Family Planning Clinics and STD Services
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

World Fertility and Family Planning 2020: Highlights (ST/ESA/SER.A/440)
World Fertility and Family Planning 2020 Highlights ST/ESA/SER.A/440 Department of Economic and Social Affairs Population Division World Fertility and Family Planning 2020 Highlights United Nations New York, 2020 The Department of Economic and Social Affairs of the United Nations Secretariat is a vital interface between global policies in the economic, social and environmental spheres and national action. The Department works in three main interlinked areas: (i) it compiles, generates and analyses a wide range of economic, social and environmental data and information on which States Members of the United Nations draw to review common problems and take stock of policy options; (ii) it facilitates the negotiations of Member States in many intergovernmental bodies on joint courses of action to address ongoing or emerging global challenges; and (iii) it advises interested Governments on the ways and means of translating policy frameworks developed in United Nations conferences and summits into programmes at the country level and, through technical assistance, helps build national capacities. The Population Division of the Department of Economic and Social Affairs provides the international community with timely and accessible population data and analysis of population trends and development outcomes for all countries and areas of the world. To this end, the Division undertakes regular studies of population size and characteristics and of all three components of population change (fertility, mortality and migration). Founded in 1946, the Population Division provides substantive support on population and development issues to the United Nations General Assembly, the Economic and Social Council and the Commission on Population and Development. It also leads or participates in various interagency coordination mechanisms of the United Nations system. -

Family Planning and the Environment
FAMILY PLANNING AND THE ENVIRONMENT STABILIZING POPULATION WOULD HELP SUSTAIN THE PLANET Because everyone counts ABOUT HALF THE EARTH’s biological people’s needs and that face the greatest production capacity has already been di- population growth. verted to human use. Life-supporting eco- z Since the 1960s, fertility in de- systems are affected everywhere by the veloping countries has been reduced planet’s 6.7 billion people, which is pro- from an average of six births per jected to reach at least 9.2 billion by 2050. woman to three, thanks primarily to The links between population the use of contraceptives. However, UNFPA, the United Nations and environmental quality are com- in 56 developing countries, the poorest plex and varied. Understanding them women still average six births, compared Population Fund, is an requires knowledge of consumption rates to 3.2 for the wealthiest. that differ between the rich and the poor, international development z The wealthiest countries, with less than of new and old technologies, of resource 20 per cent of earth’s population and the agency that promotes the extraction and restoration, and of the dy- slowest population growth, account for 86 namics of population growth and migration. right of every woman, man percent of natural resource consumption– Humans are depleting natural re- much of it wasteful–and produce the ma- and child to enjoy a life of sources, degrading soil and water, and cre- jority of the pollution and carbon dioxide. ating waste at an alarming rate, even as health and equal opportunity. z At the other extreme, the depletion of new technology raises crop yields, con- natural resources is occurring most rapidly serves resources and cleans up pollution. -

Family Planning Services APPOINTMENTS COMPREHENSIVE CONTRACEPTIVE SERVICES We Take All Major Insurance Carriers
DUKE OBGYN Family Planning Services APPOINTMENTS COMPREHENSIVE CONTRACEPTIVE SERVICES We take all major insurance carriers. We can also offer financial assistance to uninsured or underinsured patients paying out of pocket. Please call our Family Planning Coordinator directly at 919-668- 7888 for more information or to make an appointment. LOCATION Duke South Clinic 1J 200 Trent Drive Durham, NC 27710 CONTACT Tel: 919-668-7888 Fax: 919-681-4838 OBGYN.DUKE.EDU/FAMILY PLANNING We are pleased to offer a focused family planning program at Duke University Medical Center. Our attending physicians are faculty of the Department of Obstetrics and Gynecology and are specialists in the field of family planning. We specialize in innovative contraceptive techniques and provide MEDICAL AND We provide medical and surgical termination comprehensive contraceptive services, especially for patients with SURGICAL of pregnancy in a private and specialized complex medical issues. TERMINATION environment. Our services include management OF PREGNANCY of complicated pregnancies, mid-trimester Some of these conditions include hypertension (high blood pressure), pregnancies, and terminations for fetal diabetes, coagulation disorders (blood clotting problems), history of anomalies. All patients receive counseling regarding pregnancy options and blood clots (deep vein thrombosis or pulmonary embolism), cardiac procedures, ultrasound confirmation of pregnancy dating, and contraceptive disease, migraines, extensive uterine or cervical surgeries, or a options. We provide 24-hour patient phone contact for emergencies. compromised immune system. CONTRACEPTIVE SERVICES WE OFFER INCLUDE: MANAGEMENT OF We provide services for women experiencing MISCARRIAGE miscarriage, including medical treatment and • Sterilization including Essure tubal occlusion procedure surgical management of pregnancy loss in a (www.essure.com) private, specialized and compassionate outpatient environment. -

