HOUSE ...No. 2381
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

MARCH 19 Layout 1
Focus at MHA on Still no room Congresswoman Clark respect, integrity, sees value of loan repay compassion at the inn VIEWPOINTS: DITORIAL PROVIDER PROFILE: E : PAGE 5 PAGE 4 PAGE 3 Vol. 40 - No. 3 The Newspaper of the Providers’ Council March 2019 Roundtable Federal, state discussion policy work gone to pot in spotlight he Providers’ Council and Massa- Organizations need to chusetts Nonprofit Network sent Ta joint letter to Congressman update policies, train staff Richard Neal (D-Mass.), Chair of the he legalization of marijuana usage Joint Committee on Taxation, urging in Massachusetts – for both medic- the immediate repeal of the new income Tinal and recreational purposes – is tax on expenses incurred by nonprofits creating new challenges and questions for providing employee transportation for human services providers about use benefits, such as parking and transit by both employees and clients. passes. Together, the Council and MNN Nearly 40 people representing 27 represent nearly 1,000 nonprofit or- Providers’ Council member organizations ganizations throughout Massachusetts. attended an HR Roundtable on Mari- The new tax – officially Internal Rev- juana Legalization Policies and Proce- enue Code Section 512(a)(7) – is a part dures hosted by the Council on Feb. 20 of the sweeping tax code reform passed in Needham to discuss their challenges in 2017 and the first payments will be and learn about best practices. due in a matter of weeks. It imposes a A panel – including attorneys Jeffrey 21 percent tax on nonprofits offering Hirsch and Peter Moser from the law firm transportation-related benefits to em- Hirsch Roberts Weinstein LLP; Senior ployees. -

An Act to Promote Public Safety and Better Outcomes for Young Adults – S.825/H.3420
An Act to Promote Public Safety and Better Outcomes for Young Adults – S.825/H.3420 Lead Sponsors MASSACHUSETTS CURRENTLY SPENDS THE MOST MONEY ON Sen. Joseph Boncore (Winthrop) YOUNG ADULTS IN THE JUSTICE SYSTEM AND GETS THE Rep. James O'Day (West Boylston) Rep. Kay Khan (Newton) WORST OUTCOMES Co-Sponsors Shifting 18- to 20-year-olds into the juvenile system, where Rep. Ruth Balser (Newton) they must attend school and participate in rehabilitative Rep. Christine Barber (Somerville) programming, would lower recidivism. The young adult Sen. Michael Brady (Brockton) brain is still developing making them highly amenable to Rep. Mike Connolly (Cambridge) rehabilitation. This development is influenced – Sen. Brendan Crighton (Lynn) positively or negatively – by their environment. Rep. Daniel Cullinane (Dorchester) Sen. Julian Cyr (Truro) An overly punitive approach can actually cause more Rep. Marjorie Decker (Cambridge) Rep. Marcos Devers (Lawrence) offending: Most young people "age out" of offending by their Sen. Sal DiDomenico (Everett) mid-twenties, particularly with developmentally appropriate Rep. Daniel Donahue (Worcester) interventions. Exposure to toxic environments, like adult jails Rep. Carolyn Dykema (Holliston) and prisons, entrenches young people in problematic Sen. James Eldridge (Acton) behaviors, increasing probability of recidivism. Rep. Tricia Farley-Bouvier (Pittsfield) Sen. Cindy Friedman (Arlington) Recidivism among young people incarcerated in the adult Rep. Sean Garballey (Arlington) corrections is more than double similar youth released Rep. Carlos González (Springfield) from department of youth services commitment Rep. Tami Gouveia (Acton) Teens and young adults incarcerated in Massachusetts’ adult Rep. Jim Hawkins (Attleboro) correctional facilities have a 55% re-conviction rate, Rep. Stephan Hay (Fitchburg) compared to a similar profile of teens whose re-conviction Rep. -

