Relative Bioavailability, Intranasal Abuse Potential, and Safety Of
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
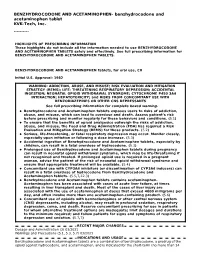
These Highlights Do Not Include All the Information Needed to Use BENZHYDROCODONE and ACETAMINOPHEN TABLETS Safely and Effectively
BENZHYDROCODONE AND ACETAMINOPHEN- benzhydrocodone and acetaminophen tablet KVK-Tech, Inc. ---------- HIGHLIGHTS OF PRESCRIBING INFORMATION These highlights do not include all the information needed to use BENZHYDROCODONE AND ACETAMINOPHEN TABLETS safely and effectively. See full prescribing information for BENZHYDROCODONE AND ACETAMINOPHEN TABLETS. BENZHYDROCODONE AND ACETAMINOPHEN tablets, for oral use, CII Initial U.S. Approval: 1982 WARNING: ADDICTION, ABUSE, AND MISUSE; RISK EVALUATION AND MITIGATION STRATEGY (REMS); LIFE- THREATENING RESPIRATORY DEPRESSION; ACCIDENTAL INGESTION; NEONATAL OPIOID WITHDRAWAL SYNDROME; CYTOCHROME P450 3A4 INTERACTION; HEPATOTOXICITY; and RISKS FROM CONCOMITANT USE WITH BENZODIAZEPINES OR OTHER CNS DEPRESSANTS See full prescribing information for complete boxed warning. Benzhydrocodone and Acetaminophen tablets exposes users to risks of addiction, abuse, and misuse, which can lead to overdose and death. Assess patient’s risk before prescribing and monitor regularly for these behaviors and conditions. (5.1) To ensure that the benefits of opioid analgesics outweigh the risks of addiction, abuse, and misuse, the Food and Drug Administration (FDA) has required a Risk Evaluation and Mitigation Strategy (REMS) for these products. (5.2) Serious, life-threatening, or fatal respiratory depression may occur. Monitor closely, especially upon initiation or following a dose increase. (5.3) Accidental ingestion of Benzhydrocodone and Acetaminophen tablets, especially by children, can result in a fatal overdose of hydrocodone. (5.3) Prolonged use of Benzhydrocodone and Acetaminophen tablets during pregnancy can result in neonatal opioid withdrawal syndrome, which may be life-threatening if not recognized and treated. If prolonged opioid use is required in a pregnant woman, advise the patient of the risk of neonatal opioid withdrawal syndrome and ensure that appropriate treatment will be available. -

Summary Analgesics Dec2019
Status as of December 31, 2019 UPDATE STATUS: N = New, A = Advanced, C = Changed, S = Same (No Change), D = Discontinued Update Emerging treatments for acute and chronic pain Development Status, Route, Contact information Status Agent Description / Mechanism of Opioid Function / Target Indication / Other Comments Sponsor / Originator Status Route URL Action (Y/No) 2019 UPDATES / CONTINUING PRODUCTS FROM 2018 Small molecule, inhibition of 1% diacerein TWi Biotechnology / caspase-1, block activation of 1 (AC-203 / caspase-1 inhibitor Inherited Epidermolysis Bullosa Castle Creek Phase 2 No Topical www.twibiotech.com NLRP3 inflamasomes; reduced CCP-020) Pharmaceuticals IL-1beta and IL-18 Small molecule; topical NSAID Frontier 2 AB001 NSAID formulation (nondisclosed active Chronic low back pain Phase 2 No Topical www.frontierbiotech.com/en/products/1.html Biotechnologies ingredient) Small molecule; oral uricosuric / anti-inflammatory agent + febuxostat (xanthine oxidase Gout in patients taking urate- Uricosuric + 3 AC-201 CR inhibitor); inhibition of NLRP3 lowering therapy; Gout; TWi Biotechnology Phase 2 No Oral www.twibiotech.com/rAndD_11 xanthine oxidase inflammasome assembly, reduced Epidermolysis Bullosa Simplex (EBS) production of caspase-1 and cytokine IL-1Beta www.arraybiopharma.com/our-science/our-pipeline AK-1830 Small molecule; tropomyosin Array BioPharma / 4 TrkA Pain, inflammation Phase 1 No Oral www.asahi- A (ARRY-954) receptor kinase A (TrkA) inhibitor Asahi Kasei Pharma kasei.co.jp/asahi/en/news/2016/e160401_2.html www.neurosmedical.com/clinical-research; -

