Therapeutic Options for Uncontrolled Asthma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Non-Controlled Bronchial Asthma: the Contemporary Condition of the Problem
1 UDC 616.248.1–085–084.001.5 Y.I. Feshchenko, I.F. Illyinskaya, L.V. Arefieva, L.M. Kuryk SO «National Institute Phthysiology and pulmonology named after F. G. Yanovsky NAMS of Ukraine» Non-controlled bronchial asthma: the contemporary condition of the problem Key words: bronchial asthma. Among all allergic diseases the most common is bron- of asthma [10, 13]. Different authors, when allocat- chial asthma (BA). In the world there are already about ing certain of its phenotypes and subtypes, rely on clini- 300 million patients with this ailment and in the forecast cal and morphological characteristics, the most significant by 2025 their number will increase by another 100 mil- triggers, the presence of concomitant pathology, as well lion. Chronization and deepening of the pathological pro- as unique responses to treatment. Thus, in the materials cess in asthma leads to a significant deterioration in the of GINA [10, 13, 20], there are those phenotypes of asthma quality of life of patients, decrease their activity, and also that can be easily identified. Distinguish: allergic asthma, causes growth disability and mortality from this illness. non-allergic asthma, childhood asthma / recurrent obstruc- According to official statistics in Ukraine, almost 500 pa- tive bronchitis, late-on asthma, asthma with obstruction tients with asthma suffer from 100 thousand adults, and this and a fixed rate of airflow, obesity asthma, occupational disease is diagnosed annually for about 8 thousand peo- asthma, asthma, severe asthma, and BA-COPD over- ple. According to experts, this does not correspond to the lapped syndrome. At the same time, the European respi- actual situation due to existing shortcomings in the diag- ratory community and the American Thoracic Community nosis of this pathology, but in fact the number of patients tend to focus more on a combination of clinical and patho- is much higher [15]. -

Simplifying Asthma Management in Primary Care EDUCATIONAL SERIES RECOMMENDATIONS from the 2020 NZ ASTHMA GUIDELINES
Simplifying asthma management A RESEARCH REVIEW™ in primary care EDUCATIONAL SERIES RECOMMENDATIONS FROM THE 2020 NZ ASTHMA GUIDELINES Making Education Easy 2021 About the expert This review is intended as an educational resource for primary healthcare professionals. It discusses the new Asthma and Respiratory Foundation NZ Adolescent and Adult Asthma Guidelines, published in the NZ Medical Professor Journal in June 2020, and how these may be implemented in primary care. The guidelines, which have Richard Beasley been developed by a multidisciplinary group of respiratory health experts, were last updated in 2016. Since CNZM, DSc(Otago), DM(Southampton), that time there have been significant advances in the understanding of how to best manage patients with MBChB, FRCP(London), FRACP, FAAAAI, FFOM(Hon), FAPSR(New Zealand), FERS, asthma. Taking into account the latest findings and incorporating recommendations from the Global Initiative FThorSoc, FRSNZ. for Asthma (GINA) Update strategy, the new guidelines provide simple, practical and evidenced-based recommendations for the diagnosis, assessment and management of asthma. Healthcare professionals may Richard Beasley is a physician at Wellington need to review the management of their asthma patients in light of the new guidelines. Regional Hospital, Director of the Medical Research Institute of New Zealand, and The 2020 Asthma and Respiratory Foundation NZ Adolescent and Adult Asthma Guidelines and a number of Professor of Medicine at Victoria University key clinical resources discussed in this review can be downloaded here. of Wellington. He is an Adjunct Professor at the University of Otago and Visiting Professor, University of Southampton, United Kingdom. Asthma: A major public health issue He is the Chair of the Asthma and Respiratory Foundation of New Zealand Adolescent and The prevalence of asthma in NZ is amongst the highest in the world, with up to 20% of children and adults affected Adult Asthma Guidelines. -
Global Strategy for Asthma Management and Prevention
