviral Vectors Fact Sheet
Lentivirus and Lentiviral Vectors Family: Retroviridae Genus: Lentivirus Enveloped Size: ~ 80 - 120 nm in diameter Genome: Two copies of positive-sense ssRNA inside a conical capsid Risk Group: 2 Lentivirus Characteristics Lentivirus (lente-, latin for “slow”) is a group of retroviruses characterized for a long incubation period. They are classified into five serogroups according to the vertebrate hosts they infect: bovine, equine, feline, ovine/caprine and primate. Some examples of lentiviruses are Human (HIV), Simian (SIV) and Feline (FIV) Immunodeficiency Viruses. Lentiviruses can deliver large amounts of genetic information into the DNA of host cells and can integrate in both dividing and non- dividing cells. The viral genome is passed onto daughter cells during division, making it one of the most efficient gene delivery vectors. Most lentiviral vectors are based on the Human Immunodeficiency Virus (HIV), which will be used as a model of lentiviral vector in this fact sheet. Structure of the HIV Virus The structure of HIV is different from that of other retroviruses. HIV is roughly spherical with a diameter of ~120 nm. HIV is composed of two copies of positive ssRNA that code for nine genes enclosed by a conical capsid containing 2,000 copies of the p24 protein. The ssRNA is tightly bound to nucleocapsid proteins, p7, and enzymes needed for the development of the virion: reverse transcriptase (RT), proteases (PR), ribonuclease and integrase (IN). A matrix composed of p17 surrounds the capsid ensuring the integrity of the virion. This, in turn, is surrounded by an envelope composed of two layers of phospholipids taken from the membrane of a human cell when a newly formed virus particle buds from the cell.