Quarterly Performance Report from October 01, 2017 to December 31, 2017
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Rakhine State Needs Assessment September 2015
Rakhine State Needs Assessment September 2015 This document is published by the Center for Diversity and National Harmony with the support of the United Nations Peacebuilding Fund. Publisher : Center for Diversity and National Harmony No. 11, Shweli Street, Kamayut Township, Yangon. Offset : Public ation Date : September 2015 © All rights reserved. ACKNOWLEDGMENTS Rakhine State, one of the poorest regions in Myanmar, has been plagued by communal problems since the turn of the 20th century which, coupled with protracted underdevelopment, have kept residents in a state of dire need. This regrettable situation was compounded from 2012 to 2014, when violent communal riots between members of the Muslim and Rakhine communities erupted in various parts of the state. Since the middle of 2012, the Myanmar government, international organisations and non-governmen- tal organisations (NGOs) have been involved in providing humanitarian assistance to internally dis- placed and conflict-affected persons, undertaking development projects and conflict prevention activ- ities. Despite these efforts, tensions between the two communities remain a source of great concern, and many in the international community continue to view the Rakhine issue as the biggest stumbling block in Myanmar’s reform process. The persistence of communal tensions signaled a need to address one of the root causes of conflict: crushing poverty. However, even as various stakeholders have attempted to restore normalcy in the state, they have done so without a comprehensive needs assessment to guide them. In an attempt to fill this gap, the Center for Diversity and National Harmony (CDNH) undertook the task of developing a source of baseline information on Rakhine State, which all stakeholders can draw on when providing humanitarian and development assistance as well as when working on conflict prevention in the state. -

General Assembly Distr.: General 5 August 2020
United Nations A/75/288 General Assembly Distr.: General 5 August 2020 Original: English Seventy-fifth session Item 72 (c) of the provisional agenda* Promotion and protection of human rights: human rights situations and reports of special rapporteurs and representatives Report on the implementation of the recommendations of the independent international fact-finding mission on Myanmar Note by the Secretary-General The Secretary-General has the honour to transmit to the General Assembly the report of the United Nations High Commissioner for Human Rights on the implementation of the recommendations of the independent international fact-finding mission on Myanmar and on progress in the situation of human rights in Myanmar, pursuant to Human Rights Council resolution 42/3. * A/75/150. 20-10469 (E) 240820 *2010469* A/75/288 Report of the United Nations High Commissioner for Human Rights on the situation of human rights in Myanmar Summary The independent international fact-finding mission on Myanmar issued two reports and four thematic papers. For the present report, the Office of the United Nations High Commissioner for Human Rights analysed 109 recommendations, grouped thematically on conflict and the protection of civilians; accountability; sexual and gender-based violence; fundamental freedoms; economic, social and cultural rights; institutional and legal reforms; and action by the United Nations system. 2/17 20-10469 A/75/288 I. Introduction 1. The present report is submitted pursuant to Human Rights Council resolution 42/3, in which the Council requested the United Nations High Commissioner for Human Rights to follow up on the implementation by the Government of Myanmar of the recommendations made by the independent international fact-finding mission on Myanmar, including those on accountability, and to continue to track progress in relation to human rights, including those of Rohingya Muslims and other minorities, in the country. -