Pregnancy Tests for Family Planning
PRODUCT BRIEF Caucus on New and Underused Reproductive Health Technologies Pregnancy tests for family planning Description • Early access to pregnancy tests was associated with earlier access to antenatal care or abortion services in a Low-cost, accurate urine pregnancy tests are a simple study in South Africa.11 tool that can be used to rule out pregnancy for some women and help increase access to same-day provision of family planning methods.* Guidance from the World Efficacy Health Organization (WHO) indicates that, for hormonal contraceptives, a woman can initiate a method if her Proper use and accuracy heath care provider is “reasonably certain she is not Two types of urine pregnancy tests are currently available. 1 pregnant.” Because many family planning providers Both types employ test strips that detect human chorionic in developing countries rely on the presence of menses gonadotropin (hCG) levels in the urine to determine the to rule out pregnancy among clients, women who are likelihood of pregnancy. In the first type, the user holds not menstruating at the time they visit the clinic are a test strip in the urine stream to capture a mid-stream 2,3 routinely denied same-day provision of family planning. sample. In the second type, the user captures a urine Studies show that anywhere from 5 to 50 percent of non- sample in a cup and then dips a test strip into the cup 4,5 menstruating women are denied services, even though (known as a “dip strip test”). With both types, the user several studies have shown that very few of these women only has to wait a few minutes before viewing the results 6,7 are actually pregnant. -

Rights and Empowerment Principles for Family Planning
TRANSPARENCY AND ACCOUNTABILITY Individuals can readily access meaningful information on the design, provision, implementation and evaluation of contraceptive services, programs and policies, including government data. Individuals are entitled to seek remedies and redress at the individual and systems level when duty-bearers have not fulfilled their obligations regarding contraceptive FAMILY PLANNING 2020: information, services and supplies.9 Policy and Programming: Measurement: Markets: RIGHTS AND EMPOWERMENT Ensure national family planning Incorporate indicators into monitoring Identify potential accountability and strategies and plans include that reflect the community and redress mechanisms, which might be accountability and redress mechanisms, service users’ point of view regarding applicable in the contraceptive delivery PRINCIPLES FOR including monitoring and evaluation, availability, accessibility, acceptability, space, including those in the private which are in place and functioning and quality of information and services, sector. Where these mechanisms already regarding the provision of contraceptive as well as awareness of their rights, exist, ensure that they are effectively FAMILY PLANNING information, services and supplies. entitlements, and mechanisms available implemented and enforced. Functioning monitoring and for them to have input and seek redress. accountability mechanisms should integrate community input and share findings with all relevant stakeholders, The fundamental right of individuals to decide, freely The -

Natural Family Planning Fact Sheet
Natural Family Planning Fact Sheet ____________________________________________________________________________ 24-hour Emergency Number/Location WHAT’S INSIDE: SOURCES: What is the natural family planning? Office on Women’s Health Basal body temperature method Calendar Method Birth Control Methods: Frequently Cervical Mucus Method Asked Questions How effective are natural family Fertility Awareness planning methods? Advantages of natural family Centers for Disease Control and planning Prevention Drawbacks of natural family planning Unintended Pregnancy Prevention: Contraception U.S. Department of Health & Human Services 200 Independence Avenue, S.W. Washington, D.C. Oklahoma State Department of Health ODH Form 337 MCH/Perinatal & Reproductive Health Division/Family Planning Program Revised Oct 2014 Office of Population Affairs Natural Family Planning Fact Sheet How effective is natural family planning? Of 100 couples who use natural family planning methods each year, anywhere from 1 to 25 will become pregnant. Natural family planning can be an effective type of birth control if all three methods are used and if all are always used correctly. What is natural family planning? A woman with a normal menstrual cycle has about 8 days a month when she can get pregnant. These include the five days before she ovulates (when an egg is released), the day she ovulates, and about one to two days after ovulation. Natural family planning (sometimes known as fertility awareness or the rhythm method) is an approach to birth control some couples use to predict when these fertile days happen. It involves paying close attention to the menstrual cycle by using methods that include: Basal Body Temperature Method Calendar Method Cervical Mucus Method When all three methods are used together, it is known as the symptothermal method. -

