Lumbar Puncture Test in Normal Pressure Hydrocephalus: Does the Volume of CSF Removed Affect the Response to Tap?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Serial Tap Test of Patients with Idiopathic Normal Pressure
da Rocha et al. Fluids Barriers CNS (2021) 18:22 https://doi.org/10.1186/s12987-021-00254-3 Fluids and Barriers of the CNS RESEARCH Open Access Serial Tap Test of patients with idiopathic normal pressure hydrocephalus: impact on cognitive function and its meaning Samanta Fabrício Blattes da Rocha1* , Pedro André Kowacs1,2, Ricardo Krause Martinez de Souza1, Matheus Kahakura Franco Pedro1, Ricardo Ramina1 and Hélio A. Ghizoni Teive3 Abstract Background: Idiopathic normal pressure hydrocephalus (INPH) is characterized by gait disturbance, urinary incon- tinence and cognitive decline. Symptoms are potentially reversible and treatment is based on cerebrospinal fuid shunting. The tap test (TT) is used to identify patients that will beneft from surgery. This procedure consists of the withdrawal of 20 to 50 mL of cerebrospinal fuid (CSF) through a lumbar puncture (LP) after which the symptoms of the triad are tested. Improvement in the quality and speed of gait are already recognized but cognitive improvement depends on several factors such as tests used, the time elapsed after LP for re-testing, and the number of punctures. Serial punctures may trigger similar conditions as external lumbar drainage (ELD) to the organism. Objective: This study aimed to identify how serial punctures afect cognition to increase the sensitivity of the test and consequently the accuracy of surgical indication. Methods: Sixty-one patients with INPH underwent baseline memory and executive tests repeatedly following the 2-Step Tap Test protocol (2-STT – two procedures of 30 mL lumbar CSF drainage separated by a 24-h interval). The baseline scores of INPH patients were compared with those of 55 healthy controls, and with intragroup post-puncture scores of the 2-STT. -

Lumbar Puncture (LP)
Lumbar puncture (LP) What is a lumbar puncture (LP)? Who will perform this test? An LP is a common and routine procedure, also A doctor trained in performing this procedure known as a spinal tap, where a very small will do the LP. A trained children’s nurse will hold needle is inserted through the base of the spine your infant in the appropriate position (which to collect a sample of the fluid surrounding the is lying on their side curled up in a tight ball). brain and spinal cord. This fluid is called Another team member may also be present to cerebrospinal fluid (CSF). help. Why do we need to do this? Can you be present during the LP? LP is the only way to confirm a case of Yes, you can tell the team that you would like to meningitis (swelling of the lining of the brain be present. However, many parents find it caused by an infection in the CSF). distressing to see any procedures being done on their baby and would rather not be present. This National guidelines strongly recommended that is perfectly understandable. Please let the team an LP is done alongside other routine know and they will usually agree to whatever investigations, such as blood and urine tests, works best for you but be aware that it is best to look for signs of infection if meningitis is to be quiet so the doctor can concentrate on the suspected. This is a routine and very important procedure. investigation. Is it a painful procedure? Getting a sample of CSF will help Drs to find out An LP is an uncomfortable procedure similar to if your child has meningitis and if what is a blood test or drip being inserted. -

Post-Lumbar Puncture Headache—Does Hydration Before Puncture Prevent Headache and Affect Cerebral Blood Flow?
