Medicaid Coverage and Other Healthcare Resources in Pittsburgh
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
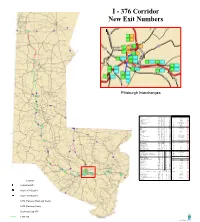
Pittsburgh Interchanges
I - 376 Corridor New Exit Numbers Pittsburgh Interchanges I-376 Exit Name County Old Route Old Exit New Route New I-376 Exit Route # Status Youngstown Mercer PA 60 I-376 1A I-80 West Approved Mercer Mercer PA 60 I-376 1B I-80 East Approved Mercer/West Middlesex (Eastbound) Mercer PA 60 I-376 1C PA 318 Approved West Middlesex Mercer PA 60 I-376 2PA 18Approved New Wilmington/Pulaski Lawrence PA 60 25 I-376 5 PA 208 Approved Mitchell Road Lawrence PA 60 24 I-376 9 To PA 18 Approved Youngstown/Sampson St. (Westbound) Lawrence PA 60 I-376 12 US 422 West/Business 422 East Approved Youngstown (Eastbound) Lawrence PA 60 I-376 12A To US 422 West Approved Sampson Street (Eastbound) Lawrence PA 60 I-376 12B Business US 422 East Approved State Street/Poland, Ohio Lawrence PA 60 I-376 13 US 224 Approved Butler Lawrence PA 60 45 I-376 15 US 422 East Approved Mt. Jackson Lawrence Toll 60 43 Toll 376 17 PA 108 Approved Moravia Lawrence Toll 60 40 Toll 376 20 PA 168 Approved PA Turnpike Harrisburg/Ohio Beaver Toll 60 33 Toll 376 26 I-76/PA Turnpike Approved Beaver Falls Beaver Toll 60 31 Toll 376 29 PA 551/To PA 18 Approved Chippewa Beaver PA 60 15 I-376 31 PA 51 Approved Brighton Beaver PA 60 14 I-376 36 Approved Beaver/Midland (Eastbound) Beaver PA 60 13 I-376 38 PA 68 Approved Midland (Westbound) Beaver PA 60 13-B I-376 38-A PA 68 West Approved Beaver (Westbound) Beaver PA 60 13-A I-376 38-B PA 68 East Approved Monaca/Shippingport Beaver PA 60 12 I-376 39 PA 18 Approved Center Beaver PA 60 11 I-376 42 Approved Aliquippa Beaver PA 60 10 I-376 45 Approved -
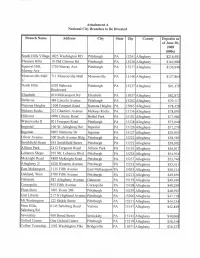
National City Branches to Be Divested
Attachment A National City Branches to Be Divested Branch Name Address City State Zip County Deposits as of June 30, 2008 WOOs) South Hills Village 1825 Washington RD Pittsburgh PA 15241 Allegheny $216,481 Pleasant Hills 10 Old Clairton Rd Pittsburgh PA 15236 Allegheny $164,980 Squirrel Hill, 1730 Murray Ave. Pittsburgh PA 15217 Allegheny $136,946 Murray Ave Monroeville Mall 711 Monroeville Mall Monroeville PA 15146 Allegheny $127,86<1 1/ North Hills 6203 Babcock Pittsburgh PA 15237 Allegheny $91,47c Boulevard Elizabeth 810 McKeesport Rd Elizabeth PA 15037 Allegheny $82,87= Bellevue 484 Lincoln Avenue Pittsburgh PA 15202 Allegheny $79,11" Natrona Heights 1509 Freeport Road Natrona Heights PA 15065 Allegheny $78,42 Mckees Rocks 527 Chartiers Avenue McKees Rocks PA 15136 Allegheny $78,095 Hillcrest 4996 Library Road Bethel Park PA 15102 Allegheny $77,984 Waterworks II 831 FreeDortRoad Pittsburgh PA 15238 Allegheny $73,040 mperial 100 W. Allegheny Rd Imperial PA .15126 Allegheny $71,279 £ngomar 9605 Harmonv Dr Ingomar PA 15127 Allegheny $70,953 Oliver Avenue 300 Sixth Avenue Bldg Pittsburgh PA 15222 Allegheny $58,583 Smithfield Street 445 Smithfield Street Pittsburgh PA 15222 Allegheny $58,00" IAllisonPark 2412 Ferguson Road Allison Park PA 15101 Allegheny $56,01 lLebanon Shops 305 Mt. Lebanon Blvd. Pittsburgh PA 15234 Allegheny $54,95<1 Mcknight Road 4808 McKnight Road Pittsburgh PA 15237 Allegheny $53,74( llegheny 2/ 1020 Western Avenue Pittsburgh PA 15233 Allegheny $53,411 East Mckeesport 1135 Fifth Avenue East McKeesDort PA 15035 Allegheny -