Family Planning and the 2030 Agenda for Sustainable Development
Family Planning and the 2030 Agenda for Sustainable Development Data Booklet Family Planning and the 2030 Agenda for Sustainable Development • Data Booklet Target 3.7 of the Sustainable Development Goals (SDGs) calls on countries “by 2030, to ensure universal access to sexual and reproductive health-care services, including for family planning, information and education, and the integration of reproductive health into national strategies and programmes”. Living up to the commitment of the international community to achieve universal access to reproductive health by 2030 requires the monitoring of key family planning indicators. Trends in contraceptive prevalence and need for family planning satisfied with modern methods indicate where increased investments and commitments by governments and international organizations are needed for the realization of reproductive rights for all people, and to help fulfil the pledge of the 2030 Agenda for Sustainable Development that “no one will be left behind”. Data presented in this booklet are based on the Estimates and Projections of Family Planning Indicators 2019, which includes estimates at the global, regional and country level of contraceptive prevalence, unmet need for family planning and SDG indicator 3.7.1 “Proportion of women who have their need for family planning satisfied with modern methods”. This work was supported, in part, by Grants No. OPP1110679 and OPP1183453, Making Family Planning Count, from the Bill & Melinda Gates Foundation. Suggested citation: United Nations, Department of Economic and Social Affairs, Population Division (2019). Family Planning and the 2030 Agenda for Sustainable Development: Data Booklet. (ST/ESA/ SER.A/429). Copyright © 2019 by United Nations, made available under a Creative Commons license (CC BY 3.0 IGO) http://creativecommons. -

Family Planning and Population Control in Developing Countries: Ethical and Sociocultural Dilemmas
Online Journal of Health Ethics Volume 11 | Issue 1 Article 6 Family planning and population control in developing countries: Ethical and sociocultural dilemmas. Edward A. Komu M.D University of Southern Denmark, [email protected] Salome N. N. Ethelberg University of Southern Denmark, [email protected] Follow this and additional works at: http://aquila.usm.edu/ojhe Part of the Bioethics and Medical Ethics Commons, Health Services Research Commons, and the Other Public Health Commons Recommended Citation Komu, E. A., & Ethelberg, S. N. (2015). Family planning and population control in developing countries: Ethical and sociocultural dilemmas.. Online Journal of Health Ethics, 11(1). http://dx.doi.org/10.18785/ojhe.1101.06 This Article is brought to you for free and open access by The Aquila Digital Community. It has been accepted for inclusion in Online Journal of Health Ethics by an authorized administrator of The Aquila Digital Community. For more information, please contact [email protected]. Introduction The World Health organization refers to family planning as the possibility of allowing individuals and couples to anticipate and attain their desired number of children and the spacing and timing of their births (WHO, 2012). Population controls according to neo-Malthusian are programs and policies with deliberate intention to decrease population growth. It is usually related to neo-Malthusian view and development plans where rising population is negatively associated as a hindrance to national economic growth (Kaler, 2004). It has been predicted by the World Resource Institute that the population will increase by 34% by the year 2050. Of this, over 90% increase will occur in the developing world (Eager, 1973). -
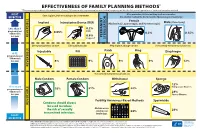
Effectiveness of Family Planning Methods
EFFECTIVENESS OF FAMILY PLANNING METHODS* *The percentages indicate the number out of every 100 women who experienced an unintended pregnancy within the first year of typical use of each contraceptive method. After procedure, little or nothing to do or remember. MOST Once in place, little or nothing to do or remember. EFFECTIVE Use another method for first 3 months (Hysteroscopic, Vasectomy). Female (Vasectomy) Implant Intrauterine Device (IUD) (Abdominal, Laparoscopic, and Hysteroscopic) Male Less than 1 0.2% pregnancy per 0.05% LNG 100 women 0.5% 0.15% PERMANENT in a year REVERSIBLE 0.8% Copper T STERILIZATION Get repeat injections on time. Take a pill each day. Keep in place, change on time. Use correctly every time you have sex. Injectable Pill Patch Ring Diaphragm 6-12 pregnancies per SUN MON TUES WED THUR FRI SAT 100 women 1 in a year 6% 2 9% 9% 9% 12% 3 4 REVERSIBLE Use correctly every time you have sex. Male Condom Female Condom Withdrawal Sponge 12% 18 or more Nulliparous Women pregnancies per 18% 21% 22% 100 women 24% in a year Parous Women Fertility Awareness-Based Methods Spermicide Condoms should always REVERSIBLE JANUARY be used to reduce 1 2 3 4 5 6 7 Abstain or use the risk of sexually 8 9 10 11 12 13 14 Spermicide 28% condoms on 15 16 17 18 19 20 21 24% transmitted infections. fertile days. LEAST 22 23 24 25 26 27 28 29 30 31 1 2 3 4 EFFECTIVE CS248124 Other Methods of Contraception: (1) Lactational Amenorrhea Method (LAM): is a highly effective, temporary method of contraception; and (2) Emergency Contraception: emergency contraceptive pills or a copper IUD after unprotected intercourse substantially reduces risk of pregnancy. -