Journal of Clinical Medicine Article Post-Lumbar Puncture Headache—Does Hydration before Puncture Prevent Headache and Affect Cerebral Blood Flow? Magdalena Nowaczewska 1,* , Beata Kukulska-Pawluczuk 2, Henryk Ka´zmierczak 3 and Katarzyna Pawlak-Osi ´nska 1 1 Department of Pathophysiology of Hearing and Balance, Ludwig Rydygier Collegium Medicum in Bydgoszcz Nicolaus Copernicus University, M. Curie 9, 85-090 Bydgoszcz, Poland; [email protected] 2 Department of Neurology, Ludwig Rydygier Collegium Medicum in Bydgoszcz Nicolaus Copernicus University, M. Curie 9, 85-090 Bydgoszcz, Poland; [email protected] 3 Department of Otolaryngology, Head and Neck Surgery, and Laryngological Oncology, Ludwik Rydygier Collegium Medicum in Bydgoszcz Nicolaus Copernicus University, M. Curie 9, 85-090 Bydgoszcz, Poland; [email protected] * Correspondence: [email protected]; Tel.: +48-52-585-4716 Received: 8 September 2019; Accepted: 15 October 2019; Published: 17 October 2019 Abstract: Headache is a common complication after diagnostic lumbar puncture (DLP). We aimed to check whether hydration before puncture influences the incidence of post-lumbar puncture headache (PLPH) and affects cerebral blood flow. Ninety-nine patients enrolled for puncture were assigned to a group with (n = 40) or without hydration (n = 59). In the hydration group, 1000 mL 0.9% NaCl was infused and a minimum of 1500 mL oral fluids was recommended within the 24 h before puncture. A Transcranial Doppler (TCD) was performed before and after DLP. Mean velocity (Vm) and pulsatility index (PI) were measured in the middle cerebral arteries (MCAs). PLPH occurred in 28 patients (28.2%): six (15.4%) from the hydrated and 22 (37.3%) from the non-hydrated group (p < 0.023). -

Quantitative MRI for Rapid and User-Independent Monitoring of Intracranial CSF Volume in Hydrocephalus
ORIGINAL RESEARCH ADULT BRAIN Quantitative MRI for Rapid and User-Independent Monitoring of Intracranial CSF Volume in Hydrocephalus X J. Virhammar, X M. Warntjes, X K. Laurell, and X E.-M. Larsson ABSTRACT BACKGROUND AND PURPOSE: Quantitative MR imaging allows segmentation of different tissue types and automatic calculation of intracranial volume, CSF volume, and brain parenchymal fraction. Brain parenchymal fraction is calculated as (intracranial volume Ϫ CSF volume) / intracranial volume. The purpose of this study was to evaluate whether the automatic calculation of intracranial CSF volume or brain parenchymal fraction could be used as an objective method to monitor volume changes in the ventricles. MATERIALS AND METHODS: A lumbar puncture with drainage of 40 mL of CSF was performed in 23 patients under evaluation for idiopathic normal pressure hydrocephalus. Quantitative MR imaging was performed twice within 1 hour before the lumbar puncture and was repeated 30 minutes, 4 hours, and 24 hours afterward. For each time point, the volume of the lateral ventricles was manually segmented and total intracranial CSF volume and brain parenchymal fraction were automatically calculated by using Synthetic MR postprocessing. RESULTS: At 30 minutes after the lumbar puncture, the volume of the lateral ventricles decreased by 5.6 Ϯ 1.9 mL (P Ͻ .0001) and the total intracranial CSF volume decreased by 11.3 Ϯ 5.6 mL (P Ͻ .001), while brain parenchymal fraction increased by 0.78% Ϯ 0.41% (P Ͻ .001). Differences were significant for manual segmentation and brain parenchymal fraction even at 4 hours and 24 hours after the lumbar tap. -

The Clinical Effect of Lumbar Puncture in Normal Pressure Hydrocephalus