Name Office Sought District
The candidates listed below have taken the Commonwealth Environmental Pledge. Name Office Sought District Gerly Adrien State Representative 28th Middlesex Representative Ruth B Balser State Representative 12th Middlesex Bryan P Barash Newton City Council Ward 2 Representative Christine P Barber State Representative 34th Middlesex Alex Bezanson State Representative 7th Plymouth 2nd Suffolk and Senator Will Brownsberger State Senate Middlesex Suezanne Patrice Bruce State Representative 9th Suffolk Michelle Ciccolo State Representative 15th Middlesex Matthew Cohen State Representative 15th Middlesex Hampshire, Franklin Jo Comerford State Senate and Worcester Representative Dan Cullinane State Representative 12th Suffolk Paul Cusack State Representative 2nd Barnstable Senator Julian Cyr State Senate Cape and Islands Representative Michael Day State Representative 31st Middlesex Representative Diana DiZoglio State Senate 1st Essex Christina Eckert State Representative 2nd Essex Representative Lori A. Ehrlich State Representative 8th Essex Middlesex and Senator James Eldridge State Senate Worcester Senator Paul Feeney State Senate Bristol and Norfolk Barnstable, Dukes and Representative Dylan Fernandes State Representative Nantucket 2nd Essex and Barry Finegold State Senate Middlesex Senator Cindy F. Friedman State Senate 4th Middlesex Representative Sean Garballey State Representative 23rd Middlesex Representative Carmine Lawrence Gentile State Representative 13th Middlesex 15 Court Square, Suite 1000, Boston, MA 02108 • (617) 742-0474 • www.elmaction.org Allison Gustavson State Representative 4th Essex Representative Solomon Goldstein-Rose State Representative 3rd Hampshire Tami Gouveia State Representative 14th Middlesex Representative Jim Hawkins State Representative 2nd Bristol Sabrina Heisey State Representative 36th Middlesex Sarah G. Hewins State Representative 2nd Plymouth Representative Natalie Higgins State Representative 4th Worcester Kevin Higgins State Representative 7th Plymouth John Hine State Representative 2nd Hampshire Senator Patricia D. -

HOUSE ...No. 2827
HOUSE DOCKET, NO. 1932 FILED ON: 1/17/2019 HOUSE . No. 2827 The Commonwealth of Massachusetts _________________ PRESENTED BY: Edward F. Coppinger _________________ To the Honorable Senate and House of Representatives of the Commonwealth of Massachusetts in General Court assembled: The undersigned legislators and/or citizens respectfully petition for the adoption of the accompanying bill: An Act relative to transparency in private utility construction contracts. _______________ PETITION OF: NAME: DISTRICT/ADDRESS: Edward F. Coppinger 10th Suffolk Louis L. Kafka 8th Norfolk Steven Ultrino 33rd Middlesex Frank A. Moran 17th Essex Timothy R. Whelan 1st Barnstable Angelo J. Puppolo, Jr. 12th Hampden Brian W. Murray 10th Worcester Richard M. Haggerty 30th Middlesex Daniel Cahill 10th Essex José F. Tosado 9th Hampden David Paul Linsky 5th Middlesex Tommy Vitolo 15th Norfolk Joseph W. McGonagle, Jr. 28th Middlesex Tackey Chan 2nd Norfolk Mike Connolly 26th Middlesex Daniel J. Ryan 2nd Suffolk James B. Eldridge Middlesex and Worcester Stephan Hay 3rd Worcester 1 of 5 David M. Rogers 24th Middlesex Alice Hanlon Peisch 14th Norfolk Christopher Hendricks 11th Bristol Angelo M. Scaccia 14th Suffolk Smitty Pignatelli 4th Berkshire Thomas P. Walsh 12th Essex Daniel M. Donahue 16th Worcester Rady Mom 18th Middlesex Mathew J. Muratore 1st Plymouth Danielle W. Gregoire 4th Middlesex Carmine Lawrence Gentile 13th Middlesex Marc T. Lombardo 22nd Middlesex David F. DeCoste 5th Plymouth Bruce E. Tarr First Essex and Middlesex Bud L. Williams 11th Hampden Natalie M. Higgins 4th Worcester Mary S. Keefe 15th Worcester Joseph F. Wagner 8th Hampden Denise C. Garlick 13th Norfolk Antonio F. D. Cabral 13th Bristol Kimberly N. -