® GLOBAL STRATEGY FOR ASTHMA MANAGEMENT AND PREVENTION REVISED 2006 Copyright © 2006 MCR VISION, Inc. All Rights Reserved Global Strategy for Asthma Management and Prevention The GINA reports are available on www.ginasthma.org. Global Strategy for Asthma Management and Prevention 2006 GINA EXECUTIVE COMMITTEE* Soren Erik Pedersen, MD Ladislav Chovan, MD, PhD Kolding Hospital President, Slovak Pneumological and Paul O'Byrne, MD, Chair Kolding, Denmark Phthisiological Society McMaster University Bratislava, Slovak Republic Hamilton, Ontario, Canada Emilio Pizzichini. MD Universidade Federal de Santa Catarina Motohiro Ebisawa, MD, PhD Eric D. Bateman, MD Florianópolis, SC, Brazil National Sagamihara Hospital/ University of Cape Town Clinical Research Center for Allergology Cape Town, South Africa. Sean D. Sullivan, PhD Kanagawa, Japan University of Washington Jean Bousquet, MD, PhD Seattle, Washington, USA Professor Amiran Gamkrelidze Montpellier University and INSERM Tbilisi, Georgia Montpellier, France Sally E. Wenzel, MD National Jewish Medical/Research Center Dr. Michiko Haida Tim Clark, MD Denver, Colorado, USA Hanzomon Hospital, National Heart and Lung Institute Chiyoda-ku, Tokyo, Japan London United Kingdom Heather J. Zar, MD University of Cape Town Dr. Carlos Adrian Jiménez Ken Ohta. MD, PhD Cape Town, South Africa San Luis Potosí, México Teikyo University School of Medicine Tokyo, Japan REVIEWERS Sow-Hsong Kuo, MD National Taiwan University Hospital Pierluigi Paggiaro, MD Louis P. Boulet, MD Taipei, Taiwan University of Pisa Hopital Laval Pisa, Italy Quebec, QC, Canada Eva Mantzouranis, MD University Hospital Soren Erik Pedersen, MD William W. Busse, MD Heraklion, Crete, Greece Kolding Hospital University of Wisconsin Kolding, Denmark Madison, Wisconsin USA Dr. Yousser Mohammad Tishreen University School of Medicine Manuel Soto-Quiroz, MD Neil Barnes, MD Lattakia, Syria Hospital Nacional de Niños The London Chest Hospital, Barts and the San José, Costa Rica London NHS Trust Hugo E. -

1 Pathology Week 13: the Lung Ver.2
Pathology week 13: the Lung ver.2 Atelectasis - either incomplete expansion of the lungs (neonatal) or collapse of previously inflated lung, producing areas of relatively airless pulmonary parenchyma - reduces oxygenation, predisposes to infection - reversible except if caused by contraction o acquired either: resorption atelectasis (obstruction airway, resorption trapped oxygen) • mucus plugging eg asthma, bronchitis, bronchiectasis, post op, FBs • mediastinum shifts towards affected lung compression atelectasis • effusion, pneumothorax, haemothorax, peritonitis – basal atelectasis • mediastinum shift away from affected lung contraction atelectasis • when local or general fibrotic changes in lung prevent full expansion Acute Lung Injury - a spectrum of pulmonary lesions (endothelial and epithelial) - initiated by many factors - susceptibility my be heritable - mediators include cytokines, oxidants, growth factors (incl TNF, IL1, IL6, IL10, TGFβ) - may manifest as congestion, oedema, surfactant disruption, atelectasis - may progress to ARDS or acute interstitial pneumonia Pulmonary Oedema - most common haemodynamic mechanism: ↑ hydrostatic pressure in LVF - heavy, wet lungs – initially basal due to greater hydrostatic pressure - alveolar capillaries engorged, intra-alveolar granular pink precipitate, alveolar microhaemorrhages and haemosiderin-laden macrophages (“heart failure” cells ) - longstanding LVF – many haemosiderin-laden macrophages, fibrosis, thickening alveolar walls – lungs firm and brown (brown induration) Oedema caused -

Volume 46 Contents
VOLUME 46 CONTENTS No 1 JANUARY 1991 Page Original articles 1 Risk of tuberculosis in immigrant Asians: culturally acquired immunodeficiency? P J Finch, F J C Millard, J D Maxwell 6 Effect of negative pressure ventilation on arterial blood gas pressures and inspiratory muscle strength during an exacerbation of chronic obstructive lung disease J M Montserrat, J A Martos, A Alarcon, R Celis, V Plaza, Thorax: first published as on 1 January 1991. Downloaded from C Picado 9 The protective effect of a beta2 agonist against excessive airway narrowing in response to bronchoconstrictor stimuli in asthma and chronic obstructive lung disease E H Bel, A H Zwinderman, M C Timmers, i H Dijkman, P J Sterk 15 Corticosteroid treatment as a risk factor for invasive aspergillosis in patients with lung disease L B Palmer, H E Greenberg, M J Schiff 21 Continuous extrapleural intercostal nerve block after pleurectomy E J Mozell, S Sabanathan, A J Mearns, P J Bickford-Smith, M R Majid, C Zografos 25 Erythropoietin concentrations in obstructive sleep apnoea J M Goldman, R M Ireland, M Berthon-Jones, R R Grunstein, C E Sullivan, J C Biggs 28 Effects ofhypercapnia and hypocapnia on respiratory resistance in normal and asthmatic subjects F J J van den Elshout, C L A van Herwaarden, H Th M Folgering 33 Abnormal lung function associated with asbestos disease of the pleura, the lung, and both: a comparative analysis K H Kilburn, R H Warsaw 39 Cysteine and glutathione concentrations in plasma and bronchoalveolar lavage fluid after treatment with N-acetylcysteine M -