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.45.1.64 on 1 January 1982. Downloaded from Journal of Neurology, Neurosurgery, and Psychiatry 1982;45:64-69 The clinical effect of lumbar puncture in normal pressure hydrocephalus C WIKKELS0, H ANDERSSON, C BLOMSTRAND, G LINDQVIST From the Department of Neurology and Neurosurgery, Sahlgren Hospital, University of Goteborg, Sweden SUMMARY Owing to all the difficulties involved in selecting patients with normal pressure hydro- cephalus for shunt-operation, a cerebrospinal fluid-tap-test (CSF-TT) is introduced. Psychometric and motor capacities of the patients are measured before and after lumbar puncture and removal of 40-50 ml CSF. Patients fulfilling criteria for normal pressure hydrocephalus were compared to patients with dementia and atrophy shown by computed tomography. Normal pressure hydro- cephaluspatients showed temporary improvement after lumbar puncture. The extent ofthe temporary improvement appeared to be well correlated with the improvement after shunt operation. Accord- ingly, the CSF-TT seems to be of value when selecting those patients who will probably benefit from a shunt operation. The syndrome of normal pressure hydrocephalus is pressure by lumbar puncture caused both subjective Protected by copyright. characterised by gait disturbance, progressive mental and objective temporary improvement in some deterioration and urinary incontinence.' Particularly patients with normal pressure hydrocephalus.10 16 17 noteworthy is the complex gait disturbance with Such patients also improved after CSF-shunting. spastic-ataxia, extrapyramidal components, and However, no details have been given about the commonly dyspraxia of gait.2 In addition, there is in amount of CSF which was drained or to what degree typical cases mental "slowing up" with lack of the CSF pressure was lowered. -

Ventriculoperitoneal Shunts in the Emergency Department: a Review
Open Access Review Article DOI: 10.7759/cureus.6857 Ventriculoperitoneal Shunts in the Emergency Department: A Review Michael Ferras 1 , Nicholas McCauley 1 , Trilok Stead 2 , Latha Ganti 3, 4, 5 , Bobby Desai 6 1. Emergency Medicine, Ocala Regional Medical Center, University of Central Florida, Ocala, USA 2. Emergency Medicine, Trinity Preparatory School, Winter Park, USA 3. Emergency Medicine, Envision Physician Services, Orlando, USA 4. Emergency Medicine, University of Central Florida College of Medicine/Hospital Corporation of America Graduate Medical Education Consortium of Greater Orlando, Orlando, USA 5. Emergency Medicine, Polk County Fire Rescue, Bartow, USA 6. Emergency Medicine, Ocala Regional Medical Center, University of Central Florida College of Medicine, Ocala, USA Corresponding author: Latha Ganti, [email protected] Abstract In this paper, we review the indications, complications, and pitfalls associated with ventriculoperitoneal (VP) shunts. As most VP shunt problems initially present to the emergency department, it is important for emergency physicians to be well-versed in managing them. In the article, the possible reasons for shunt failure are explored and summarized using an infographic. We also examine potential clinical presentations of VP shunt failure. Categories: Emergency Medicine, Neurosurgery Keywords: ventriculoperitoneal shunts Introduction And Background Emergency department physicians usually see a large number of patients with medical maladies managed by the aid of instrumentation or hardware such as a ventriculoperitoneal (VP) shunt. While patients have shunts placed for multiple reasons, it is important for emergency service providers to know how to evaluate, troubleshoot, and treat those with VP shunt complications. An estimated 30,000 VP shunt procedures are performed yearly in the United States [1]. -

Role of Lumbar Puncture in Traumatic Brain Injury