100% Renewable Energy Agenda 2019-2020 Legislative Session
! The 100% Renewable Energy Agenda 2019-2020 Legislative Session The 100% Renewable Energy Act Repower Massachusetts with 100 percent renewable electricity by 2035 and 100 percent renewable energy economy-wide (including heating and transportation) by 2045. • HD 3092: Rep. Marjorie Decker, Rep. Sean Garballey An Act re-powering Massachusetts with 100 percent renewable energy • SD 1625: Sen. Jamie Eldridge An Act transitioning Massachusetts to 100 per cent renewable energy Renewable electricity Community Empowerment An Act for community empowerment: Allow 25% solar power by 2030 cities and towns to support renewable en- An Act relative to solar power and the green ergy projects, like solar and offshore wind, economy: Eliminate caps on solar net me- by leveraging the buying power of their res- tering and increase the renewable portfolio idents. standard by 3 percent per year. • HD 3717: Rep. Dylan Fernandes • HD 2529: Rep. Paul Mark • SD 2098: Sen. Julian Cyr • SD 1376: Sen. Jamie Eldridge Clean Energy Future Act Solar roofs for new homes and businesses An Act to secure a clean energy future: In- An Act increasing solar rooftop energy: Re- crease solar, offshore wind, energy storage, quire solar panels to be installed on new and electric vehicles to get closer to zero residential and commercial buildings. carbon emissions by 2050. • HD 2890: Rep. Mike Connolly, Rep. Jack • HD 1248: Rep. Ruth Balser Lewis • SD 757: Sen. Marc Pacheco • SD 1532: Sen. Jamie Eldridge Contact: Ben Hellerstein, [email protected], 617-747-4368 Efficient buildings and appliances Clean transportation Net zero building code All-electric buses by 2035 An Act to establish a net zero stretch energy An Act transitioning Massachusetts to electric code: Allow cities and towns to adopt a buses: Require all transit buses and school stronger building code for highly efficient, buses to be clean electric vehicles by 2035. -

SNAP Gap Cosponsors - H.1173/S.678 91 Representatives & 28 Senators
SNAP Gap Cosponsors - H.1173/S.678 91 Representatives & 28 Senators Rep. Jay Livingstone (Sponsor) Representative Daniel Cahill Representative Jack Patrick Lewis Senator Sal DiDomenico (Sponsor) Representative Peter Capano Representative David Linsky Senator Michael Barrett Representative Daniel Carey Representative Adrian Madaro Senator Joseph Boncore Representative Gerard Cassidy Representative John Mahoney Senator William Brownsberger Representative Michelle Ciccolo Representative Elizabeth Malia Senator Harriette Chandler Representative Mike Connolly Representative Paul Mark Senator Sonia Chang-Diaz Representative Edward Coppinger Representative Joseph McGonagle Senator Jo Comerford Representative Daniel Cullinane Representative Paul McMurtry Senator Nick Collins Representative Michael Day Representative Christina Minicucci Senator Brendan Crighton Representative Marjorie Decker Representative Liz Miranda Senator Julian Cyr Representative David DeCoste Representative Rady Mom Senator Diana DiZoglio Representative Mindy Domb Representative Frank Moran Senator James Eldridge Representative Daniel Donahue Representative Brian Murray Senator Ryan Fattman Representative Michelle DuBois Representative Harold Naughton Senator Paul Feeney Representative Carolyn Dykema Representative Tram Nguyen Senator Cindy Friedman Representative Lori Ehrlich Representative James O'Day Senator Anne Gobi Representative Nika Elugardo Representative Alice Peisch Senator Adam Hinds Representative Tricia Farley-Bouvier Representative Smitty Pignatelli Senator -

METCO Legislators 2020
Phone (617) Address for newly District Senator/Representative First Name Last Name 722- Room # Email elected legislators Boston Representative Aaron Michlewitz 2220 Room 254 [email protected] Boston Representative Adrian Madaro 2263 Room 473-B [email protected] Natick, Weston, Wellesley Representative Alice Hanlon Peisch 2070 Room 473-G [email protected] East Longmeadow, Springfield, Wilbraham Representative Angelo Puppolo 2006 Room 122 [email protected] Boston Representative Rob Consalvo [email protected] NEW MEMBER Needham, Wellesley, Natick, Wayland Senator Becca Rausch 1555 Room 419 [email protected] Reading, North Reading, Lynnfield, Middleton Representative Bradley H. Jones Jr. 2100 Room 124 [email protected] Lynn, Marblehead, Nahant, Saugus, Swampscott, and Melrose Senator Adam Gomez [email protected] NEW MEMBER Longmeadow, Hampden, Monson Representative Brian Ashe 2430 Room 236 [email protected] Springfield Representative Bud Williams 2140 Room 22 [email protected] Springfield Representative Carlos Gonzales 2080 Room 26 [email protected] Sudbury and Wayland, Representative Carmine Gentile 2810 Room 167 [email protected] Boston Representative Chynah Tyler 2130 Room 130 [email protected] Woburn, Arlington, Lexington, Billerica, Burlington, Lexington Senator Cindy Friedman 1432 Room 413-D [email protected] Boston Senator Nick Collins 1150 Room 410 [email protected] Newton, Brookline, Wellesley Senator Cynthia Stone Creem 1639 Room 312-A [email protected] Boston, Milton Representative Dan Cullinane 2020 Room 527-A [email protected] Boston, Milton Representative Fluker Oakley Brandy [email protected] Boston, Chelsea Representative Daniel Ryan 2060 Room 33 [email protected] Boston Representative Daniel J. -

