Wajir South Sub County, Kenya
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Kenya Interagency Rapid Assessment Wajir County August
KENYA INTER AGENCY RAPID ASSESSMENT WAJIR COUNTY CONFLICT ASSESSMENT REPORT August 8 – August 25, 2014 Figure 1: Photo taken by KIRA Assessment Team in Gulani village, Wajir County KIRA – Wajir assessment – August 2014 1 1. OVERVIEW OF THE SITUATION AND CRISIS a. Background of the situation Wajir County is divided into 8 districts namely; Wajir East, Tarbaj, Wajir South, Habaswein, Wajir West, Eldas, Buna and Wajir North districts .There are 6 Sub – counties/constituencies currently that is, Tarbaj, Wajir East, Wajir South, Wajir West, Eldas and Wajir North. The current inter-ethnic clashes between the Degodia and Garre communities along Border areas of Mandera and Wajir began on May 13, 2014. There has been an escalation and repeated attacks in Gunana location in Tarbaj Sub – county at the border of the two counties that is in May and June, 2014 and many people were killed in the conflict. This had spillover effects in the entire Wajir County. The inter clan clashes between Garre and Degodia communities along the Wajir – Mandera Border has directly affected 10 locations in Tarbaj District namely; Lehely, Bojigaras, El Kutulo, Mansa, Burmayo, Ogoralle, Berjanai, Dunto, Basaneja and Gunana, as well as Batalu, Danaba, Gulani, Belowle, Bosicha and Ajawa in Wajir North. Similarly, Wagberi in Wajir Central in Wajir East Sub – County has been affected where many houses were torched and vandalized leading to displacement of residents to in El Ado in Wajir South Sub – county and Hodhan in Wajir East with many others displaced into Mandera County. The clashes in Wajir County further affected other areas that are hosting an influx of displaced persons which include Sarman, Elben, Tarbaj and Kutulo in Tarbaj Sub - county, and Waradey in Eldas Sub - county, and Batalu, Danaba, Quadama and Gulani in Wajir North Sub - county. -

North Eastern Province (PRE) Trunk Roads ABC Road Description
NORTH EASTERN PROVINCE North Eastern Province (PRE) Trunk Roads ABC Road Description Budget Box culvert on Rhamu-Mandera B9 6,000,000 A3 (DB Tana River) Garissa - Dadaab - (NB Somali) Nr Liboi 14,018,446 C81 (A3) Modika - (B9) Modogashe 24,187,599 B9 (DB Wajir East) Kutulo - Elwak - Rhamu - (NB Somali) Mandera 11,682,038 Regional Manager Operations of office 4,058,989 Regional Manager RM of Class ABC unpaved structures 725,628 B9 (DB Lagdera) Habaswein - Wajir - (DB Mandera East) Kutulo 31,056,036 C80 (DB Moyale) Korondile - (B9) Wajir 29,803,573 A3 (DB Mwingi) Kalanga Corner- (DB Garissa) Tana River 16,915,640 A3 (DB Mwingi) Kalanga Corner- (DB Garissa) Tana River 90,296,144 North Eastern (PRE) total 228,744,093 GARISSA DISTRICT Trunk Roads ABC Road Description Budget (DB Garissa) Tana River- Garissa Town 21,000,000 Sub Total 21,000,000 District Roads DRE Garissa District E861 WARABLE-A3-D586 2,250,000.00 R0000 Admin/Gen.exp 302,400.00 URP26 D586(OHIO)-BLOCK 4,995,000.00 Total . forDRE Garissa District 7,547,400.00 Constituency Roads Garissa DRC HQ R0000 Administration/General Exp. 1,530,000.00 Total for Garissa DRC HQ 1,530,000.00 Dujis Const D586 JC81-DB Lagdera 1,776,000.00 E857 SAKA / JUNCTION D586 540,000.00 E858 E861(SANKURI)-C81(NUNO) 300,000.00 E861 WARABLE-A3-D586 9,782,000.00 URP1 A3-DB Fafi 256,000.00 URP23 C81(FUNGICH)-BALIGE 240,000.00 URP24 Labahlo-Jarjara 720,000.00 URP25 kASHA-D586(Ohio)-Dujis 480,000.00 URP26 D586(Ohio)-Block 960,000.00 URP3 C81-ABDI SAMMIT 360,000.00 URP4 MBALAMBALA-NDANYERE 1,056,000.00 Total for Dujis Const 16,470,000.00 Urban Roads Garissa Mun. -