September 2020 1
SEPTEMBER 2020 1 SEPTEMBER 2020 2 TABLE OF CONTENTS MONTH IN REVIEW 4 CHRONOLOGY 7 ● POLITICAL PRISONERS 7 ○ ARRESTS 7 ○ CHARGES 8 ○ SENTENCES 12 ○ RELEASES 13 ○ ARRESTS BY EAO 14 ○ RELEASES BY EAO 14 ○ DISAPPEARANCES 14 ● RESTRICTIONS ON CIVIL AND POLITICAL RIGHTS 14 ● REFERENCES 22 SEPTEMBER 2020 3 MONTH IN REVIEW Freedom of Speech and Expression September 15 was the UN International Democracy Day. Democracy is “a form of government in which the people have the authority to choose their governing legislation.” However, the values and standards of democracy have not yet been established in Burma and the people’s authority over their daily lives and fundamental rights is fading. It is clearly shown that Burma is deviating from the path of democracy as those who exercise their right to freedom of speech and expression which is a fundamental right in democratization, face not only oppression and restrictions but arbitrary detentions and arrests. This September, freedom of speech and expression became more severely restricted. A total of 34 students and members of student unions from Rangoon, Mandalay, Meiktila Monywa, Pakokku and Pyay Townships were charged under Section 19 of PAPPL or Section 505(a)(b) of the Penal Code or Section 25 of the Natural Disaster Management Law for staging protests in related to the conflict in Arakan. Among them, 23 students were formally arrested and one was sentenced. In addition to this, four civilians were arrested. Moreover, Sithu Aung a.k.a Saung Kha was fined under Section 19 of PAPPL for protesting to reinstate internet services in Arakan and Chin states. -

Rakhine Death Toll Hits 67 As Govt Defends Soldiers
E H T MYANMARTIMES October 29 - November 4, 2012 Myanmar’s first international weekly Volume 33, No. 650 1200 Kyats Averting the apocalypse: U Thant’s finest hour By Douglas Long WITH all the hype in recent months about Myanmar ending 50 years of isolation, it bears remembering that the secretary general of the United Nations from 1961 to 1971 was a top diplomat from Myanmar. It’s also worth noting that 50 years ago this month, this particular secretary general, U Thant, not only presided over the UN during the Cuban Missile Crisis — one the most dire international emergencies of the 20th century — but also played a key role in ensuring that the situation did not devolve into an apocalyptic frenzy of nuclear destruction. The crisis unfolded over 13 days in 1962, from October 16 to 28, after photos taken by U-2 spy plane pilot Richard Heyser alerted US president John F Kennedy to the presence of Soviet nuclear missiles in Cuba. This revelation led the US government to mull airstrikes on Cuba, but Mr Kennedy went against the advice of many Senate leaders and instead implemented a naval blockade. By October 24 the situation looked A man with a gunshot wound is treated at Kyauktaw Township Hospital in Rakhine State on October 25. Pic: Kaung Htet desperate: Reconnaissance photographs showed that the missiles in Cuba were in launch position and US and Soviet warships were engaged in a standoff, only a few hundred metres apart and pointing their weapons at one another. On the same day, the US military’s Rakhine death toll hits 67 five-level defense readiness condition (DEFCON) was advanced from Level 3 (increase in force readiness above normal readiness) to Level 2 (next step to nuclear war), still the highest in history. -