Short-Acting Opioid Analgesics
Short-acting Opioid Analgesics Goals: Restrict use of short-acting opioid analgesics for acute conditions funded by the OHP. Promote use of preferred short-acting opioid analgesics. Length of Authorization: Initial: 7 to 30 days (except 12 months for end-of-life, sickle cell disease, severe burn injury, or cancer-related pain) Renewal: Up to 6 months Covered Alternatives: Current PMPDP preferred drug list per OAR 410-121-0030 at www.orpdl.org Searchable site for Oregon FFS Drug Class listed at www.orpdl.org/drugs/ Requires a PA: Non-preferred short-acting opioids and opioid combination products. All short-acting products prescribed for more than 14 days. Each prescription is limited to 7 days in treatment-naïve patients. Patients may fill up to 2 prescriptions every 90 days without prior authorization. All codeine and tramadol products for patients under 19 years of age Note: Patients on palliative care with a terminal diagnosis or with cancer-related pain or with pain associated with sickle cell disease or severe burn injury are exempt from this PA. Table 1. Daily Dose Threshold (90 morphine milligram equivalents per day (MME/day) of Oral Opioid Products. Opioid 90 MME/day Dose Notes Benzhydrocodone 73.5 mg Codeine 600 mg Codeine is not recommended for pediatric use; codeine is a prodrug of morphine and is subject to different rates of metabolism, placing certain populations at risk for overdose. Dihydrocodeine 360 mg Hydrocodone bitartrate 90 mg Hydromorphone 22.5 mg Levorphanol tartrate 8 mg Meperidine 900 mg Meperidine is not recommended for management of chronic pain due to potential accumulation of toxic metabolites. -
Abuse-Deterrent Formulation (ADF) Opioid Medications
Abuse-Deterrent Formulation (ADF) Opioid Medications Mark Garofoli, PharmD, MBA, BCGP, CPE Director, Experiential Learning Program WVU School of Pharmacy Clinical Pain Management Pharmacist, WVU Medicine Center for Integrative Pain Management Opioid Risk Screenings Opioid Naïve Opioid Experienced Self Reported Self Reported • Drug Abuse Screening Test (DAST) • Current Opioid Misuse Measure (COMM) • Screener & Opioid Assessment for Patients with Pain (SOAPP) • Pain Medication Questionnaire (PMQ) • Prescription Drug Use Questionnaire, Patient (PDUQp) Provider Reported • Opioid Risk Tool (ORT) Provider Reported • Diagnosis, Intractability, Risk, & Efficacy Score (DIRE) • Prescription Drug Use Questionnaire (PDUQ) www.opioidrisk.com Opioid Risk Tool (ORT) Opioid Risk Tool (ORT) Female Male Family History of SUD Alcohol 1 3 Illegal Drugs 2 3 Prescription Drugs 4 4 Personal History of SUD Alcohol 3 3 Illegal Drugs 4 4 Low Risk 0 - 3 Prescriptions Drugs 5 5 Moderate Risk 4 - 7 Age 16-45 1 1 High Risk >/= 8 History of Preadolescence Yes 3 0 Sexual Abuse Psychological Disease ADHD, OCD, Bipolar, Schizophrenia 2 2 Depression 1 1 Total Score Where are these opioids coming from… Friend/Relative (Theft) Drug Dealer Rx from >1 MD Clinician/Office (Theft) Friend/Relative Rx from 1 MD (Buy) Friend/Relative (Free) 2017 DEA National Drug Threat Assessment. https://www.dea.gov/docs/DIR-040-17_2017-NDTA.pdf Opioid Abuse Transition Hydrocodone Oxycodone Oxycodone Combo Combo IR Sole ER/IR Heroin Tablets Products Products ($10/Bag) $5-10/Tab $10-15/Tab $1.50/mg Shah A, et al. Characteristics of Initial Prescription Episodes and Likelihood of Long-Term Opioid Use – United States, 2006-2015. -

