September 2015 – South East Expression of Interest for Wave One
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Progress Summary
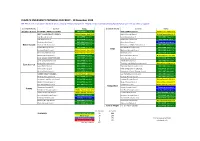
CLIMATE EMERGENCY PROGRESS CHECKLIST - 10 December 2019 NB. This is work in progress! We have almost certainly missed some actions. Please contact [email protected] with any news or updates. County/Authority Council Status County/Authority Council Status Brighton & Hove BRIGHTON & HOVE CITY COUNCIL DECLARED Dec 2018 KENT COUNTY COUNCIL Motion Passed May 2019 WEST SUSSEX COUNTY COUNCIL Motion Passed - April 2019 Ashford Borough Council Motion Passed July 2019 Adur Borough Council DECLARED July 2019 Canterbury City Council DECLARED July 2019 Arun District Council DECLARED Nov 2019 Dartford Borough Council DECLARED Oct 2019 Chichester City Council DECLARED June 2019 Dover District Council Campaign in progress West Sussex Chichester District Council DECLARED July 2019 Folkestone and Hythe District Council DECLARED July 2019 Crawley Borough Council DECLARED July 2019 Gravesham Borough Council DECLARED June 2019 Kent Horsham District Council Motion Passed - June 2019 Maidstone Borough Council DECLARED April 2019 Mid Sussex District Council Motion Passed - June 2019 Medway Council DECLARED April 2019 Worthing Borough Council DECLARED July 2019 Sevenoaks District Council Motion Passed - Nov 2019 EAST SUSSEX COUNTY COUNCIL DECLARED Oct 2019 Swale Borough Council DECLARED June 2019 Eastbourne Borough Council DECLARED July 2019 Thanet District Council DECLARED July 2019 Hastings Borough Council DECLARED Dec 2018 Tonbridge and Malling Borough Council Motion Passed July 2019 East Sussex Lewes District Council DECLARED July 2019 Tunbridge -

Local Government Boundary Commission for England Report No
Local Government Boundary Commission For England Report No. Principal Area Boundary Review Borough of Gravesham/Borough of Dartford/District of Sevenoaks LOCAL GOVEHNICWT BOUNDARY COMMISSION FOR ENGLAND HEK)hT NO. LOCAL GOVKRflUEJlT BOI'NJJAHY COMMISSION FOR CHAIRMAN Mr C J Ellerton CMC MB1C Mr J U Powell PRICE FGV* Lady Aoknur lir T Brockbank DI^ Professor G E Cherry Mr K J L Newell Me B Qcholee QBE THE RT. HON. PATRICK JENKIN MP SECRETARY OF STATE FOR THE ENVIRONMENT 1. At present the New Barn residential area is split between Dartford Borough, Sevenoaks District and Gravesham Borough; the part situated in Dartford is in the parish of ^outhfleet; the part in Sevenoaks is in the parish of Longfield, whilst the part in Gravesham is unparished. On 30 November 1979» Gravesham Borough Council requested ue to review the boundaries between the districts of Gravesham, Dartford and Sevenoaks in the vicinity of New Barn. Their request was in response to representations from the New Barn Ratepayers Association for the whole of the New Barn residential area to be incorporated within Gravesham Borough. The Association based their representations on a survey of opinion which they carried out in 1978 among the residents of New Barn on the question of whether the area should be under one authority, and if so, which one. The results indicated that a majority (8?#) of residents indicating a view preferred to see New Barn under one authority and a large proportion (6990 of these considered that this should be Gravesham. 2. We noted that Kent County Council, Dartford Borough Council, Sevenoaks District Council, and Longfield Parish Council were all opposed to a review beinp undertaken at that time, although Kent County Council and Dartford BOrough Council did a^ree that the current boundaries in the New Barn area were not wholly satisfactory. -

WELCOME to the LONDON TRAINING CENTER KEY FACTS 24/7 365 Days Operation Per Year
WELCOME TO THE LONDON TRAINING CENTER KEY FACTS 24/7 365 days operation per year WELCOME TO YOUR NEW HOME 8 7 Certified $100M+ FOR TRAINING. Level D Full State-of-the-art To CAA and EASA Investment in pilot Flight Simulators classrooms standards training The recently opened London Training Center, is a $100+ million investment focused on delivering the highest quality of pilot training in a purpose built state-of-the-art facility. We have prepared this welcome pack about the London Training Center in advance of your visit, so you can familiarize yourself with the facilities beforehand. To best prepared for your training. ABOUT L3HARRIS L3Harris are the global experts in providing a comprehensive range of training courses and support services, including training systems hardware and software for pilots and airlines. L3Harris delivers training matched to airline needs through a long history of successful relationships with global airlines. Our connected expertize enhances our ability to provide you with the very best pilot training. We have training centers close to major airports and a global network of academies, making training accessible for candidates and airlines. What’s more, we ensure training is truly reflective of the unique “Airlines rely on their pilots corporate cultures of our airline customers across the world. expertize - so the flexibility and Technology that takes you closer to reality Our training systems take tomorrow’s pilots and crew to near-reality, combining unrivaled simulated experiences with our in-depth knowledge of aircraft and the human behavior that governs them. From reactivity of our training is key to tablet-based tuition to Full Flight Simulators, we’re equipped to exceed training requirements. -