October 30, 2020 Secretary Stephanie Pollack Jeffrey Mcewen
October 30, 2020 Secretary Stephanie Pollack Jeffrey McEwen Massachusetts Department of Transportation Federal Highway Administration 10 Park Plaza, Suite 4160 55 Broadway, 10th Floor Boston, MA 02116 Cambridge, MA 02142 [email protected] [email protected] Dear Secretary Pollack and Administrator McEwen, Over the past six years all of us have welcomed the opportunity to comment on MassDOT’s designs to the I-90 Allston Interchange/Allston Multimodal Project. We also understand this project is a transformative, once-in-a-generation project. As elected officials representing communities directly abutting this project and elected officials whose constituents will be severely affected by this project, we are all in agreement that of the three proposals that are under consideration of NEPA submission the Modified All At-Grade Proposal is the only plan that should move forward in this process. Our constituents span from Boston to Worcester and beyond, and the Modified All At-Grade Proposal is the least disruptive to commuter rail riders and allows for the most lanes to be in use on the Mass Pike during construction. For commuter rail riders, the Modified All At-Grade Proposal lays the foundation for a transformative transportation network expanding transit from MetroWest communities. Likewise, for drivers, the Modified All At-Grade Proposal provides the most safe, straight, and flat highway. We feel that at this critical moment for the future of this project, it is important for us to express our utmost desire for MassDOT to pick the Modified All At-Grade Proposal as the preferred alternative. Despite some competing interests from various large institutions and economic sectors, the Modified All At-Grade Proposal has garnered the most widespread support because of its transformative impacts for generations to come. -
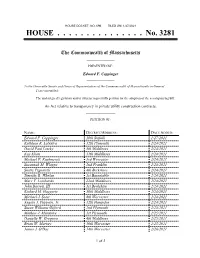
HOUSE ...No. 3281
HOUSE DOCKET, NO. 696 FILED ON: 1/27/2021 HOUSE . No. 3281 The Commonwealth of Massachusetts _________________ PRESENTED BY: Edward F. Coppinger _________________ To the Honorable Senate and House of Representatives of the Commonwealth of Massachusetts in General Court assembled: The undersigned legislators and/or citizens respectfully petition for the adoption of the accompanying bill: An Act relative to transparency in private utility construction contracts. _______________ PETITION OF: NAME: DISTRICT/ADDRESS: DATE ADDED: Edward F. Coppinger 10th Suffolk 1/27/2021 Kathleen R. LaNatra 12th Plymouth 2/24/2021 David Paul Linsky 5th Middlesex 2/24/2021 Kay Khan 11th Middlesex 2/24/2021 Michael P. Kushmerek 3rd Worcester 2/24/2021 Susannah M. Whipps 2nd Franklin 2/24/2021 Smitty Pignatelli 4th Berkshire 2/24/2021 Timothy R. Whelan 1st Barnstable 2/24/2021 Marc T. Lombardo 22nd Middlesex 2/24/2021 John Barrett, III 1st Berkshire 2/24/2021 Richard M. Haggerty 30th Middlesex 2/24/2021 Michael J. Soter 8th Worcester 2/24/2021 Angelo J. Puppolo, Jr. 12th Hampden 2/24/2021 Susan Williams Gifford 2nd Plymouth 2/25/2021 Mathew J. Muratore 1st Plymouth 2/25/2021 Danielle W. Gregoire 4th Middlesex 2/25/2021 Brian W. Murray 10th Worcester 2/25/2021 James J. O'Day 14th Worcester 2/26/2021 1 of 2 Peter Capano 11th Essex 2/26/2021 Lindsay N. Sabadosa 1st Hampshire 2/26/2021 Christopher Hendricks 11th Bristol 2/26/2021 Jessica Ann Giannino 16th Suffolk 2/26/2021 Diana DiZoglio First Essex 2/26/2021 Michael S. Day 31st Middlesex 2/26/2021 James M. -