Acdsee PDF Image
• • NATIONAL GUIDELINES STHMA RONCHIOLITIS ....OPD • • 3rd Edition 2005 . " " • - - • • • • Asthma Association • Bangladesh National Asthma Centre, National Institute of Diseases of the Chest & Hospital Mohakhali, Dhaka·1212, Bangladesh www.asthmabd.org Published by: PREFACE Asthma Association, Bangladesh An Appeal for Dissemination of Knowledge National Asthma Center NIDCH Campus, Mohakhali Bismillahir Rahmanir Rahim. Dhaka-1212, Bangladesh Assalamu Alaikum. Address for correspondence: It is a pleasure for me as we got the opportunity from Almighty Allah to National Asthma Center publish the 3rd edition of our National Guidelines with an intention to National Institute of Diseases of the Chest and Hospital disseminate proper knowledge through out the country. The 1st edition of Mohakhali, Dhaka-1212, Bangladesh "National Asthma Guidelines" was published in 1999, which was revised and Tel: +88-02-9887050 the 2nd edition was published in 2001. By this time new information has came E-mail: asmaasso@bttb• .net.bd out from different research papers in home and abroad. Many physicians of the Web : www.asthmabd.org country took interest and send comments. After having long discussion with various groups we are now providing this updated version of the guidelines. First Edition : November 1999 Second Edition : April 2001 This time we included management updates of bronchiolitis and COPD in our Third Edition : May 2005 guidelines. It is essential for all phYSicians dealing with asthma to know the diagnosis and management of bronchiolitis and COPD, because they are, to some extent, symptomatically looking alike asthma. Contents of this book, whole or in part can be reproduced for research, academic or educational purposes. Acknowledgement to the Asthma In Bangladesh more than 100 million people are suffering from cough and Association, Bangladesh will be highly appreciated. -

Assessing the Risk of Attack in the Management of Asthma: a Review and Proposal for Revision of the Current Control-Centred Paradigm
Prim Care Respir J 2013; 22(3): 344-352 CLINICAL REVIEW Assessing the risk of attack in the management of asthma: a review and proposal for revision of the current control-centred paradigm *John D Blakey1, Kerry Woolnough2, Jodie Fellows2,3, Samantha Walker4, Mike Thomas5, Ian D Pavord6 1 Clinical Sciences, Liverpool School of Tropical Medicine, Liverpool, UK 2 Severe and Brittle Asthma Unit, Heartlands Hospital, Birmingham, UK 3 Clinical Health Psychology, Birmingham & Solihull Mental Health Foundation Trust, Birmingham, UK 4 Asthma UK, London, UK 5 Centre for Academic Primary Care, University of Southampton, UK 6 Institute for Lung Health, Glenfield Hospital, Leicester, UK Received 26th November 2012; resubmitted 27th February 2013; revised 9th April 2013; accepted 13th April 2013; online 2nd July 2013 Abstract Asthma guidelines focus on day-to-day control of symptoms. However, asthma attacks remain common. They continue to cause mortality and considerable morbidity, and are a major financial burden to the UK National Health Service (NHS) and the wider community. Asthma attacks have chronic consequences, being associated with loss of lung function and significant psychological morbidity. In this article we argue that addressing daily symptom control is only one aspect of asthma treatment, and that there should be a more explicit focus on reducing the risk of asthma attacks. Management of future risk by general practitioners is already central to other conditions such as ischaemic heart disease and chronic renal impairment. We therefore propose a revised approach that separately considers the related domains of daily control and future risk of asthma attack. We believe this approach will have advantages over the current ‘stepwise’ approach to asthma management. -
Severe Asthma