“Caged Without a Roof” Apartheid in Myanmar’S Rakhine State
“CAGED WITHOUT A ROOF” APARTHEID IN MYANMAR’S RAKHINE STATE Amnesty International is a global movement of more than 7 million people who campaign for a world where human rights are enjoyed by all. Our vision is for every person to enjoy all the rights enshrined in the Universal Declaration of Human Rights and other international human rights standards. We are independent of any government, political ideology, economic interest or religion and are funded mainly by our membership and public donations. © Amnesty International 2017 Except where otherwise noted, content in this document is licensed under a Creative Commons Cover photo: Rohingya children in a rural village in Buthidaung township, northern Rakhine State, (attribution, non-commercial, no derivatives, international 4.0) licence. March 2016. © Amnesty International. https://creativecommons.org/licenses/by-nc-nd/4.0/legalcode For more information please visit the permissions page on our website: www.amnesty.org Where material is attributed to a copyright owner other than Amnesty International this material is not subject to the Creative Commons licence. First published in 2017 by Amnesty International Ltd Peter Benenson House, 1 Easton Street London WC1X 0DW, UK Index: ASA 16/7436/2017 Original language: English amnesty.org CONTENTS TIMELINE OF KEY EVENTS 8 EXECUTIVE SUMMARY 10 METHODOLOGY 16 1. BACKGROUND 19 1.1 A HISTORY OF DISCRIMINATION AND PERSECUTION 20 1.2 THE 2012 VIOLENCE AND DISPLACEMENT 22 1.3 FURTHER VIOLENCE AND DISPLACEMENT: 2016 23 1.4 ARSA ATTACKS AND THE CAMPAIGN OF ETHNIC CLEANSING: 2017 24 1.5 THE POLITICAL CONTEXT 25 1.6 UNDERSTANDING ETHNIC RAKHINE GRIEVANCES 26 2. -

Situation of Human Rights of Rohingya Muslims and Other Minorities in Myanmar
A/HRC/45/5 Advance Edited Version Distr.: General 3 September 2020 Original: English Human Rights Council Forty-fifth session 14 September–2 October 2020 Agenda item 2 Annual report of the United Nations High Commissioner for Human Rights and reports of the Office of the High Commissioner and the Secretary-General Situation of human rights of Rohingya Muslims and other minorities in Myanmar Report of the Office of the United Nations High Commissioner for Human Rights* Summary The present report is submitted pursuant to Human Rights Council resolution 42/3, in which the Office of the United Nations High Commissioner for Human Rights (OHCHR) is requested to submit to the Council at its forty-fifth session a report on the implementation of the recommendations of the independent international fact-finding mission on Myanmar, including those on accountability, and on progress in the situation of human rights in Myanmar, including of Rohingya Muslims and other minorities. * The present report was submitted after the deadline so as to include the most recent information. A/HRC/45/5 I. Introduction 1. The present report is submitted pursuant to Human Rights Council resolution 42/3, in which the United Nations High Commissioner for Human Rights was requested to follow up on the implementation by the Government of Myanmar of the recommendations made by the independent international fact-finding mission, including those on accountability, and to continue to track progress in relation to human rights in Myanmar, including of Rohingya Muslims and other minorities. 2. The report was prepared on the basis of primary and secondary information collected from various sources – including primary witness testimonies, the Government, the United Nations, civil society organizations, representatives of ethnic and religious minority communities, diplomats, media professionals, academics and other experts. -