Neighborhood Parks Shelter Guide
Neighborhood Parks Shelter Guide Banksville Park $225.00 / $150.00 (without alcohol) Indoor heated facility/ Portable toilets/ Equipped kitchen/ Access to playground and ball field. Capacity: 70 people Location: Crane Ave. and Carnahan Rd. Open: Year round Please Note: playgrounds, swimming pools, fields, etc. are not exclusively reserved for the permit holder unless indicated otherwise. Brighton Heights Park $150.00 / $75.00 (without alcohol) Open-air shelter/ Portable toilet(s)/ No electric. Capacity: 24 people Location: Brighton Woods Rd. & Weltz Way Open: May thru September Only available weekdays from 1PM-9PM June 8th-August 31st. Please Note: playgrounds, swimming pools, fields, etc. are not exclusively reserved for the permit holder unless indicated otherwise. Brookline Park $150.00 / $75.00 (without alcohol) Open-air shelter/ Portable toilet(s)/ Outdoor grill/ No electric/ Playground and fields available. Capacity: 24 people Location: 1400 Brookline Blvd. Open: May thru September Please Note: playgrounds, swimming pools, fields, etc. are not exclusively reserved for the permit holder unless indicated otherwise. Chartiers Park $115.00 / $40.00 (without alcohol) Open-air shelter/ Portable Toilet(s)/ Access to fields. Capacity: 10 people Location: Chartiers Ave and Eyre Way Open: May thru September Please Note: playgrounds, swimming pools, fields, etc. are not exclusively reserved for the permit holder unless indicated otherwise. McKinley Park $150.00 / $75.00 (without alcohol) Open-air shelter/ Portable toilet(s)/ Outdoor grill/ No electric/ Access to playground, ball field, tennis, and hockey courts available. Capacity: 24 people Location: Bausman St. Open: May thru September Please Note: playgrounds, swimming pools, fields, etc. are not exclusively reserved for the permit holder unless indicated otherwise. -

A Qualitative Study of Single Mothers in Allegheny County: a 100 Percent Pittsburgh Project
THERE’S A STIGMA AROUND BEING A SINGLE PARENT. THAT’S WHAT I CHOOSE, BUT PEOPLE LOOK DOWN ON YOU. ‘YOU’RE NOT MARRIED? AND YOU HAVE THOSE KIDS?’ DAMN STRAIGHT I HAVE THOSE KIDS. BE- CAUSE I LOVE MY KIDS. | I USED TO WEAR A WEDDING RING ON MY RING FINGER WHEN I WENT TO THE COMMUNITY MARKET, TO A QUALITATIVE STUDY GO TO THE DOCTOR’SOF SINGLE MOTHERS IN OFFICE, AND ALLEGHENY COUNTY A 100 PERCENT EVERYWHERE ELSE. | I NEED AN PITTSBURGH EDUCATION AND I DON’T KNOW PROJECT HOW TO DO IT, I’M STUCK. | THE IDEAS ARE THERE. WILKINSBURG BALDWIN SOUTHSIDE BRA DDOCK HILL DISTRICT HOMEWOOD WEST END HOMEWOOD WEST END NORTHSIDE BRAD- DOCK UNIONTOWN HOMESTEAD EAST HILLS WILKINSBURG BALDWIN SOUTHSIDE HILL DIS- TRICT MCKEESPORT HOMEWOOD WEST END BRADOCK NORTHSIDE UNIONTOWN HOMESTEAD EAST HILLS NORTHSIDE UNIONTOWN HOME- STEAD EAST HILLS WILKINSBURG BALDWIN SOUTHSIDE MCKEESPORT HILL DISTRICT WEST Foreward from Maxwell King , President and CEO 3 END NORTHSIDE BRADDOCKThe Pittsburgh Foundation UNIONTOWN is Listening HOME4 - Background 6 STEAD EAST HILLS WILKINSBURGProject Design BALDWIN 9 Key Findings 10 DWIN HOMEWOOD WESTRecommendations END NORTHSIDE 24 DE Methodology / Acknowledgements 32 UNIONTOWN BRADDOCKReferences HOMESTEAD WILKINS34 - BURG BALDWIN SOUTHSIDE UNIONTOWN HOME- STEAD EAST HILLS WILKINSBURG BALDWIN SOUTHSIDE HILL DISTRICT MCKEESPORT 3 FOREWARD WHEN WE ADOPTED 100 PERCENT PITTSBURGH, The Pittsburgh Foundation’s organizing principle in 2015, the goal was to direct a majority of our convening and policy work, advocacy and grantmaking, to serve the specific populations in our community who were most directly affected by poverty. Our staff relied upon rigorous quantitative research to develop a sobering picture of the lives of those who struggled to meet basic needs in a region that is, for some, a national example of prosperity and opportunity. -