Winning Hearts and Minds? Examining the Relationship Between Aid and Security in Kenya Mark Bradbury and Michael Kleinman ©2010 Feinstein International Center
A PR I L 2 0 1 0 Strengthening the humanity and dignity of people in crisis through knowledge and practice Winning Hearts and Minds? Examining the Relationship Between Aid and Security in Kenya Mark Bradbury and Michael Kleinman ©2010 Feinstein International Center. All Rights Reserved. Fair use of this copyrighted material includes its use for non-commercial educational purposes, such as teaching, scholarship, research, criticism, commentary, and news reporting. Unless otherwise noted, those who wish to reproduce text and image files from this publication for such uses may do so without the Feinstein International Center’s express permission. However, all commercial use of this material and/or reproduction that alters its meaning or intent, without the express permission of the Feinstein International Center, is prohibited. Feinstein International Center Tufts University 200 Boston Ave., Suite 4800 Medford, MA 02155 USA tel: +1 617.627.3423 fax: +1 617.627.3428 fic.tufts.edu Acknowledgements The report has been written by Mark Bradbury and Michael Kleinman, who take responsibility for its contents and conclusions. We wish to thank our co-researchers Halima Shuria, Hussein A. Mahmoud, and Amina Soud for their substantive contribution to the research process. Andrew Catley, Lynn Carter, and Jan Bachmann provided insightful comments on a draft of the report. Dawn Stallard’s editorial skills made the report more readable. For reasons of confidentiality, the names of some individuals interviewed during the course of the research have been withheld. We wish to acknowledge and thank all of those who gave their time to be interviewed for the study. -

Hydrogeological Assessment of the Merti Aquifer, Kenya
Hydrogeological Assessment of the Merti Aquifer, Kenya Technical report no 1 of ARIGA. Assessing Risks of Investment in Groundwater Development in Sub-Saharan Africa Summary The Government of Kenya has approached the Dutch investment company ORIO to support the investment in infrastructure for the Habaswein-Wajir Water Supply project. The project proposes to draw water from the Merti Aquifer to supply the city of Wajir with drinking water, through a 120 km pipeline. The proposed well-field is located near Habaswein and will be used for urban water supply for Habaswein as well. This documents reports the outcomes of a hydrogeological assessment that determines the risk of groundwater depletion as a result of the proposed well- field. It is a technical report published in the framework of ARIGA - Assessing Risks of Investment in Groundwater Development in Sub-Saharan Africa. The principles of Applied Information Economics are used to develop a decision model for the water supply intervention. The results of the hydrogeological study are used in that decision model. The hydrogeological study aims to predict the effect of the pipeline project on the groundwater system, while also stating the uncertainty in the predictions. This study focusses on the prediction of drawdown of groundwater levels, ultimately leading to boreholes falling dry, and deteriorating water quality as a result of displacement of saline water in the aquifer in a 30 year time period. Process-based models, that conceptualize the physical processes in the groundwater system, are combined with stochastic methods. This approach provides the probabilistic characteristics of the model outcomes to support decision-making. -