Draft Restricted
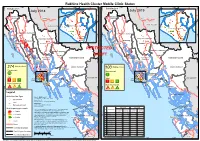
Rakhine Health Cluster Mobile Clinic Status N N N N ' ' ' ' 0 0 92°30'E 93°0'E 93°30'E 0 92°30'E 93°0'E 93°30'E 0 3 3 3 3 ° ° ° ° 1 1 Bangladesh 1 Bangladesh 1 2 2 July 2018 2 July 2019 2 MAUNGDAW MAUNGDAW TOWNSHIP Paletwa TOWNSHIP Paletwa CHIN STATE CHIN STATE SITTWE TOWNSHIP SITTWE TOWNSHIP BUTHIDAUNG TOWNSHIP N N N N ' ' ' BUTHIDAUNG TOWNSHIP ' 0 0 0 0 ° ° ° ° 1 1 1 1 2 2 2 2 KYAUKTAW TOWNSHIP KYAUKTAW TOWNSHIP Buthidaung Sittwe Buthidaung Sittwe Maungdaw Kyauktaw Maungdaw Kyauktaw RESTRICTED MRAUK-U TOWNSHIP MRAUK-U TOWNSHIP Mrauk-U DRAFT Mrauk-U RATHEDAUNG RATHEDAUNG PONNAGYUN PONNAGYUN TOWNSHIP RAKHINE STATE TOWNSHIP RAKHINE STATE N TOWNSHIP N N TOWNSHIP N ' ' ' ' 0 0 0 0 3 Rathedaung 3 3 Rathedaung 3 ° ° ° ° 0 0 0 0 2 2 2 2 Mobile clinics MINBYA TOWNSHIP Mobile clinics MINBYA TOWNSHIP Minbya 274 Ponnagyun Minbya 100 Ponnagyun Government Government 116 PAUKTAW PAUKTAW TOWNSHIP 1 TOWNSHIP Joint ANN TOWNSHIP SITTWE Joint SITTWE ANN TOWNSHIP Pauktaw Pauktaw TOWNSHIP TOWNSHIP 7 6 4 Sittwe Sittwe 1 4 5 Non Government Non Government N N N N ' Myebon ' ' Myebon ' 0 0 0 0 ° ° ° ° 0 81 39 12 0 0 0 2 2 2 54 21 8 2 Legend MYEBON TOWNSHIP MYEBON TOWNSHIP Clinic Provider Type Map ID: MIMU1546v04 Creation Date: 17 September 2019 Government Paper Size: A3 Joint Projection/Datum: Geographic/WGS84 Data Source: Non-Government Health Cluster (Rakhine State) Base map: MIMU Visit frequency per month July 2018 July 2019 Clinics not displayed in the maps because of missing geographic No Township Mobile Vistits/ Mobile Vistits/ < 4 visits coordinates: 9 locations in 2018 and 6 locations in 2019 N N N Clinics Month Clinics Month N ' Place Names: General Administration Department (GAD) and field ' ' ' 0 0 0 0 3 sources.Place names on this product are in line with the general 3 3 3 ° ° ° 1 Sittwe 92 404 56 328 ° 9 4 - 8 visits cartographic practice to reflect the names of such places as 9 9 9 1 KYAUKPYU TOWNSHIP 1 1 2 Buthidaung 64 85 6 8 KYAUKPYU TOWNSHIP 1 designated by the government concerned. -

Arakan (Rakhine State) a Land in Conflict on Myanmar’S Western Frontier AUTHOR: Martin Smith
Arakan (Rakhine State) A Land in Conflict on Myanmar’s Western Frontier AUTHOR: Martin Smith DESIGN: Guido Jelsma PHOTO CREDITS: Tom Kramer (TK) Martin Smith (MS) The Irrawaddy (IR) Agence France-Presse (AFP) European Pressphoto Agency (EPA) Mizzima (MZ) Reuters (RS) COVER PHOTO: Displaced Rakhine woman fetching water in IDP camp near Sittwe (TK) ACKNOWLEDGEMENTS: This publication was made possible through the financial support of Sweden. The contents of this publication are the sole responsibility of TNI and can under no circumstances be regarded as reflecting the position of the donor. PUBLICATION DETAILS: Contents of the report may be quoted or reproduced for non-commercial purposes, provided that the source of information is properly cited. ISBN 978-90-70563-69-1 TRANSNATIONAL INSTITUTE (TNI) De Wittenstraat 25, 1052 AK Amsterdam, The Netherlands Tel: +31-20-6626608, Fax: +31-20-6757176 e-mail: [email protected] www.tni.org/en/myanmar-in-focus Amsterdam, December 2019 2 | Arakan (Rakhine State): A Land in Conflict on Myanmar’s Western Frontier transnationalinstitute Table of Contents Myanmar Map 3 Arakan Political Timeline 4 Abbreviations 6 1. Introduction 8 Arakan Map 11 2. The Forgotten Kingdom of Arakan 12 A Legacy of Conflict and Colonisation 12 Rakhine State: A Contemporary Snapshot 15 British Rule and the Development of Nationalist Movements 17 Japanese Invasion and Inter-communal Violence 19 The Marginalisation of Arakan and Rush to Independence 21 Rakhine, Rohingya and the “Politics of Labelling” 25 3. The Parliamentary Era (1948-62) 28 A Country Goes Underground 28 Electoral Movements Revive 29 “Arms for Democracy”: Peace Breakthroughs and Political Failures 31 The Mayu Frontier Administration and Ne Win’s Seizure of Power 34 4. -