208653Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 208653Orig1s000 CLINICAL REVIEW(S) As noted by the biopharmaceutics reviewer, the in vitro dissolution method for the drug product “was derived directly from the USP monograph for Hydrocodone Bitartrate and Acetaminophen Tablets. The dissolution method of KP201 had been determined in buffers with different pH conditions. This method also showed that the dissolving conditions of acetaminophen matched those in the USP monograph. Therefore, the proposed dissolution method as Apparatus II (paddle), 0.1N HCl, 900 mL, 50 rpm, is acceptable for the drug product.” The in vitro dissolution method was adequately validated, and the mean and individual dissolution data were acceptable for the drug product. The CMC microbiology review found the drug product to be a low microbial risk solid oral tablet, (b) (4) and found the Applicant’s request for waiver of microbial limit testing (MLT) specifications for drug product release and stability specifications acceptable. The Applicant has committed to MLT and (b) (4) tests on these stability batches annually and to report additional stability data from these studies in post-approval Annual Reports to the NDA. The tablets are stored in HDPE bottles (b) (4) The facilities, the site responsible for drug product manufacture, packaging and labeling, and release and stability testing, is (b) (4) As noted in the CMC review (b) (4) : (b) (4) The response to the information request was adequate and the reviewer concluded that “based on the acceptable inspectional history of this facility, their experience with these unit operations, and the adequate IR responses received, (b) (4) is acceptable for NDA 208653.” Sufficient data were provided to support the quality and safety of the manufacture and release of the drug substance and drug product. -

FDA Briefing Document Joint Meeting of Anesthetic and Analgesic Drug
FDA Briefing Document Joint Meeting of Anesthetic and Analgesic Drug Products Advisory Committee and Drug Safety and Risk Management Advisory Committee May 5, 2016 1 of 158 DISCLAIMER STATEMENT The attached package contains background information prepared by the Food and Drug Administration (FDA) for the panel members of the advisory committee. The FDA background package often contains assessments and/or conclusions and recommendations written by individual FDA reviewers. Such conclusions and recommendations do not necessarily represent the final position of the individual reviewers, nor do they necessarily represent the final position of the Review Division or Office. We have brought results of studies evaluating the abuse of KP201 (benzhydrocodone/acetaminophen) tablets to this Advisory Committee in order to gain the Committee’s insights and opinions, and the background package may not include all issues relevant to the final regulatory recommendation and instead is intended to focus on issues identified by the Agency for discussion by the advisory committee. The FDA will not issue a final determination on the issues at hand until input from the advisory committee process has been considered and all reviews have been finalized. The final determination may be affected by issues not discussed at the advisory committee meeting. 2 of 158 FOOD AND DRUG ADMINISTRATION Center for Drug Evaluation and Research Joint Meeting of the Anesthetic and Life Support Drugs Advisory Committee and Drug Safety & Risk Management Advisory Committee May 5, 2016 Table of Contents- Open Session Background Materials Page 1. Division of Anesthesia, Analgesia, and Addiction Products (DAAAP) 4 Director Memorandum (Dr. Hertz) 2. Regulatory History of Abuse-Deterrent Opioids 7 3. -