308 Indian Journal of Public Health Research & Development, April-June 2021, Vol. 12, No. 2 Role of Lumbar Puncture In Traumatic Brain Injury Ranjeet Kumar Jha1, Rachna Gupta2 1Assistant Professor, Department of Neurosurgery, 2Professor, Department of Surgery, Shyam Shah Medical College, Rewa Abstract Background: Cerebrospinal fluid (CSF) drainage via ventricular puncture is an established therapy of elevated intracranial pressure (ICP). In contrast, lumbar CSF removal is believed to be contraindicated with intracranial hypertension. Method: We investigated the safety and efficacy of lumbar CSF drainage to decrease refractory elevated ICP in a small cohort of patients with traumatic brain injury (TBI). A score (0–8 points) was used to assess computed tomography (CT) images for signs of herniation and for patency of the basal cisterns. All patients received lumbar CSF drainage either as a continuous drainage or as a single lumbar puncture (LP). Type and method of CSF drainage, mean ICP 24 h prior and after CSF removal, and adverse events were documented. Outcome was assessed after 3 months (with dichotomized Glasgow outcome scale). Results: Eight patients were evaluated retrospectively. n = 5 suffered a moderate, n = 2 a severe TBI (one Glasgow coma score not documented). The CT score was ≥5 in all patients prior to LP and decreased after puncture without clinical consequences in two patients. The amount of CSF removal did not correlate with score changes (P = 0.45). CSF drainage led to a significant reduction of mean ICP (from 22.3 to 13.9 mmHg, P = 0.002). Continuous drainage was more effective than a single LP. Three of eight patients reached a favorable outcome. -

Endoscopic Third Ventriculostomy in Post Traumatic Hydrocephalus- Institutional Experience
Original Research Article DOI: 10.18231/2455-8451.2018.0015 Endoscopic third ventriculostomy in post traumatic hydrocephalus- Institutional experience Geover J. Lobo1, Madhukar T. Nayak2,* 1Assistant Professor, 2Professor, Dept. of Neurosurgery, Fr. Muller Medical College & Hospital, Mangaluru, Karnataka, India *Corresponding Author: Email: [email protected] Abstract Introduction: Hydrocephalus is a known sequelae in traumatic brain injury patients. It may occur early or late and presents with dementia, urinary incotinence and difficulty in walking as described by Hakim and Adams. There are two distinct types of normal pressure hydrocephalus one is idiopathic most commonly seen in the elderly age groups and the other is secondary due to a cerebro vascular accident, trauma or surgery. The idiopathic type may not respond to the CSF diversion procedure, but the secondary type which responds to CSF diversion procedure. Our study aims at exploring the option of ETV in these patients not making them shunt dependent. Materials and Methods: The patients with traumatic brain injury admitted in the dept. of neurosurgery between January 2012 and January 2018 were included into the study. Congenital hydrocephalus and secondary hydrocephalus due to spontaneous SAH and tumours were excluded. 14 patients were identified and if there was some improvement in their condition after CSF tap test were planned for endoscopic third ventriculostomy. Results: Out of the 14 patients 2 were females and the remaining 12 were males. 2 did not improve at all. 12 had some improvement out of which 3 had a failure and underwent a v-p shunt. Hence there were 5 failures out of 14 which made 35.7%. -

Idiopathic Normal Pressure Hydrocephalus: Diagnostic and Predictive Value of Clinical Testing, Lumbar Drainage, and CSF Dynamics
CLINICAL ARTICLE J Neurosurg 125:591–597, 2016 Idiopathic normal pressure hydrocephalus: diagnostic and predictive value of clinical testing, lumbar drainage, and CSF dynamics *Cynthia V. Mahr, MD,1 Markus Dengl, MD,1 Ulf Nestler, MD,1 Martin Reiss-Zimmermann, MD,2 Gerrit Eichner, ScD,3 Matthias Preuß, MD,1 and Jürgen Meixensberger, MD 1Departments of 1Neurosurgery and 2Neuroradiology, University Hospital Leipzig; and 3Mathematical Institute, Justus-Liebig University Gießen, Germany OBJECTIVE The aim of the study was to analyze the diagnostic and predictive values of clinical tests, CSF dynamics, and intracranial pulsatility tests, compared with external lumbar drainage (ELD), for shunt response in patients with idio- pathic normal pressure hydrocephalus (iNPH). METHODS Sixty-eight consecutive patients with suspected iNPH were prospectively evaluated. Preoperative assess- ment included clinical tests, overnight intracranial pressure (ICP) monitoring, lumbar infusion test (LIFT), and ELD for 24–72 hours. Simple and multiple linear regression analyses were conducted to identify predictive parameters concern- ing the outcome after shunt therapy. RESULTS Positive response to ELD correctly predicted improvement after CSF diversion in 87.9% of the patients. A Mini–Mental State Examination (MMSE) value below 21 was associated with nonresponse after shunt insertion (specific- ity 93%, sensitivity 67%). Resistance to outflow of CSF (ROut) > 12 mm Hg/ml/min was false negative in 21% of patients. Intracranial pulsatility parameters yielded different results in various parameters (correlation coefficient between pulse amplitude and ICP, slow wave amplitude, and mean ICP) but did not correlate to outcome. In multiple linear regression analysis, a calculation of presurgical MMSE versus the value after ELD, ROut, and ICP amplitude quotient during LIFT was significantly associated with outcome (p = 0.04). -

The Adjustable Shunt Valve in the Treatment of Adult Hydrocephalus Effect on Complications, Intracranial Pressure and Clinical Symptoms
The adjustable shunt valve in the treatment of adult hydrocephalus Effect on complications, intracranial pressure and clinical symptoms Dan Farahmand Department of Neurosurgery Institute of Neuroscience and Physiology Sahlgrenska Academy at University of Gothenburg Click here to enter text. The adjustable shunt valve in the treatment of adult hydrocephalus Effect on complications, intracranial pressure and clinical symptoms © Dan Farahmand 2014 [email protected] ISBN 978-91-637-5698-6 Printed in Gothenburg, Sweden 2014 by Ineko AB To my beloved wife Johanna and to our wonderful sons Valter and Viktor ABSTRACT Background: Hydrocephalus causes impaired gait, balance, cognition and continence, all of which can be reversed by shunt treatment. Adjustable valves are commonly used in the shunt treatment of hydrocephalus but randomized controlled trials (RCT) are scarce. The aim of the present thesis was to evaluate adjustable valves in the treatment of hydrocephalus. Patients and Methods: In Study I, 450 hydrocephalus patients undergoing primary shunt insertion were followed over 10 years to investigate the short- term perioperative risk factors of shunt surgery. In Study II the relationship between intracranial pressure (ICP) and ICP wave amplitude (AMP), valve settings and body positions were studied in 15 hydrocephalus patients. During the shunt operation an intraparenchymatous ICP-sensor was simultaneously inserted and ICP/AMP analyzed with the shunt ligated and when opened at different opening pressures and body positions. A double- centered RCT was conducted in studies III and IV, including 68 patients with iNPH. The patients received a ventricular shunt and were randomized into two groups; in one group (20-4) the valve was initially set to 20 cm H2O and gradually reduced to 4 cm H2O over the course of the 6 month study period. -
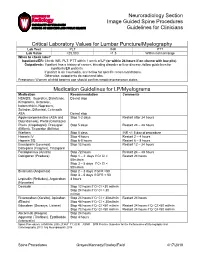
Neuroradiology Section Image Guided Spine Procedures Guidelines for Clinicians
Neuroradiology Section Image Guided Spine Procedures Guidelines for Clinicians Critical Laboratory Values for Lumbar Puncture/Myelography Lab Test PLT INR PTT Lab Value >25,000 <1.5 Within normal range When to check labs? Inpatients/ER: Check INR, PLT, PTT within 1 week of LP (or within 24 hours if on chemo with low plts) Outpatients: If patient has a history of cancer, bleeding disorder or liver disease, follow guidelines for inpatients/ER patients If patient is on Coumadin, see below for specific recommendations. Otherwise, outpatients do not need labs. Pregnancy: Women of child bearing age should confirm negative pregnancy status Medication Guidelines for LP/Myelograms Medication Recommendation Comments NSAIDS: Ibuprofen, Diclofenac, Do not stop Ketoprofen, Ketorolac, Indomethicin, Naproxen, Sulindac, Diflunisal, Celecoxib ASA Do not stop Aggrenox/persantine (ASA and Stop 1-2 days Restart after 24 hours Dipyridamole), Pletal (Cilostazol) Plavix (Clopidogrel), Prasugrel Stop 5 days Restart 24 – 48 hours (Effient), Ticagrelor (Brilinta) Warfarin Stop 5 days INR <1.5 day of procedure Heparin IV Stop 4 hours Restart 2 – 4 hours Heparin SQ Stop 6-8 hours Restart 6 – 8 hours Enoxaparin (Lovenox), Stop 12 hours Restart 12 – 24 hours Dalteparin (Fragmin), Tinzaparin Fondaparinux (Arixtra) Stop 72 hours Restart 24 – 48 hours Dabigatran (Pradaxa) Stop 1 – 2 days if Cr Cl > Restart 24 hours 50ml/min Stop 3 – 5 days if Cr Cl < 50ml/min Bivalrudin (Angiomax) Stop 2 – 3 days if GFR >50 Stop 3 – 5 days if GFR < 50 Lepirudin (Refludan), Argatroban 4 hours (Novastan) Desrudin Stop 12 hours if Cr Cl >30 ml/min Stop 24 hours if Cr Cl < 30 ml/min Rivaroxaban (Xarelto), Apixaban Stop 24 hours if Cr Cl > 30ml/min Restart 24 hours (Eliquis) Stop 48 hours if Cr Cl < 30ml/min Edoxaban (Savasya, Lixiana) Stop 48 hours if Cr Cl >50 ml/min Restart 24 hours if Cr Cl >50 ml/min Stop 72 hours if Cr Cl <50 ml/min Restart 24 hours if Cr Cl <50 ml/min Abciximab (Reopro) Stop 24 hours Aggrastat (Tirofiban), Eptifibatide Stop 4 hours (Intergrelin) Spinal Procedures. -
Ventriculoperitoneal Shunt Occlusion and Cranioplasty. a Case Report
Ventriculoperitoneal shunt occlusion and cranioplasty. A case report Lívio Pereira de Macêdo, Arlindo Ugulino Netto, Juan Pablo Borges R. Maricevich, Nivaldo S. Almeida, Hildo Rocha Cirne Azevedo-Filho DOI: 10.33962/roneuro-2020-063 Romanian Neurosurgery (2020) XXXIV (1): pp. 405-410 DOI: 10.33962/roneuro-2020-063 www.journals.lapub.co.uk/index.php/roneurosurgery Ventriculoperitoneal shunt occlusion and cranioplasty. A case report Lívio Pereira de Macêdo1, Arlindo Ugulino Netto1, Juan Pablo Borges Rodrigues Maricevich2, Nivaldo S. Almeida1, Hildo Rocha Cirne Azevedo-Filho1 1 Department of Neurosurgery, Hospital da Restauração, Recife, Pernambuco, BRAZIL 2 Department of Plastic Surgery, Hospital da Restauração, Recife, Pernambuco, Brazil ABSTRACT Keywords Decompressive craniectomy (DC) is an urgent neurosurgical procedure, effective in cranioplasty, the reduction of intracranial pressure (ICP) in patients with elevated ICP and in VPS, complications of brain infarction that do not respond to clinical treatment; traumatic VPS Occlusion brain injury (TBI); intracerebral haemorrhage (ICH) and aneurysmal intracerebral haemorrhage. Symptomatic hydrocephalus is present in 2 to 29% of patients who undergo craniectomy. They may require a ventriculoperitoneal shunt (VPS). The literature does not yet show standard management of cranioplasty in patients who have previously undergone a shunt, showing evidence of sinking skin flap syndrome. This case shows parenchymal expansion after VPS occlusion and cranioplasty in the Corresponding author: Lívio Pereira de Macêdo patient’s profile. The 23-year-old male patient, right-handed, went to the hospital in January 2017 due to severe traumatic brain injury following multiple traumas. The Department of Neurosurgery, patient underwent urgent DC surgery for the management of elevated ICP.