CAUGHT in the CROSSFIRE: Witness and Survivor Accounts of Burma Army Attacks and Human Rights Violations in Arakan State
CAUGHT IN THE CROSSFIRE: Witness and Survivor Accounts of Burma Army Attacks and Human Rights Violations in Arakan State WARNING: This report contains graphic photos Caught in the Crossfire At right: Photos of victims of a Burma Army attack in Arakan State on April 13, 2020. For more information on this particular airstrike, please see the photo on page 9. Caught in the Crossfire Free Burma Rangers About this Report This report is the result of 178 interviews conducted, recorded, and translated by Arakan members of the Free Burma Rangers (FBR). The Rangers conducted the interviews during 2019 and submitted the translations and corresponding videos and photos in June 2020. These interviews represent a fraction of the total incidences of Burma Army abuse that is being perpetrated on a grand scale in Arakan State. In March 2020, the Burmese government designated the Arakan Army as a terrorist organization. With this designation, locals fear that the Burmese soldiers will increase the use of torture and detention against civilians in Arakan State with total impunity. Acknowledgements FBR would like to acknowledge and thank the Arakan Rangers for their hard work and dedication in collecting these interviews regarding the ongoing conflict in Arakan State. This report would not be possible without their commitment to getting the news out. We are also grateful to the witnesses who shared their stories and without whose courage in coming forward this report would not have been possible. FBR continues to stand with the Arakan people and others under attack in northern Arakan State as well as Chin State where this particular conflict has spilled into. -
Burma Gazetteer Akyab District Volume a Compiled by Mr. Rb Smart
BURMA GAZETTEER AKYAB DISTRICT VOLUME A COMPILED BY MR. R. B. SMART (DY. COMMISSIONER), SETTLEMENT OFFICER, AKYAB SUPDT., GOVT. PRINTING AND STATY., UNION OF BURMA RANGOON LIST OF AGENTS FOR THE SALE OF THE GOVERNMENT OF THE UNION OF BURMA PUBLICATIONS IN BURMA 1. CITY BOOK CLUB. 98, Phayre Street, Rangoon. 2. U LU GALE Govt, Law Book Agent, 34th Road. Nyaungzindan Quarter, Mandalay. 3. MESSRS, K, BIN HOON & SONS. Nyaunglebin, Pegu District. 4. NEW LIGHT OF BURMA PRESS, 58, Komin Kochin Road, Rangoon. 5. PROPRIETOR, THU DHAMA WADI PRESS, 55-56, Tsee Kai Maung Khine Street, Rangoon. 6. PROPRIETOR, BURMA NEWS AGENCY. 135 Fraser Street, Rangoon. 7. MANAGER, BURMA BOOK CO.. 62. Barr Street. Rangoon. 8. BURMA EDUCATIONAL BOOK SHOP. 551-3, Merchant Street, Rangoon. 9. MANAGER, UNION PUBLISHING HOUSE. 20. Sule Pagoda Road, Rangoon 10. U KYAw ZAN, The National Book Depôt and Stationery Supply House, North Godown, Zegyo, Mandalay. IN INDIA 1. MESSRS, HIGGINBOTHAMS, LTD. Post Box No. 311, Madras. 2. MESSRS, THACKER, SPINK & Co, (1933), LTD., P.O. Box No. 54 3. Esplanade East, Calcutta (West Bengal), PREFACE THANKS are due to the many officials and others · who have supplied materials for the compilation of this Gazetteer and particularly to those mentioned below :- Mr. A. H. M. Barrington, Deputy Conservator of Forests, Arakan Division, for the Chapter on Forests and the paragraphs on the Flora of the district. Mr. W. S. Thom, Deputy Commissioner, Hill District of Arakan, for the paragraph on Fauna. Mr, Saw Chin Hin, B.A., Inspector of Schools, Arakan Circle, for the Chapter on Education. -