I Exploring the Management of Inter-Clan Conflict By
EXPLORING THE MANAGEMENT OF INTER-CLAN CONFLICT BY NON- GOVERNMENTAL ORGANISATIONS IN WAJIR COUNTY, KENYA BY MOHAMED SHEIKH NOOR SUBMITTED IN PARTIAL FULFILMENT OF THE REQUIREMENTS FOR THE DEGREE OF MASTERS IN CONFLICT TRANSFORMATION AND MANAGEMENT AT THE NELSON MANDELA METROPOLITAN UNIVERSITY SUPERVISOR: DR. GAVIN BRADSHAW I DECLARATION Full Name: Mohamed Sheikh Noor Student Number: 208090554 Qualification: MPHIL Conflict transformation and Management REC-H Ethics Clearance Ref No: H/12/ART/PGS-001 DECLARATION In accordance with Rule G4.6.3, I hereby declare that the above-mentioned treatise is my own work and that it has not previously been submitted for assessment to another University or for another qualification. SIGNED ………………………… DATE…………DECEMBER 2012… II ACKNOWLEDGEMENTS I am deeply indebted to the people who have been instrumental to the success of this study. I would like to thank my Supervisor Dr. Gavin Bradshaw for the guidance, without which this treatise could not have been possible. Thanks to Mr. Sultan M. Ali, a friend and a brother in NMMU who was instrumental in this study. I sincerely thank my dear mother, Maryan (Arisha) Sheikh Mohamud, Brother Omar Sheikh Noor and Spouse Johara Adan for their support towards my studies and their continued encouragement not limited to the production of this treatise. I would also thank all individuals who have participated in the Research, particularly Elder Muhumed Hassan Mumin (Dukow), the Chairman of Al-Fatah Peace Elders, the Wajir South Development Association and the Arid lands Development Focus, Wajir Human Rights Network, the Women for Peace and most notably the Wajir Peace and Development Committee. -
Kenya Program Maps
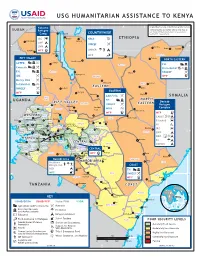
USG HUMANITARIAN ASSISTANCE TO KENYA 35°Kakuma 36° 37° 38° 39° 40°Original Map Courtesy 41° of the UN Cartographic Section 42° SUDAN The boundaries and names used on this map do Refugee not imply official endorsement or acceptance Camp Todenyang COUNTRYWIDE by the U.S. Government. IRC Banya KRCS a ETHIOPIA Lokichokio D Sabarei LWF 4° UNICEF F 4° LWR Banissa Ramu UNHCR Mandera Kakuma WFP Lokwa G Kangole WFP y Mandera Moyale RIFT VALLEY Takaba NORTH EASTERN North Horr ACTED ACJ Lodwar Moyale FH AC 3° El Wak 3° Concern ACF Horn Relief B JC FH Turkana AC Buna UNICEF F Loiyangalani IMC F Marsabit WFP Lokichar Mercy USA F Marsabit Solidarités Wajir Tarbaj AJ EASTERN 2° UNICEF F Lokori Girito 2° EASTERN WFP Baragoi Laisamis Wajir AAH/USA SOMALIA West F UGANDA Pokot FH AC NORTH RIFT VALLEY Dadaab Samburu UNICEF EASTERN Tot F RefugeeDif Trans Nzoia Marakwet Maralal Archer's Complex 1° Mt Kitale Baringo WHH 1° Kisima Post J Habaswein Elgon Lugari Lorule WFP WFP Liboi Uasin WESTERN CARE Bungoma Gishu Isiolo Mado Gashi VJ Teso Webuye Eldoret Marigat Busia Isiolo FilmAid Kakamega Keiyo Lare Kinna D Burnt Nyahururu Laikipia Busia Kakamega Forest HI Butere Nandi Koibatek (Thomson's Falls) Meru North Nanyuki Dadaab Siaya Vihiga Subukia Mogotio Meru IRC D 0° Kipkelion Meru 0° Kisumu Londiani Central a Garissa Bondo Koru k LWF Kisumu Rongai Elburgon Nyando Nakuru Nyeri hara Kericho Meru TharakaT NRC J # NyandaruaN Nyeri EmbuEm South V NYANZA Kericho yan Suba Njoro b Garissa Nyamira u SC Kamwaura Molo Nakuru darua G Homa Bay Mawingo CENTRAL Embu Central Buret Kirinyaga Mwingi Suba Homa Mbeere UNHCR Kisii Muranga Nguni Bay Bomet Naivasha Gucha Maragua CENTRAL Migori 1° Sotik Kiambu Thika Thika Migori Narok Mwingi 1° Trans Mara Narok Njoro WFP Bura Nairobi Kolbio Kuria Machakos Nairobi Area Kitui Tana River NAIROBI AREA Hola Heshima Ijara Kenya, Inc. -