Pharmacokinetics and Abuse Potential of Benzhydrocodone, a Novel Prodrug of Hydrocodone, After Intranasal Administration in Recr
38 Pharmacokinetics and Abuse Potential of Benzhydrocodone, a Novel Prodrug of Hydrocodone, Presented at the After Intranasal Administration in Recreational Drug Users International Conference on Opioids (ICOO) 1 1 2 2 3 3 June 5 –7, 2016 Travis Mickle, Sven Guenther, Kathryn Roupe Jing Zhou , Daniel Dickerson , Lynn Webster Boston, Massachusetts 1KemPharm, Coralville, IA; 2Worldwide Clinical Trials, Austin, TX; 3PRA Health Sciences, Lenexa, KS Background • The treatments were single, equimolar, Results Figure 1. Mean Hydrocodone Plasma Levels After The proportions of subjects with various levels of E max Ease of Insufflation score was significantly higher (i.e., IN doses. separated by a washout period of Study-Drug Dosing (PK Population, N= 24) reduction (expressed as percent reduction from their E max more difficult) for IN benzhydrocodone than for IN HB, approximately 72 hours. for HB) are displayed in Figure 3 . Approximately 69% of at a mean (SD) VAS rating of 78.7 (20.0) vs 65.6 (26.3). Immediate-release opioids are commonly abused Study Participants. 66 subjects were enrolled. 40 The difference between least-squares mean values was via alternative routes such as intranasal (IN) and —Benzhydrocodone HCl, 13.34 mg • Cohort 1: ( n= 33) excluded from all PK analyses due to subjects showed some degree of reduction, approximately intravenous administration. 1 Benzhy drocodone n 43% showed a 30% reduction, approximately 29% showed 12.7 points (95% confidence interval: 19.4, 5.9; P=0.0004). blood sample mishandling. o —Hydrocodone bitartrate, 15.0 mg i t (also known as KP201) is a hydrocodone prodrug a a 50% reduct≥ion. -
BMJ Open Is Committed to Open Peer Review. As Part of This Commitment We Make the Peer Review History of Every Article We Publish Publicly Available
BMJ Open: first published as 10.1136/bmjopen-2018-027935 on 5 May 2019. Downloaded from BMJ Open is committed to open peer review. As part of this commitment we make the peer review history of every article we publish publicly available. When an article is published we post the peer reviewers’ comments and the authors’ responses online. We also post the versions of the paper that were used during peer review. These are the versions that the peer review comments apply to. The versions of the paper that follow are the versions that were submitted during the peer review process. They are not the versions of record or the final published versions. They should not be cited or distributed as the published version of this manuscript. BMJ Open is an open access journal and the full, final, typeset and author-corrected version of record of the manuscript is available on our site with no access controls, subscription charges or pay-per-view fees (http://bmjopen.bmj.com). If you have any questions on BMJ Open’s open peer review process please email [email protected] http://bmjopen.bmj.com/ on September 26, 2021 by guest. Protected copyright. BMJ Open BMJ Open: first published as 10.1136/bmjopen-2018-027935 on 5 May 2019. Downloaded from Treatment of stable chronic obstructive pulmonary disease: a protocol for a systematic review and evidence map Journal: BMJ Open ManuscriptFor ID peerbmjopen-2018-027935 review only Article Type: Protocol Date Submitted by the 15-Nov-2018 Author: Complete List of Authors: Dobler, Claudia; Mayo Clinic, Evidence-Based Practice Center, Robert D. -

Lopinavir; Ritonavir (All Populations Monograph)
3/17/2020 Clinical Pharmacology powered by ClinicalKey Lopinavir; Ritonavir (All Populations Monograph) Indications/Dosage expand all | collapse all Labeled human immunodeficiency virus (HIV) infection Off-Label, Recommended coronavirus disease 2019 (COVID-19) † severe acute respiratory syndrome coronavirus 2 (SARS- human immunodeficiency virus (HIV) prophylaxis † CoV-2) infection † † Off-label indication NOTE: HIV guidelines recommend consideration be given to avoiding use of lopinavir; ritonavir-containing regimens in patients at high risk for cardiovascular adverse events.[46638] Initiation of therapy for HIV treatment: [46638] [23512] [42452] For adults, initiation of treatment immediately (or as soon as possible) after HIV diagnosis is recommended in all patients to reduce the risk of disease progression and to prevent the transmission of HIV, including perinatal transmission and transmission to sexual partners. Starting antiretroviral therapy early is particularly important for patients with AIDS-defining conditions, those with acute or recent HIV infection, and individuals who are pregnant; delaying therapy in these subpopulations has been associated with high risks of morbidity, mortality, and HIV transmission. Antiretroviral drug-resistance testing: Genotypic drug-resistance testing is recommended prior to initiation of therapy in all antiretroviral treatment- naive patients and prior to changing therapy for treatment failure. Phenotypic resistance testing may be used in conjunction with the genotypic test for patients with known or suspected complex drug-resistance mutation patterns. HIV-1 proviral DNA resistance testing is available for use in patients with HIV RNA concentrations below the limits of detection or with low-level viremia (i.e., less than 1,000 copies/mL), where genotypic testing is unlikely to be successful; however, the clinical utility of this assay has not been fully determined. -