BY SLOWING POPULATION GROWTH, FAMILY PLANNING CAN HELP ADDRESS FOOD INSECURITY and CLIMATE CHANGE February 3, 2015
BY SLOWING POPULATION GROWTH, FAMILY PLANNING CAN HELP ADDRESS FOOD INSECURITY AND CLIMATE CHANGE February 3, 2015 Executive Summary Slowing the rapid growth of human population through strengthened voluntary family planning services would powerfully and inexpensively contribute to improvements in food security and the reduction of the greenhouse gas emissions that cause climate change. A confluence of long-term environmental and population trends is undermining world food availability and driving climate change. These trends include quickening climate changes and difficulty adapting to its effects; widespread depletion of water, soils and fisheries; increased diversion of grains from human consumption to bio-fuel production and livestock and poultry feed; rapid population growth, particularly in sub-Saharan Africa and South Asia; and increasing affluence in middle income countries. Insufficient food is a serious problem for more than 800 million people, and the problem will only continue to mount as the population grows. The global community has not adequately addressed the important links between food security, climate, family planning, and population growth. Future food security can be improved substantially by decreasing future demand for food. This can be accomplished by meeting the already existing need for voluntary family planning in developing countries, thereby reducing unintended pregnancy and slowing population growth. Further, reducing unintended pregnancy and slowing growth decreases the need to expand health facilities and schools; gives couples the opportunity to invest more in the welfare of each child; and promotes the economic benefits of a “demographic bonus” due to a more favorable age distribution with fewer dependents who are not working. Since agriculture and livestock together emit 30% of all greenhouse gasses, reducing the need to increase production of crops and farm animals will also help stabilize the climate. -

How to Be Reasonably Sure a Client Is Not Pregnant
How to Be Reasonably Sure a Client is Not Pregnant Before initiating a medical regimen, health care providers often need to assess whether a woman is pregnant because some medications may have side effects that are potentially harmful to the fetus. According to the World Health Organization (WHO), there is no known harm to the woman, the course of her pregnancy, or fetus if hormonal contraceptive methods are accidentally used during pregnancy. However, it is recommended that family planning providers assess whether a woman seeking contraceptive services might already be pregnant, because women who are currently pregnant do not require contraception. In addition, methods such as IUDs should never be initiated in pregnant women because doing so might lead to septic miscarriage, a serious complication. Providers often rely on the presence of menses as an indicator that a woman is not pregnant. However, providers often see women who want to start a contraceptive method when they are between menstrual periods. Since pregnancy cannot be confirmed or ruled out with a pregnancy test until a woman has missed her period, providers often require women to wait until they menstruate and then come back for method initiation. The pregnancy checklist helps providers rule out pregnancy with reasonable certainty when women are between menstrual periods, allowing women to initiate their method of choice without a delay. FHI 360 (formerly Family Health International) developed the checklist with support from the U.S. Agency for International Development (USAID). The checklist is based on criteria endorsed by the WHO to determine with reasonable certainty that a woman is not pregnant. -

Contraception and Family Planning
INFORMATION SERIES ON SEXUAL AND REPRODUCTIVE HEALTH AND RIGHTS UPDATED 2020 CONTRACEPTION AND FAMILY PLANNING Access to contraception and family planning is well protected under international human rights standards. 214 MILLION WOMEN OF REPRODUCTIVE In the last two decades, the percentage of women accessing AGE IN DEVELOPING contraceptives in both developed and developing countries has COUNTRIES WHO WANT increased. The United Nations Population Fund reports that in TO AVOID PREGNANCY 2019, 63 per cent of women aged 15 to 49 were using some form of contraception 1 ARE NOT USING MODERN method and 58 per cent were using a modern contraception method. This has CONTRACEPTIVE METHODS improved women’s opportunities to choose when and how many children they want to have, which can positively impact not only their right to health, but also their rights to education, work and an adequate standard of living, amongst other human rights. BY PREVENTING UNINTENDED AND Despite these advancements, millions of women continue to lack access to modern RISKY PREGNANCIES, contraceptives. Today, an estimated 885 million women in developing regions want CONTRACEPTION/FAMILY to prevent a pregnancy. Three of quarters of these women use a modern method PLANNING DECREASES of contraception, however, one quarter—214 million—have an unmet need for 2 THE RISKS OF MATERNAL contraception. While contraceptive use is above 70 per cent in Europe, Latin MORTALITY AND America and the Caribbean, and Northern America, it is below 25 per cent in LONG-TERM MORBIDITY Middle and