SEVERE ASTHMA Tamara Kerbelker Severe asthma Kerbelker Feb 2012 OBJECTIVES • Is it asthma? • What is severe asthma? • Differential diagnosis • Workup • Treatment Severe asthma Kerbelker Feb 2012 CASE 1 • 9 year old girl • Attends Allergy clinic since age 1 year • Early onset wheeze – 1st presentation at age 7 weeks • Other medical history – ENT grommets bilateral glue ear – GIT chronic constipation Severe asthma Kerbelker Feb 2012 CASE 1 cont • Allergy – Sensitised hdm / cat / grass mix/ dog – Persistent allergic rhinitis – Asthma – persistent severe uncontrolled • Seretide 25/250 initiated age 5 (trial of LTRA made no difference) • PEF consistently 80 – 90%expected Severe asthma Kerbelker Feb 2012 CASE 1 cont • Admission acute exacerbation March 2011 – Amoxil commenced at primary care – Augmentin in acute care – No change and given Azithromycin – Prednisone 2 weeks! – Assumed severe viral associated excaerbation but took 3 weeks to settle completely and expected PEF not ever achieved FURTHER WORK UP COMMENCED Severe asthma Kerbelker Feb 2012 CASE 2 • 11 years old boy • Asthma since age 4 years • Adherent • Coke bottle spacer • Uncontrolled – SABA use daily, exertional symptoms, cough 2 / week • Medication – Seretide 25/250 – Singulair 10mg – Omeprazole 20mg Severe asthma Kerbelker Feb 2012 CASE 2 cont • Milk scan 2009 – mild reflux, started on PPI • Asthma still uncontrolled • Milk scan repeated 2011 – “no reflux” Severe asthma Kerbelker Feb 2012 CASE 3 • 6 year old boy • Referred from MOPD uncontrolled asthma on ICS 400mcg BD Severe -

Journal of Nursing and Health Sciences
Research & Reviews: Journal of Nursing and Health Sciences Asthma: A common chronic inflammatory disease Anurashree Verma1*, Charushila Biswas2 SRM University, Tamilnadu, India 1SRM University, Chennai, India 2VIT University, Vellore, India Mini Review Article Received: 25/05/2015 Revised: 28/05/2015 Accepted: 09/06/2015 *For Correspondence Anurashree Verma, SRM University, Chennai, Tamilnadu, India, Tel: +91 9941372586; E-mail: [email protected] DESCRIPTION Asthma is a chronic lung disease which cause inflammation in the bronchioles, narrow the airways and characterized by airflow obstruction and bronchospasm, coughing, chest tightness, wheezing, shortness of breath referred as asthma attack [1,5,9,16,27,32,52,69,73,78]. The major risk factors of asthma are allergens like pollens, dust, smoking, mites in bedding and chemical irritants [63,85]. The disease may also trigger by extreme emotion, anger, fear, cold air and physical exercise and also affects distal lung parenchyma [10,25,31,33,35,75,76]. Laryngopharyngeal reflux is one of the suspected exacerbating factors for developing asthma and studies are going on to understand the real association between these two common diseases [44]. Even endocrine disorders like obesity and diabetes influence the prevalence of asthma [55,61,68,71]. World health organization has proposed different groupings and phenotypes of the severe asthma and differentiated into two categories: treatment resistance severe asthma (TRSA) and difficult to treat severe asthma (DTTSA). TRSA includes patients using maximum levels of inhaled medications and not achieving adequate levels of control whereas DTTSA is a controllable severe asthma [21]. Asthma is a treatable disease affecting more than 300 million people worldwide but if it is poorly controlled can become life threatening [2,30,41,43,47,70,86]. -

Diycult Asthma: Beyond the Guidelines
Arch Dis Child 1999;80:201–206 201 Arch Dis Child: first published as 10.1136/adc.80.2.201 on 1 February 1999. Downloaded from PERSONAL PRACTICE DiYcult asthma: beyond the guidelines Ian Balfour-Lynn The current guidelines for prophylactic treat- should be considered, some more rare than ment of paediatric asthma culminate in the others. Relevant investigations should be car- addition of regular oral corticosteroids after a ried out when the history or examination stepwise increase in treatment.1–3 However, suggests one of these other diagnoses (table 1). there are still a few patients whose asthma is In particular, the presence of finger clubbing is not controlled despite such maximal conven- incompatible with the lone diagnosis of tional treatment and these children are often asthma. An asthmatic child may be aVected by referred to a tertiary paediatric respiratory another condition that contributes to or centre. Childhood asthma has several manifes- worsens the asthma symptoms. In particular, tations and diVerent approaches may be gastro-oesophageal