January 28, 2021 the Honorable Charles D. Baker Office of The
January 28, 2021 The Honorable Charles D. Baker Office of the Governor Massachusetts State House Boston, MA 02133 Dear Governor Baker: We write to you to express our concern regarding the current process available to the public to sign up for COVID-19 vaccines. Our constituencies have called on us for assistance in navigating the pathway laid out by your Administration. The system in use, while made to be expedient and accessible, has created barriers for our aging population, those who have limited access to technology, and those who struggle to use it. Inadvertently, restricting the sign up process to a digital format puts our senior population at risk. In searching for the official online tool, the query also provides results not affiliated with the Commonwealth. This makes residents vulnerable to scams, and exposes them to undue online risks. Collectively, we implore the Administration to create a user friendly 1-800 number which would allow Massachusetts residents to access the sign up process more easily. Additionally, we request that the Administration create a centralized system, under the COVID-19 Task Force, that would allow for a more accessible sign-up process for those who can utilize the online tools. Currently, residents must choose a location, and then follow one of many links to separate entities to book appointments. We are appreciative for the steps that the Administration has taken, and are grateful for your consideration. Please contact our offices should you have questions, concerns, or wish to discuss this further. Sincerely, Anne M. Gobi Adam Gomez State Senator State Senator Worcester, Hampden, Hampshire Middlesex District Hampden District Eric P. -

MASC Legislative Directory 2020
2020 Massachusetts State Legislative Directory Massachusetts Constitutional Officers Governor Charlie Baker (617) 725-4005 Room 280 Lt. Governor Karyn Polito (617) 725-4005 Room 360 Treasurer Deborah Goldberg (617) 367-6900 Room 227 Atty. General Maura Healey (617) 727-2200 1 Ashburton Place, 18th Floor [email protected] Sec. of the State William Galvin (617) 727-9180 Room 340 [email protected] State Auditor Suzanne Bump (617) 727-2075 Room 230 [email protected] Massachusetts Senate (617) 722- Email (@masenate.gov) Room # (617) 722- Email (@masenate.gov) Room # Michael Barrett 1572 Mike.Barrett 109-D Patricia Jehlen 1578 Patricia.Jehlen 424 Joseph Boncore 1634 Joseph.Boncore 112 John Keenan 1494 John.Keenan 413-F Michael Brady 1200 Michael.Brady 416-A Edward Kennedy 1630 Edward.Kennedy 70 William Brownsberger 1280 William.Brownsberger 319 Eric Lesser 1291 Eric.Lesser 410 Harriette Chandler 1544 Harriette.Chandler 333 Jason Lewis 1206 Jason.Lewis 511-B Sonia Chang-Diaz 1673 Sonia.Chang-Diaz 111 Joan Lovely 1410 Joan.Lovely 413-A Nick Collins 1150 Nick.Collins 312-D Mark Montigny 1440 Mark.Montigny 312-C Joanne Comerford 1532 Jo.Comerford 413-C Michael Moore 1485 Michael.Moore 109-B Cynthia Creem 1639 Cynthia.Creem 312-A Patrick O'Connor 1646 Patrick.OConnor 419 Brendan Crighton 1350 Brendan.Crighton 520 Marc Pacheco 1551 Marc.Pacheco 312-B Julian Cyr 1570 Julian.Cyr 309 Rebecca Rausch 1555 Becca.Rausch 218 Sal DiDomenico 1650 Sal.DiDomenico 208 Michael Rodrigues 1114 Michael.Rodrigues 212 Diana DiZoglio 1604 Diana.DiZoglio 416-B -

2019 04 10 Schools Subcommittee Report WA
Article 28 – Resolution in Support of Changing the Flag and Seal of the Commonwealth School Subcommittee Recommendation to the Advisory Committee April 23, 2019 On April 10, 2019 at 6:30 PM, the School Subcommittee held a public hearing in Room 308 on Article 28. Subcommittee members – Dennis Doughty, Bobbie Knable, David Lescohier and Michael Sandman heard from the petitioner, Cornelia Van Der Ziel (TMM 16) and from one member of the public, Patricia Connor, former TMM 3 and former Brookline resident. SUMMARY Article 28 supports the adoption of legislation filed by State Senator Jason Lewis (5th Middlesex), State Reps. Nika Elugardo (Jamaica Plain & Brookline) and Lindsay Sabadosa Hatfield/Northampton), and co-sponsored by Rep. Tommy Vitolo (Brookline), among others. The legislation calls for the appointment of a commission to study whether to change the state flag and seal. The commission would be appointed: (1) for the purpose of investigating the features of the official seal and motto of the Commonwealth including those which potentially have been unwittingly harmful to or misunderstood by the citizens of the Commonwealth and (2) for the purpose of examining the seal and motto of the Commonwealth to ensure that they faithfully reflect and embody the historic and contemporary commitments of the commonwealth to peace, justice, liberty and equality and to spreading the opportunities and advantages of education. The commission would be comprised by a broadly representative group including: …the Executive Director of the Commission on