A Continuing Genocide
A continuing genocide Burmese Rohingya Organisation UK - Briefing May 2020 Myanmar’s failure to implement the International Court of Justice Provisional Measures Order Background to the ICJ’s provisional measures order Ongoing impunity in Myanmar On 11 November 2019, the Gambia filed an ‘Application The Independent Commission of Enquiry (ICOE) set up in Instituting Proceedings and Request for Provisional Measures’ 2018 by the Myanmar government was tasked to ‘investigate at the International Court of Justice (ICJ), the United Nations’ allegations of human rights violations and related issues following World Court, against Myanmar for alleged violations of its the terrorist attacks by the Arakan Rohingya Salvation Army obligations under the 1948 Convention on the Prevention and (ARSA) in Rakhine State with a view to seeking accountability’.5 Punishment of the Crime of Genocide (Genocide Convention). The ICOE published the 15-page Executive Summary of its The Gambia also included an urgent request for the Court to findings two days before the ICJ’s provisional measures order. order provisional measures in light of ‘the ongoing, severe and The ICOE concluded that, ‘war crimes, serious human rights irreparable harm being suffered by members of the Rohingya violations, and violations of domestic law took place during the g roup.’ 1 security operations... there are reasonable grounds to believe that members of Myanmar’s security forces were involved’. The ICOE On 23 January 2020, the ICJ issued a relatively rare unanimous, asserted that its -
Rathedaung Disclaimer: the Names Shown and the Boundaries Used on This Map Do Not Imply Official Endorsement Or Acceptance by the United Nations
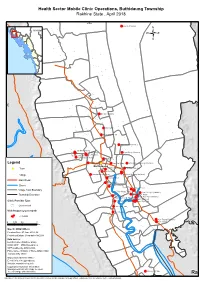
Health Sector Mobile Clinic Operations, Buthidaung Township Rakhine State , April 2018 92°30'E Laung Chaung MYANMAR 21°0'N 21°0'N Bo Gyi Chaung Maung Nu Dar Paing Sa Yar Pyin Shey (Rakhine) Tat Min Chaung Let Wea Det Pyin Shey (Musilm) Tat Min Chaung Let Wea Det Kyauk Hpyu Taung Ywar Ma Legend Thittaw Ywar Nan Yar Kone War Khoke Chaung (NaTaLa) Buthidaung Town Tat Yar (Rakhine) Da Pyu Chaung Mun Shi Ywar Village Gandamar (NaTaLa) Inn Gyin Myaing (NaTaLa) Ka Kyet Bet Main Road Myaung Nar Shore Ah Lel Chaung Done Thein Done Thein Village Tract Boundary Maungdaw Ah Twin Hnget Thay Tha Yet Pyin (Rakhine) Township Boundary Htan Shauk Khan Kin Chaung Kyar Nyo Pyin (Musilm) Hpon Nyo Leik (Musilm) Hpon Nyo Leik Clinic Provider Type Tha Peik Taung Hpon Nyo Leik Government Tha Pyay Taw Visit frequency per month Yet Chaung < 4 visits Kun Taung(Rakhine) 0 1.75 3.5 7 Kun Taung Km Map ID: MIMU1555v02 Creation Date: 07 June 2018, A4 Projection/Datum: Geographic/WGS84 Data Source: Health Cluster (Rakhine State) BASE MAP - MIMU;Boundaries - WFP,modified by MIMU 2008; Place name - Ministry of Home Affair (GAD) translated by MIMU Map produced by the MIMU - E-mail: [email protected] Website: www.themimu.info Copyright © Myanmar Information Management Unit 2018.May be used free of charge with attribution. Maung Hnit Ma 92°30'E Rathedaung Disclaimer: The names shown and the boundaries used on this map do not imply official endorsement or acceptance by the United Nations. Health Sector Mobile Clinic Operations, Kyaukpyu Township Rakhine State, April 2018 93°30'E