Geohydrology of Orth Eastern Province
Geohydrology of orth Eastern Province GEOLOGICAL SURVEY WATER-SUPPLY PAPER 1757-N Prepared in cooperation with the ^ Water Department, Kenya Ministry /%£ of Agriculture under the auspices M^ of the US. Agency for International \v» Development \^s Geohydrology of oEC 2f North Eastern Province, Kenya By W. V. SWARZENSKI and M. J. MUNDORFF CONTRIBUTIONS TO THE HYDROLOGY OF AFRICA AND THE MEDITERRANEAN REGION GEOLOGICAL SURVEY WATER-SUPPLY PAPER 1757-N Prepared in cooperation with the Water Department, Kenya Ministry of Agriculture under the auspices of the U.S. Agency for International Development UNITED STATES GOVERNMENT PRINTING OFFICE, WASHINGTON 1977 UNITED STATES DEPARTMENT OF THE INTERIOR CECIL D. ANDRUS, Secretary GEOLOGICAL SURVEY V. E. McKelvey, Director Library of Congress Cataloging in Publication Data Swarzenski, Wolfgang Victor, 1917- Geohydrology of North Eastern Province, Kenya. (Geological Survey water-supply paper; 1757-N) Bibliography: p. Includes index. Supt. of Docs, no.: I 19.13:1757-N 1. Water, Under ground-Kenya--North-Eastern Province. I. Mundorff, Maurice John, 1910- joint author. II. Title. III. Series: United States. Geological Survey. Water-supply paper; 1757-N. TC801.U2 no. 1757-N [GB1173.K4] 553'.7'0973s [553J.79'0967624] 77-608022 For sale by the Superintendent of Documents, U.S. Government Printing Office Washington; D.C. 20402 Stock Number 024-001-02977-4 CONTENTS Page Abstract ______________________________________ Nl Introduction _____________________________________ 2 Purpose and scope of project ____________________ -

Water Governance and Development in the Drylands: the Case of Wajir County, Kenya
Water governance and development in the drylands: The case of Wajir County, Kenya Partners Acknowledgements This report is part of a collaborative effort of many people and organisations, including the Wajir County Government Water Department, WAJWASCO, the Wajir Community Radio, Mercy Corps, and IIED: Wajir County Government Water Department – Yussuf Dayib Ali, Mohammed Ali, Mohamed Farah, Hussein Abdille, Fatuma Dekow, Shale Abdi Bare, Hassan Abdi Haji, Saida Yusuf, Abdirahim Adan, Ibrahim Hassan Mohammed, Engineer Mwangi, Mohammed Abid Hussein, Abdirizak Hassan WAJWASCO – Ahmed Omar Abdille, Ahmed Abdi Mohamed, Adan Ibrahim, Abakiyo Mohamed Noor, Abdi Mohammed Adan Wajir Community Radio – Halima Kahiya Mercy Corps – Diyad Hujale, Florence Randari, Phelix Ouma, John Burns, Ibrahim Jelle, Daud Hassan, Jimale Hussein, Hussein Noor Abdille, Maryan Jelle Hillow, Shukri Samow Noor IIED – Claire Bedelian, Ced Hesse We would like to thank all the people interviewed as part of the study, especially the community participants for giving up their time freely to talk with us and share their knowledge and experiences. This work is part of the Building Resilience and Adaptation to Climate Extremes and Disasters (BRACED) programme funded by the United Kingdom (UK) Department for International Development (DFID). The contents of this report do not necessarily reflect the views of DFID, the UK Government or Mercy Corps and partners. Photo credits – BRACED programme Suggested citation: Bedelian, C. 2019. Water governance and development in the drylands: The case of Wajir County, Kenya. Wajir County Government working paper. Table of contents Executive Summary 3 1. Introduction 6 2. Good water governance 7 3. Water in the drylands 9 4. -