A Abacavir Abacavirum Abakaviiri Abagovomab Abagovomabum
A abacavir abacavirum abakaviiri abagovomab abagovomabum abagovomabi abamectin abamectinum abamektiini abametapir abametapirum abametapiiri abanoquil abanoquilum abanokiili abaperidone abaperidonum abaperidoni abarelix abarelixum abareliksi abatacept abataceptum abatasepti abciximab abciximabum absiksimabi abecarnil abecarnilum abekarniili abediterol abediterolum abediteroli abetimus abetimusum abetimuusi abexinostat abexinostatum abeksinostaatti abicipar pegol abiciparum pegolum abisipaaripegoli abiraterone abirateronum abirateroni abitesartan abitesartanum abitesartaani ablukast ablukastum ablukasti abrilumab abrilumabum abrilumabi abrineurin abrineurinum abrineuriini abunidazol abunidazolum abunidatsoli acadesine acadesinum akadesiini acamprosate acamprosatum akamprosaatti acarbose acarbosum akarboosi acebrochol acebrocholum asebrokoli aceburic acid acidum aceburicum asebuurihappo acebutolol acebutololum asebutololi acecainide acecainidum asekainidi acecarbromal acecarbromalum asekarbromaali aceclidine aceclidinum aseklidiini aceclofenac aceclofenacum aseklofenaakki acedapsone acedapsonum asedapsoni acediasulfone sodium acediasulfonum natricum asediasulfoninatrium acefluranol acefluranolum asefluranoli acefurtiamine acefurtiaminum asefurtiamiini acefylline clofibrol acefyllinum clofibrolum asefylliiniklofibroli acefylline piperazine acefyllinum piperazinum asefylliinipiperatsiini aceglatone aceglatonum aseglatoni aceglutamide aceglutamidum aseglutamidi acemannan acemannanum asemannaani acemetacin acemetacinum asemetasiini aceneuramic -

Ibm Micromedex® Carenotes Titles by Category
IBM MICROMEDEX® CARENOTES TITLES BY CATEGORY DECEMBER 2019 © Copyright IBM Corporation 2019 All company and product names mentioned are used for identification purposes only and may be trademarks of their respective owners. Table of Contents IBM Micromedex® CareNotes Titles by Category Allergy and Immunology ..................................................................................................................2 Ambulatory.......................................................................................................................................3 Bioterrorism ...................................................................................................................................18 Cardiology......................................................................................................................................18 Critical Care ...................................................................................................................................20 Dental Health .................................................................................................................................22 Dermatology ..................................................................................................................................23 Dietetics .........................................................................................................................................24 Endocrinology & Metabolic Disease ..............................................................................................26 -

Apadaz (Benzhydrocodone and Acetaminophen)
HIGHLIGHTS OF PRESCRIBING INFORMATION • Initiate treatment with APADAZ at 1 or 2 tablets every 4 to 6 hours These highlights do not include all the information needed to use as needed for pain. Dosage should not exceed 12 tablets in a 24 APADAZ™ safely and effectively. See full prescribing information hour period. (2.2) for APADAZ. • 6.12 mg benzhydrocodone is equivalent to 4.54 mg hydrocodone or 7.5 mg hydrocodone bitartrate. If switching from immediate-release APADAZ (benzhydrocodone and acetaminophen) tablets, for oral hydrocodone bitartrate/acetaminophen, substitute 6.12 mg/325 mg use, CII APADAZ for 7.5 mg/325 mg hydrocodone bitartrate/acetaminophen. Initial U.S. Approval: 1982 Dosage of APADAZ should be adjusted according to the severity of the pain and the response of the patient. WARNING: ADDICTION, ABUSE, AND MISUSE; LIFE • Do not stop APADAZ abruptly in a physically-dependent patient. THREATENING RESPIRATORY DEPRESSION; ACCIDENTAL (2.5) INGESTION; NEONATAL OPIOID WITHDRAWAL SYNDROME; --------------------- DOSAGE FORMS AND STRENGTHS -------------------- HEPATOTOXICITY, CYTOCHROME P450 3A4 INTERACTION, and Immediate-release tablets: 6.12 mg benzhydrocodone (equivalent to RISKS FROM CONCOMITANT USE WITH BENZODIAZEPINES OR 6.67 mg benzhydrocodone hydrochloride) and 325 mg acetaminophen OTHER CNS DEPRESSANTS (3) See full prescribing information for complete boxed warning. ------------------------------- CONTRAINDICATIONS ------------------------------ • APADAZ exposes users to risks of addiction, abuse, and • Significant respiratory depression (4) misuse, which can lead to overdose and death. Assess patient’s • Acute or severe bronchial asthma in an unmonitored setting or in risk before prescribing and monitor regularly for these absence of resuscitative equipment (4) behaviors and conditions. (5.1) • Known or suspected gastrointestinal obstruction, including paralytic • Serious, life-threatening, or fatal respiratory depression may ileus (4) occur.