Housing Market Partnership for Hart District Council, Rushmoor Borough
Housing Market Partnership for the administrative areas of Hart, Rushmoor and Surrey Heath Terms of Reference (Version 3) Purpose 1. To ensure the Strategic Housing Land Availability Assessments are robust and credible in that they will deliver the core outputs and follow the process checklist as appended 2. To receive and consider reports from commissioned consultants (where appropriate) and feedback from the wider stakeholder group 3. To share and pool information and intelligence, including relevant contextual intelligence and policy information on housing land availability, housing market and financial data 4. To support core members in the analysis and interpretation of the assessment data 5. To consider the implications of the assessments, including signing off the assessment reports, core outputs and agreeing follow up action 6. To agree a process by which the SHLAA findings can be regularly reviewed Membership At its outset, the membership will comprise representatives from the following bodies: Hart District Council Rushmoor Borough Council Surrey Heath Borough Council Berkeley Homes Barton Willmore Mitchell and Partners Gregory Gray Associates Annington Property Ltd Barratt Southern Counties Mitchell and Partners Re-Format Architects Sentinel HA Accent Peerless First Wessex Housing Lovell Partnerships The Rund Partnership Rippon Development Services MGA Planning Rio Homes and Estates These are the organisations that attended either the first meeting, the second meeting, or both. Other key stakeholders1 can join the partnership should they wish to do so by contacting either Hart District Council, Rushmoor Borough Council, or Surrey Heath Borough Council. New members will be invited as necessary to ensure that the housing market area is represented with at least one house builder and preferably with other key stakeholders such as local property and planning agents, Registered Social Landlords and key landowners. -

Surrey Hotel Futures Report
SURREY HOTEL FUTURES FINAL REPORT Prepared for: Surrey County Council June 2015 Surrey Hotel Futures Study 2015 __________________________________________________________________________________________ CONTENTS EXECUTIVE SUMMARY .................................................................................................................................. i 1. INTRODUCTION ................................................................................................................................... 1 1.1. Study Background and Brief................................................................................................... 1 1.2. Scope of the Study ................................................................................................................... 2 1.3. Methodology ............................................................................................................................. 4 2. NATIONAL HOTEL TRENDS ................................................................................................................ 6 2.1. National Hotel Performance Trends ...................................................................................... 6 2.2. National Hotel Development Trends .................................................................................... 8 3. SURREY HOTEL SUPPLY ..................................................................................................................... 19 3.1. Current Surrey Hotel Supply ................................................................................................. -

Pharmaceutical Needs Assessment DGS
1 Kent Pharmaceutical Needs Assessment Dartford, Gravesend, Swanley and surrounding areas co-terminus with Dartford, Gravesham & Swanley CCG The accompanying maps etc. in Appendix A should be viewed alongside this document Kent PNA 2018- DGS CCG area Final version March 2018 2 Contents Introduction ...................................................................................................... 3 Transport Links ................................................................................................ 8 Pharmaceutical Services in the area ................................................................ 8 Healthy Living Pharmacies ............................................................................ 14 Housing .......................................................................................................... 15 Kent PNA 2015 – Dartford, Gravesham and Swanley area ........................... 16 Consultation ................................................................................................... 16 Conclusions and recommendations Kent PNA 2018 DGS area .................... 17 Document Version Control ............................................................................. 18 Kent PNA 2018- DGS CCG area Final version March 2018 3 Introduction This document has been written as part of the main Kent Pharmaceutical Needs Assessment (PNA) to allow judgements to be made using local data. This document should be read in conjunction with the main Kent PNA. The area consists of 3 main towns, Dartford, Gravesend -