reflux should be looked for required for diVerent patterns of asthma. and treated although its significance is not Unfortunately, some of these children are diY- always clear.5 Immunodeficiencies should also cult to treat. These include infants with severe be excluded; an initial screen should include recurrent viral wheezing who respond poorly to serum immunoglobulins and IgG subclasses, medication but generally have a good progno- complement concentrations, and antibody re- sis. There are those said to have “brittle sponses to common antigens (diphtheria, teta- asthma”; this has been classified into those with nus, Haemophilus influenzae type b, and pneu- a wide peak flow variation despite maximal mococcus) (Jones A, personal communication, treatment (type 1), and those who are well 1998). -
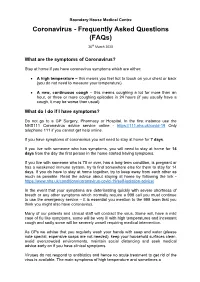
Coronavirus - Frequently Asked Questions (Faqs)
Boundary House Medical Centre Coronavirus - Frequently Asked Questions (FAQs) 26th March 2020 What are the symptoms of Coronavirus? Stay at home if you have coronavirus symptoms which are either: A high temperature – this means you feel hot to touch on your chest or back (you do not need to measure your temperature) A new, continuous cough – this means coughing a lot for more than an hour, or three or more coughing episodes in 24 hours (if you usually have a cough, it may be worse than usual). What do I do if I have symptoms? Do not go to a GP Surgery, Pharmacy or Hospital. In the first instance use the NHS111 Coronavirus advice service online - https://111.nhs.uk/covid-19 Only telephone 111 if you cannot get help online. If you have symptoms of coronavirus you will need to stay at home for 7 days . If you live with someone who has symptoms, you will need to stay at home for 14 days from the day the first person in the home started having symptoms. If you live with someone who is 70 or over, has a long-term condition, is pregnant or has a weakened immune system, try to find somewhere else for them to stay for 14 days. If you do have to stay at home together, try to keep away from each other as much as possible. Read the advice about staying at home by following the link - https://www.nhs.uk/conditions/coronavirus-covid-19/self-isolation-advice/ In the event that your symptoms are deteriorating quickly with severe shortness of breath or any other symptoms which normally require a 999 call you must continue to use the emergency service – it is essential you mention to the 999 team that you think you might also have coronavirus. -

Clinical Asthma Syndromes and Important Asthma Mimics
Clinical Asthma Syndromes and Important Asthma Mimics Christopher S King MD and Lisa K Moores MD Introduction Clinical Phenotypes Severity-Defined Exacerbation-Prone Asthma With Chronic Airflow Obstruction Treatment-Resistant Asthma Asthma Defined by Age at Onset Trigger-Related Phenotypes Inflammatory Phenotypes Why Do Phenotypes Matter? Asthma Mimics Chronic Obstructive Pulmonary Disease Vocal Cord Dysfunction Summary Asthma is a heterogeneous disorder with multiple clinical phenotypes. Phenotypes can be grouped into clinical or physiological, trigger-defined, and inflammatory phenotypes. Treatment based on inflammatory phenotyping improves clinical measures of asthma morbidity. Further study of in- dividual asthma phenotypes will improve understanding of their immunologic and pathologic char- acteristics and improve diagnosis and therapy. Because asthma is a common disorder with non- specific presenting features, other disorders are often misdiagnosed as asthma. A high index of suspicion for alternative diagnoses must be maintained when evaluating a patient who presents with clinical features suggestive of asthma, particularly if the patient presents with atypical symptoms or fails to respond to therapy. Key words: asthma; phenotypes; asthma, etiology; asthma, genetics; asthma, mimics; vocal cord dysfunction. [Respir Care 2008;53(5):568–580] Introduction are poorly characterized, with little known about the un- derlying pathophysiology. The recent development of tar- Asthma is probably not a single disease, but rather a complex of multiple, separate syndromes that overlap. Sev- eral classification schemes have been proposed, but many The opinions and assertions in this report are the private views of the authors and are not to be construed as official or as the views of the Department of the Army or the Department of Defense.