Urban Essay Fall 06 Website.Pub
University of Pittsburgh’s Urban Studies Association Newsletter Issue 13 October 2005 T HE PRESIDENT’ S A DDRESS My fellow Urbanites— We’re back! The urbanSA (yes, we had a branding change this year) is starting Fall 2005 renewed and ready to explore the city again. After a mid-summer planning session with officers, alumni, and current members, the urbanSA is setting up its first strategic plan to make sure we’re sustain- able enough for years to come. Put your two cents into our strategic plan by taking our first-ever online survey, available from our website’s front page. Your opinion will affect how we plan our events in the not-so-distant future. And speaking of events... We know how much you heart getting out into town. So TRACKS OF STEEL: LIGHT far, we’ve set up Oakland cleanups with the Oakland Planning and Development Corporation’s Adopt-a-Block program, an- R AIL IN PITTSBURGH other work day with Habitat for Humanity’s Panther Chapter B Y PATRICK SINGLETON (which was a huge success even in last winter’s 19-degree weather), a tour of Regent Square, with more tours of East One of the most hotly contested issues recently is, not surprisingly, Liberty and other hotspots in the East End in the works, plus a government spending on a transportation project. This time, it is a light talk with Boldly Live Where Others Won’t author Mark Harvey rail extension to the T termed the North Shore Connector. With both Smith and a screening of the End of Suburbia. -

City of Pittsburgh Neighborhood Profiles Census 2010 Summary File 1 (Sf1) Data
CITY OF PITTSBURGH NEIGHBORHOOD PROFILES CENSUS 2010 SUMMARY FILE 1 (SF1) DATA PROGRAM IN URBAN AND REGIONAL ANALYSIS UNIVERSITY CENTER FOR SOCIAL AND URBAN RESEARCH UNIVERSITY OF PITTSBURGH JULY 2011 www.ucsur.pitt.edu About the University Center for Social and Urban Research (UCSUR) The University Center for Social and Urban Research (UCSUR) was established in 1972 to serve as a resource for researchers and educators interested in the basic and applied social and behavioral sciences. As a hub for interdisciplinary research and collaboration, UCSUR promotes a research agenda focused on the social, economic and health issues most relevant to our society. UCSUR maintains a permanent research infrastructure available to faculty and the community with the capacity to: (1) conduct all types of survey research, including complex web surveys; (2) carry out regional econometric modeling; (3) analyze qualitative data using state‐of‐the‐art computer methods, including web‐based studies; (4) obtain, format, and analyze spatial data; (5) acquire, manage, and analyze large secondary and administrative data sets including Census data; and (6) design and carry out descriptive, evaluation, and intervention studies. UCSUR plays a critical role in the development of new research projects through consultation with faculty investigators. The long‐term goals of UCSUR fall into three broad domains: (1) provide state‐of‐the‐art research and support services for investigators interested in interdisciplinary research in the behavioral, social, and clinical sciences; (2) develop nationally recognized research programs within the Center in a few selected areas; and (3) support the teaching mission of the University through graduate student, post‐ doctoral, and junior faculty mentoring, teaching courses on research methods in the social sciences, and providing research internships to undergraduate and graduate students. -

State Rep. Dan Deasy Summer 2013 I Have Organized a Bus Trip for Tuesday, October 1, 2013
STATE REP. DAN DEASY www.pahouse.com/Deasy Summer 2013 I HAVE ORGANIZED A BUS TRIP FOR TUESDAY, OCTOBER 1, 2013. P.O. Box 202027 THE BUS TRIP WILL INCLUDE: Harrisburg, PA 17120-2027 BUS TRIP n A visit to the Flight 93 National Memorial in Shanksville 27th Legislative District n A tour of the state Capitol n A visit to the Antique Automobile Club of America Museum for O c to b e r 1 their Pop Culture & Cars Retro Adventure exhibit STATE REP. DAN DEASY n A Visit to Hershey’s Chocolate World Reservations will be taken starting September 3. The cost of the trip is DISTRICT OFFICE: 436 S. Main St., Suite 100 • Pittsburgh, PA 15220 • (412) 928-9514 $50 per person. Lunch and dinner are on your own and not included in Mon. – Fri. 8:30 a.m. to 4:30 p.m.; extended hours on Thurs. until 6 p.m. the trip fee. If you would like more details about the trip, please contact SATELLITE OFFICE: Avalon Borough Building • 640 California Ave. • Pittsburgh, PA 15202 • (412) 761-5820, ext. 15 • By appointment my office at 412-928-9514. CAPITOL OFFICE: 323 Irvis Office Building • P.O. Box 202027 • Harrisburg, PA 17120-2027 • (717) 772-8187 lpo • kaf • 0713 an updaTe On legiSlaTive reappOrTiOnMenT: !Clip and save Future changes to the 27th legislative district Fall calendar OF evenTS: CURRENT DISTRICT 27 – Effective through 11/30/14 Avalon Borough McKees Rocks Borough, Each fall, I host a series of Tuesday, September 3 Ben Avon Borough 1-1, 1-2, 2-1, 2-2, 3-2, 3-3 September events around my district. -

Downtown-Uptown-Oakland-East End Bus Rapid Transit Pittsburgh, Pennsylvania Small Starts Project Development (Rating Assigned November 2019)
Downtown-Uptown-Oakland-East End Bus Rapid Transit Pittsburgh, Pennsylvania Small Starts Project Development (Rating Assigned November 2019) Summary Description Proposed Project: Bus Rapid Transit 15 Miles, 46 Stations Total Capital Cost ($YOE): $249.90 Million Section 5309 CIG Share ($YOE): $99.95 Million (40.0%) Annual Operating Cost (opening year 2024): $62.16 Million Existing Corridor Ridership (Warranted): 37,000 Daily Linked Trips Overall Project Rating: High Project Justification Rating: Medium-High Local Financial Commitment Rating: High Project Description: The Port Authority of Allegheny County (PAAC) proposes to implement Bus Rapid Transit (BRT) service between Downtown Pittsburgh and neighborhoods to the east. The proposed service is planned to operate on exclusive lanes between downtown and Oakland. In Oakland, the service branches off in three directions – toward Oakland-East, Highland Park, and Squirrel Hill. The Highland Park and Squirrel Hill branches are anticipated to operate in mixed traffic as corridor-based BRT services, while the Oakland-East branch is anticipated to operate in dedicated lanes along the Martin Luther King, Jr. East Busway. The project includes queue jump lanes, the purchase of 15 battery-powered articulated electric buses, branded BRT stations, transit signal priority, and charging stations. The service is planned to operate from 4:00 am to 2:00 am on weekdays, and from 5:00 am to 2:00 am on weekends. The service plan includes buses operating every three to four minutes during weekday peak periods, and every four to eight minutes during weekday off-peak periods and evenings. On weekends, the service plan includes buses operating every five to eight minutes throughout the day. -

Now Offering Sports Physicals!
Now offering sports physicals! Check https://www.chp.edu/our-services/mobile-medical-clinic/schedule for the most up-to-date locations and dates this summer! All clinics run from 10AM – 2PM Neighborhood Location Dates Braddock Braddock Civic Plaza June 24th 451 Braddock Ave, Braddock, PA 15104 July 22nd Chartiers Chartiers Early Childhood Center June 8th 3799 Chartiers Ave, Pittsburgh, PA 15204 June 10th Clairton Family Dollar June 4th 533 Miller Ave, Clairton, PA 15025 Coraopolis Cornell School District August 31st 1099 Maple St, Coraopolis, PA 15108 Crafton/West End The First United Presbyterian Church of June 29th Crafton Heights July 17th 50 Stratmore Ave, Pittsburgh, PA 15205 Hazelwood Old S&R Market Lot July 8th 4915 Second Ave, Pittsburgh, PA 15207 Hill District Ebenezer Baptist Church July 6th 2001 Wylie Ave, Pittsburgh, PA 15219 August 12th Homestead/Munhall Steel Valley Middle School July 27th 3114 Main St, Munhall, PA 15120 July 29th Homewood Homewood-Brushton YMCA June 25th 7140 Bennett St, Pittsburgh, PA 15208 July 23rd Mt. Oliver Hilltop Family Care Connection July 10th 1635 Arlington Ave, Mount Oliver, PA 15210 Natrona Heights Allegheny Valley YMCA July 2nd 5021 Freeport Rd, Natrona Heights, PA August 6th 15065 New Castle New Castle Jr/Sr High School July 20th 300 E Lincoln Ave, New Castle, PA 16101 August 19th New Kensington Valley Points Family YMCA June 22nd 800 Constitution Blvd, New Kensington, July 16th PA 15068 North Side Children’s Museum of Pittsburgh June 17th 10 Children’s Way, Pittsburgh, PA 15212 July 15th The Pittsburgh Project July 24th 2801 N Charles St, Pittsburgh, PA 15214 August 5th Penn Hills Penn Hills Family Care Connection June 18th 10 Duff Rd, Penn Hills, PA 15235 July 31st Wilkinsburg Wilkinsburg School District June 19th 718 Wallace Ave, Pittsburgh, PA 15221 July 13th Children’s Hospital Injury Prevention will be on site at this location and date distributing free bike helmets. -