LDF Thank You for the Opportunity to Comment. Surrey Heath Have No
LDF From: Jane Ireland <[email protected]> Sent: 13 April 2015 16:41 To: LDF Subject: RE: Publication of the Reigate & Banstead Community Infrastructure Levy Draft Charging Schedule Thank you for the opportunity to comment. Surrey Heath have no comments on the CIL charging schedule. Regards Jane Ireland Planning Policy and Support Manager Policy and Conservation Surrey Heath Borough Council Knoll Road Camberley GU15 3HD (01276 707213) www.surreyheath.gov.uk Great Place l Great Community l Great Future From: LDF [mailto:[email protected]] Sent: 13 April 2015 12:09 To: LDF Subject: Publication of the Reigate & Banstead Community Infrastructure Levy Draft Charging Schedule Dear Sir/Madam In accordance with Regulation 16 of the Community Infrastructure Levy Regulations 2010 (as amended), I am writing to inform you of publication of the Reigate and Banstead Infrastructure Levy (CIL) Draft Charging Schedule, and invite your comments on the document. A copy of the CIL Draft Charging Schedule and Statement of Representations Procedure are attached to this email. These documents are also available to view on the Council’s website at www.reigate- banstead.gov.uk/cil, along with a range of relevant evidence and supporting documentation. Documents are also available for inspection at the Town Hall in Reigate and hard copies of all documents are available on request from 01737 276178 or [email protected]. You are encouraged to respond using the standard response form which is also available to download or on request using the details above. Responses must be submitted to the Council by 5pm, Tuesday 26 May 2015: By email to: [email protected]; or By post to: Planning Policy Team, Reigate & Banstead Borough Council, Town Hall, Castlefield Road, Reigate, Surrey, RH2 0SH. -

21 Bus Time Schedule & Line Route
21 bus time schedule & line map 21 Crawley - Dorking - Leatherhead - Epsom View In Website Mode The 21 bus line (Crawley - Dorking - Leatherhead - Epsom) has 4 routes. For regular weekdays, their operation hours are: (1) Box Hill: 7:08 PM (2) Crawley: 6:51 AM - 5:15 PM (3) Epsom: 6:20 AM - 2:46 PM (4) Leatherhead: 5:30 PM Use the Moovit App to ƒnd the closest 21 bus station near you and ƒnd out when is the next 21 bus arriving. Direction: Box Hill 21 bus Time Schedule 19 stops Box Hill Route Timetable: VIEW LINE SCHEDULE Sunday Not Operational Monday 7:08 PM Leatherhead Railway Station (T) Station Approach, Leatherhead Tuesday 7:08 PM Leret Way, Leatherhead Wednesday 7:08 PM Leret Way, Leatherhead Thursday 7:08 PM The Crescent, Leatherhead Friday 7:08 PM Russell Court, Leatherhead Saturday Not Operational Highlands Road, Leatherhead Seeability, Leatherhead Lavender Close, Leatherhead 21 bus Info Clinton Road, Leatherhead Direction: Box Hill Stops: 19 Glenheadon Rise, Leatherhead Trip Duration: 27 min Line Summary: Leatherhead Railway Station (T), Tyrrells Wood, Leatherhead Leret Way, Leatherhead, The Crescent, Leatherhead, Highlands Road, Leatherhead, Seeability, Headley Court, Headley Leatherhead, Clinton Road, Leatherhead, Glenheadon Rise, Leatherhead, Tyrrells Wood, Hurst Lane, Headley Leatherhead, Headley Court, Headley, Hurst Lane, Headley, The Cock Inn, Headley, Broome Close, The Cock Inn, Headley Headley, Crossroads, Headley, Headley Common Road, Headley, Headley Common Road, Broome Close, Headley Pebblecombe, The Tree, Box Hill, -

Green Homes Grant Local Authority Delivery Phase 1 GDPR Privacy Notice
Green Homes Grant Local Authority Delivery Phase 1 GDPR Privacy Notice Privacy Notice This notice sets out how Woking Borough Council as the lead authority on behalf of the consortium of the following local authorities Elmbridge Borough Council, Epsom & Ewell Borough Council, Guildford Borough Council, Mole Valley District Council, Reigate & Banstead Borough Council, Spelthorne Borough Council, Surrey Heath Borough Council, Tandridge District Council Waverley Borough Council, Woking Borough Council and Surrey County Council will use your personal data, and your rights. It is made under Articles 13 and/or 14 of the General Data Protection Regulation (GDPR). This notice relates to data collected under the Green Jump Surrey scheme operated by Woking Borough Council and Action Surrey, which is funded by the Green Homes Grant Local Authority Delivery Scheme (GHG LAD) run by the Department for Business, Energy and Industrial Strategy. Action Surrey is an energy efficiency advice service established by Surrey local authorities and operated by ThamesWey Sustainable Communities, a company wholly owned by Woking Borough Council. YOUR DATA The data We will process the following personal data: Customers: - Address and details of property receiving the GHG LAD installation(s) - Details about the GHG LAD installation(s) installed at the property, including type, size and cost - Contact address (if not the property receiving the GHG LAD installation(s)) - Address and details of property offered, but not receiving, the GHG LAD installation(s) - Your -