Wajir East and South SMART Survey Report
NUTRITIONAL ANTHROPOMETRIC AND MORTALITY SURVEY FINAL REPORT WAJIR EAST AND SOUTH DISTRICT NORTH EASTERN PROVINCE, KENYA 18th to 26th JUNE 2014 Caroline Njeri Kimere 1 Table of contents Table of contents .......................................................................................................................................... 2 Acknowledgements ..................................................................................................................................... 5 Acronyms ..................................................................................................................................................... 6 EXECUTIVE SUMMARY .............................................................................................................................. 7 Goals and objectives ................................................................................................................................. 7 Area covered ................................................................................................................................................. 8 Methodology ................................................................................................................................................. 8 Main survey results ....................................................................................................................................... 8 Summary of findings .................................................................................................................................. -

Female Genital Mutilation/ Cutting and Child Marriage Among the Rendille, Maasai, Pokot, Samburu and Somali Communities in Kenya
Baseline Study Report Summary Baseline Study Report Summary Female Genital Mutilation/ Cutting and Child Marriage among the Rendille, Maasai, Pokot, Samburu and Somali Communities in Kenya a Baseline Study Report: Female Genital Mutilation/ Cutting and Child Marriage among the Rendille, Maasai, Pokot, Samburu and Somali Communities in Kenya ©United Nations Children’s Fund (UNICEF), Nairobi, 2017 UNICEF Kenya Office P.O. Box 44145-00100 GPO Nairobi Prepared by Information Research Solutions Lantana Court, Ground Floor Lantana Road, Off Rhapta Road P.O. Box 1282 – 00606 Westlands, Nairobi, Kenya Tel: +254 (020) 24 830 16/26 Email address: [email protected] Website: www.iresearchsolutions.com Edited 2017 by Adam Woolf For further information, please contact: Patrizia Di Giovanni, UNICEF Kenya Deputy Representative: [email protected] Lisa Kurbiel, Chief of Communication: [email protected] Aminul Islam, Child Protection Specialist: [email protected] Haithar Somo, Child Protection Specialist:[email protected] Cover photograph: ©UNICEF/KENA00454/Noorani Baseline Study Report Summary Female Genital Mutilation/ Cutting and Child Marriage among the Rendille, Maasai, Pokot, Samburu and Somali Communities in Kenya Baseline Study Report Summary Foreword In recognition that Female Genital Mutilation (FGM) is not only a harmful practice but a violation of human rights, Kenya has adopted a robust legal framework. The country has ratified several international legal instruments that have become part of the Kenyan law as provided for in Article 2 of the constitution. Further to the provisions of the constitution, the government has enacted the Prohibition of Female Genital Mutilation Act, 2011. The law provides the framework for public engagement and advocacy for accelerating the eradication of FGM. -
KDRDIP) Additional Financing (P166266)
Public Disclosure Authorized GOVERNMENT OF KENYA EXECUTIVE OFFICE OF THE PRESIDENT Social Assessment Report Public Disclosure Authorized Kenya Development Response to Displacement Impacts Project (KDRDIP) Additional Financing (P166266) Public Disclosure Authorized Public Disclosure Authorized May 2018 TABLE OF CONTENTS List of abbreviations and acronyms ................................................................................................................ iv Executive summary ........................................................................................................................................... vi 1.0 Introduction ................................................................................................................................................. 1 1.1 Project summary .............................................................................................................................. 1 1.2 Project development objectives ....................................................................................................... 2 1.3 Project components ......................................................................................................................... 3 1.4 Objectives of the social assessment (SA) ........................................................................................ 4 1.5 Methods ........................................................................................................................................... 4 2.0 Legal and administrative frameworks -

Wajir County Hiv and Aids Strategic Plan 2015/16 - 2018/19
WAJIR COUNTY HIV AND AIDS STRATEGIC PLAN 2015/16 - 2018/19 A County free of new HIV infection, stigma and discrimination WAJIR COUNTY HIV AND AIDS STRATEGIC PLAN 2015/16 - 2018/19 Map of Wajir County Table of Contents List of Figures and Tables ..........................................................................................................................................................v Abbreviations and Acronyms .................................................................................................................................................vi Foreword .....................................................................................................................................................................................vii Preface ....................................................................................................................................................................................... viii Acknowledgements ..................................................................................................................................................................ix Executive Summary ...................................................................................................................................................................x CHAPTER 1: BACKGROUND INFORMATION ON WAJIR COUNTY ...................................................... 1 1.1: Introduction ...................................................................................................................................................