City of Pittsburgh, Allegheny County, Pennsylvania Planning Sector 4: West Pittsburgh West End & Elliott Neighborhoods Report of Findings and Recommendations
Architectural Inventory for the City of Pittsburgh, Allegheny County, Pennsylvania Planning Sector 4: West Pittsburgh West End & Elliott Neighborhoods Report of Findings and Recommendations The City of Pittsburgh In Cooperation With: Pennsylvania Historical & Museum Commission September 2018 Paving Chartiers Avenue in Elliott, April 28, 1910, view northwest from Lorenz Avenue. Pittsburgh City Photographer’s Collection, Archives of Industrial Society, University of Pittsburgh Prepared By: Michael Baker International, Inc. Jesse A. Belfast Justin Greenawalt and Clio Consulting Angelique Bamberg with Cosmos Technologies, Inc. James Brown The Architectural Inventory for the City of Pittsburgh, Allegheny County, Pennsylvania, was made possible with funding provided by the Pennsylvania State Historic Preservation Office (PA SHPO), the City of Pittsburgh, and the U.S. Department of the Interior National Park Service Certified Local Government program. The contents and opinions contained in this document do not necessarily reflect the views or policies of the Department of the Interior. This program receives federal financial assistance for identification and protection of historic properties. Under Title VI of the Civil Rights Act of 1964, Section 504 of the Rehabilitation Act of 1973, and the Age Discrimination Act of 1975, as amended, the U.S. Department of the Interior prohibits discrimination on the basis of race, color, national origin, disability, or age in its federally assisted programs. If you believe you have been discriminated against -

North Campus & West Hills Center Resource Guide
NORTH CAMPUS & WEST HILLS CENTER RESOURCE GUIDE FOOD HOUSING CLOTHING/CONSIGMENT STORES CRISIS INTERVENTION HOTLINES FREE HEALTH CLINICS OTHER RESOURCES Provided by: JOB PLACEMENT & CAREER SERVICES CCAC-North Campus 8701 Perry Highway, Pittsburgh, PA 15237 www.ccac.edu Last Updated: March 2018 Table of Contents Food and Housing Resources ................................................... 3 Allegheny County ..................................................................... 3 Beaver County .......................................................................... 6 Butler County ............................................................................ 8 Clothing/Consignment Stores ................................................. 10 Crisis Intervention Hotlines ..................................................... 12 Free Health Clinics .................................................................... 14 Transportation Services ........................................................... 15 Homeless Services .................................................................. 16 2 FOOD and HOUSING RESOURCES ALLEGHENY COUNTY Housing Assistance Allegheny County Bureau of Hunger and Housing & Food 412-350-4354 Housing Services Assistance www.alleghenycounty.us One Smithfield Street, Pittsburgh, PA 15222 Urban League of Greater Pittsburgh Housing & Food www.ulpgh.org 610 Wood Street Assistance Pittsburgh, PA 15222 Neighbor-Aid (United Pittsburgh crisis relief Way) 412-255-1155 fund- helping to meet 5 PPG Place, 2nd floor, www.neighbor-aid.org -

Profile of Change in the City of Pittsburgh
PROFILE OF CHANGE IN THE CITY OF PITTSBURGH COMPARISON OF 2009‐2013 AND 2014‐2018 AMERICAN COMMUNITY SURVEY (ACS) ESTIMATES FOR THE CITY OF PITTSBURGH AND NEIGHBORHOODS PROGRAM IN URBAN AND REGIONAL ANALYSIS UNIVERSITY CENTER FOR SOCIAL AND URBAN RESEARCH UNIVERSITY OF PITTSBURGH JANUARY 2020 PROFILE OF CHANGE IN THE CITY OF PITTSBURGH – JANUARY 2020 Table of Contents Data and Methodology ............................................................................................ 2 Population Trends in the City of Pittsburgh ............................................................. 3 Age ........................................................................................................................ 4 Race ...................................................................................................................... 5 Educational Attainment ........................................................................................ 7 Commuting ........................................................................................................... 8 Housing Tenure ..................................................................................................... 9 Poverty ................................................................................................................ 10 Veterans .............................................................................................................. 11 Data Profiles ..........................................................................................................