Holiday Extra
From the M23 Junction 9 Brighton Crawley - 1 Follow the M23 overpass at Junction 9 and take the A23 Brighton A 3 Crawley 21 exit toward Airport 7 A2 - 2 Following signs to North Terminal go straight over M23 TO N Gatwick R LONGBRIDGELONGBRIDGE M25 JCt 7 E Gatwick the first roundabout ROUNDABOUTROUNDABOUT I G A E. Grinstead (A23) T D - 3 At the 2nd roundabout take the 4th exit signposted A E B R O R (M23) R S S A I G 3 A23 Crawley/Redhill D 5 2 H 9 CRO 3 T 2 Y O N M - 4 After joining the A23 Northbound, get into the right POVE Gatwick R 4 O hand lane A (A23) C D D H A R R L D - 5 At the roundabout take the 4th exit signposted A23 W O O AIRPORTAIRPORT WAYWAY ROUNDABOUTROUNDABOUT M23 Crawley/Brighton (you should now be travelling in the Junction 9a A 2 direction you have just come from) 3 1 NORTHNORTH 3 Crawley A I R - 6 Stay on the A23 southbound and go straight on at TERMINALTERMINAL P O R T W M23 D AY R the first roundabout Y E AIRPORTAIRPORT WAYWAY L 2 R ROUNDABOUTROUNDABOUT - 7 At the second roundabout take the 2nd exit for O M23 H EASTEAST Junction 9 Lowfield Heath/Charlwood RVP North Terminal Long Term NORTH - 8 After 200 yards take the 1st exit at the mini SSOUTHOUTH Air cargo Air Cargo Airport other areas TERMINALTERMINAL GATWICKGATWICK roundabout (Charlwood Road) 3 Redhill A23 North 2 AIPORTAIPORT - 9 Airparks is 1.5 miles ahead on the right hand side Terminal A LONDON GATWICK Crawley South From the M23 Junction 10 Airport RVP SOUTH D AIRPORT Other areas Redhill Terminal - 1 From the M23 overpass at Junction 10 take the exit proud to park your car General Aviation Terminal A Station A23 O R signposted Horsham (A2011) Airparks Gatwick N - 2 At the first roundabout take the 3rd exit signposted O Charlwood Road, Lowfield Heath T H A2011 Horsham (A23) Crawley, West Sussex, RH11 0QB Town Centre A23 3 G 3 I Horsham (A264) 2 - Next, you come to a roundabout with traffic lights. -

Gossops Green Neighbourhood Centre Draft Conservation Area Appraisal (February 2021) DRAFT
Gossops Green Neighbourhood Centre Draft Conservation Area Appraisal (February 2021) DRAFT crawley.gov.uk Contents Part 1. Introduction ................................................................................................................................. 2 Part 2. General Character, Location and Uses ........................................................................................ 4 Part 3. Historic Interest ........................................................................................................................... 6 Part 4. Architectural Interest and Built Form .......................................................................................... 7 Part 5. Locally Important Buildings ....................................................................................................... 10 Part 6. Spatial Analysis .......................................................................................................................... 13 Part 7. Streets and Open Space, Parks and Gardens, and Trees........................................................... 13 Part 8. Setting and Views ...................................................................................................................... 17 Part 9. Character Areas and zones ........................................................................................................ 24 Part 10. Assessment of Condition ......................................................................................................... 26 Part 11. Identifying -

Volunteer Opportunities Across Surrey
VOLUNTEER OPPORTUNITIES ACROSS SURREY: Age Concern Epsom and Ewell Visiting and Befriending service covering the following areas: KT4, KT6, KT9 KT17 – KT22 SM2 – SM3 Volunteer drivers also required Please contact Liz Hope, Volunteer Co-coordinator Call: 01372 732458 Email: [email protected] Surrey Heath Age Concern Visiting and Befriending service in the following areas: GU15 – GU20 Volunteers drivers also required Please contact Gill Gibson, Charity Manager Call: 01276 707585 Email: [email protected] Age Concern Merstham, Redhill and Reigate Visiting and Befriending service in the following areas: RH1 – RH2, RH6 Volunteer opportunities across Surrey 10/17 Volunteer drivers also required Please contact Sandy Featherstonhaugh, Business Manager Call: 01737 645636 Email: [email protected] Age Concern Banstead Visiting and Befriending service in the following areas: SM2 Call: 01737 352156 Email: [email protected] Age Concern Mole Valley Visiting and Befriending service in the following areas: RH4 – RH5 KT21 – KT23 Please contact: Julia Gallagher, Volunteer Co-ordinator Call: 01306 899104 or 07442 017169 Email: [email protected] Age Concern Woking Visiting and Befriending service in the following areas: GU21 – GU24 Call: 01483 770753 Email: [email protected] Volunteer opportunities across Surrey 10/17 Visiting Friends Visiting and Befriending service and Day Care Service in the following areas: GU21 – GU24 KT12 – KT14 Please contact: Sandra Smook, Manager Call: