Haydon Bridge and Allendale Medical Practice Quality Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Public Toilet Map NCC Website
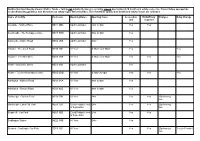
Northumberland County Council Public Tolets - Toilets not detailed below are currently closed due to Covid-19 health and safety concerns. Please follow appropriate social distancing guidance and directions on safety signs at the facilities. This list will be updated as health and safety issues are reviewed. Name of facility Postcode Opening Dates Opening times Accessible RADAR key Charges Baby Change unit required Allendale - Market Place NE47 9BD April to October 7am to 4pm Yes Yes Allenheads - The Heritage Centre NE47 9HN April to October 7am to 4pm Yes Alnmouth - Marine Road NE66 2RZ April to October 24hr Yes Alnwick - Greenwell Road NE66 1SF All Year 6:30am to 6:30pm Yes Yes Alnwick - The Shambles NE66 1SS All Year 6:30am to 6:30pm Yes Yes Yes Amble - Broomhill Street NE65 0AN April to October Yes Amble - Tourist Information Centre NE65 0DQ All Year 6:30am to 6pm Yes Yes Yes Ashington - Milburn Road NE63 0NA All Year 8am to 4pm Yes Ashington - Station Road NE63 9UZ All Year 8am to 4pm Yes Bamburgh - Church Street NE69 7BN All Year 24hr Yes Yes 20p honesty box Bamburgh - Links Car Park NE69 7DF Good Friday to end 24hr Yes Yes 20p honesty of September box Beadnell - Car Park NE67 5EE Good Friday to end 24hr Yes Yes of September Bedlington Station NE22 5HB All Year 24hr Yes Berwick - Castlegate Car Park TD15 1JS All Year Yes Yes 20p honesty Yes (in Female) box Northumberland County Council Public Tolets - Toilets not detailed below are currently closed due to Covid-19 health and safety concerns. -

John Martin Heritage Trail 0 ⁄2 1 Mile from the Information Panel Follow Church Street Towards Southern Section 0 0.5 1 Km N Ratcliffe Road
. 0 9 7 2 4 0 0 0 1 r e b m u n e c n e c i L . d e v r e s e r s t h g i r l l A . 7 0 0 2 t h g i r y p o c n w o r C © p a M h c r u h C s ’ t r e b h t u C t S . k s i r n w o r i e h t t a o s o d l i a r T e g a t i r e H n i t r a M n h o J e h t g n i k l a w e l p o e P i . k l a w y r t n u o c a e g d i r B n o d y a H n o t n e s e r p s r e g n a d d n a s k s i r y n a m e h t f o e r a w a e B e r e h t r a t S . l l i H p s E d n a e l t s a C y e l g n a L t a 6 8 6 A e h t n o d n a s e n a l y r t n u o c i n o , s e l c i h e v m r a f e g r a l g n i d u l c n i , c i f f a r t f o e r a w e B • R i v e r S o u . -

Haydon News on Line
THE HAYDON NEWS ON LINE Dan Anderson & Tom Robb, Tom Craggs & Michael O’Riordan, Michael Thirlaway & ‘Dickie’ Lambert, Mick Hayter & Chad Alder get set for the Annual Wheelbarrow Race on Easter Monday. The race was supported by the Haydonian Social Club, the Anchor Hotel, the General Havelock and the Railway Hotel. INSIDE THIS ISSUE PAGE Parish Council Notes 3/13 Historical Notes 4 to 6 Correspondence 6 All The Way From Haydon Bridge 7 Issue 4 A Museum Is Born 8 Haydon Bridge War Memorial 9 THE NEXT ISSUE OF THE A View From Up There….. 10 HAYDON NEWS WILL BE PUBLISHED May IN JUNE 2011 John Martin Heritage Centre 11 John Martin Heritage Festival Events 12 All copy to the editors 2011 Haydon Bridge High School 13 as soon as possible, but not later than Church Pages 14/15 Friday May 22nd 2011. www.haydon-news.co.uk Notices 16 Thank you. Crossword 17 e mail: [email protected] HAYDONPublished NEWS by The Friends Of Haydon Bridge Page 1 THE HAYDON NEWS ON LINE In last month’s article on the Community Centre, the regular club meetings and other activities at the Community The Haydon News was Established in 1979 and preceded Centre were listed. Unfortunately the Bowls Club Thursday on and off for over forty five years by a church Parish evening meetings were omitted from the list. Magazine, The Haydon News is published by the Friends We apologise for this omission. The Editors of Haydon Bridge and is written, printed, collated and delivered by volunteers. -

HAYDON BRIDGE Conservation Area Character Appraisal
HAYDON BRIDGE Conservation Area Character Appraisal Adopted March 2009 Tynedale Council Haydon Bridge Conservation Area Character Appraisal CONTENTS 1 Introduction 2 2 Statement of Significance 7 3 Historic Development 8 4 Context 14 5 Spatial Analysis 20 6 Character analysis 29 7 Public Realm 46 8 Management recommendations 48 9 Appendix 1 Policies 52 Appendix 2 Listed Buildings 56 Appendix 3 Maps 57 Appendix 4 Sources 60 Church Street, Haydon Bridge March 2009 1 . Tynedale Council Haydon Bridge Conservation Area Character Appraisal 1 INTRODUCTION 1.2 Haydon Bridge Conservation Area 1.1 Location Conservation areas are ‘areas of special architectural or historic interest, the character or appearance of which it is desirable to Haydon Bridge is located on a gentle meander of the River South preserve or enhance’.1 They are designated by the local planning Tyne approximately ten kilometres to the west of Hexham and authority using local criteria. thirteen kilometres to the east of Haltwhistle. It is divided by the river and the A69 and bisected by the Newcastle to Carlisle railway. Conservation areas are about character and appearance, which It is overlooked by the steep valley sides which are decorated by can derive from many factors including individual buildings, building fields and woodlands. The village is located within Haydon Ward groups and their relationship with open spaces, architectural and its centre is at National Grid reference NY 842644 detailing, materials, views, colours, landscaping and street furniture. Character can also draw on more abstract notions such as sounds, local environmental conditions and historical changes. These things combine to create a locally distinctive sense of place worthy of protection. -

4 Fairhill Cottages, Alston, Cumbria
4 FAIRHILL COTTAGES, ALSTON, CUMBRIA 4 FAIRHILL COTTAGES, ALSTON, CUMBRIA A spacious and charming cottage in the rural town of Alston within an area of outstanding natural beauty. Hexham 25 miles • Penrith 20 miles • Barnard Castle Cross Fell. that can accommodate additional vehicles and 25 miles • Carlisle 28 miles • Newcastle 45 miles Accommodation beyond which is a raised bedded and lawned front Entering into the entrance hallway with feature garden area. Situation fireplace and staircase to the first floor the spacious Alston is a historic town with a cobbled market family kitchen is accessed immediately on your right. General Information place, supporting an interesting variety of shops The kitchen has a stone floor and original exposed and public houses. There are two churches along beams, from the rear window it enjoys beautiful views Services with a health centre, cottage hospital, primary and over the garden and the countryside beyond. It has Mains electricity, gas, water and drainage connected. secondary schools and petrol filling stations. It claims a feature inglenook fireplace, at the heart of which to be one of the highest market towns in England is a Rayburn cooker, fitted wall and base units with Note being approximately 1000 feet above sea level wooden work surfaces, integrated into the units The second floor creates a flying freehold above the and is situated within the North Pennines Area of are a gas hob, electric oven, Belfast style sink and neighbouring cottage. Outstanding Natural Beauty. It lies on the confluence plumbing for washing machine. The sitting room is of the River South Tyne and River Nent and is at the other end of the entrance hallway, the room Tenure surrounded by heather clad moor land with breath- benefits from a double aspect, a charming feature Freehold taking, unspoilt countryside. -

Chesterwood Grange Chesterwood, Hexham, NE47 6HW Chesterwood Grange Chesterwood Hexham NE47 6HW
Chesterwood Grange Chesterwood, Hexham, NE47 6HW Chesterwood Grange Chesterwood Hexham NE47 6HW Guide Price: £695,000 Traditional stone property situated in rural setting with panoramic views to the south and west. · Traditional stone property · Land extending to c. 10.55 acres · Noteworthy character features · Substantial and versatile accommodation · Self-contained home office unit with two offices · Further development potential · EPC rating F Hexham - 01434 608980 DESCRIPTION original fireplaces plus one single bedroom. There are two in an elevated position enjoying beautiful views over the Traditional stone property situated in rural setting with views to bathrooms and a separate w/c. surrounding countryside. the south and west. EXTERNALLY Haydon Bridge is a popular village with an excellent range of local Chesterwood Grange is a traditional period farmhouse boasting The property is accessed from the lane onto a gated tarmac drive. services and amenities including a small supermarket, butchers, many character features. Benefitting from further extension into There are mature well maintained south facing gardens with a post office and pharmacy. The market town of Hexham is just 6.5 the adjoining outbuildings it provides a substantial amount of wicket gate leading to the land. miles to the east providing a wider range of amenities. accommodation making the perfect family home. A traditional outbuilding houses three stores with another to Railway stations in Haydon Bridge and Hexham which provide The lobby leads to a well appointed kitchen with aga, wall and the rear of the property housing the boiler further links east and west. The A69 and A68 are in close floor units and a staircase to the first floor. -

Building Plots at Thornley Gate Allendale ▪ Hexham ▪ Northumberland ▪ Ne47 9Nh Building Plots at Thornley Gate Allendale ▪ Hexham ▪ Northumberland ▪ Ne47 9Nh
BUILDING PLOTS AT THORNLEY GATE ALLENDALE ▪ HEXHAM ▪ NORTHUMBERLAND ▪ NE47 9NH BUILDING PLOTS AT THORNLEY GATE ALLENDALE ▪ HEXHAM ▪ NORTHUMBERLAND ▪ NE47 9NH Hexham 10 Miles ▪ Corbridge 14 Miles ▪ Newcastle 34 Miles Exciting development opportunity • Full planning permission to build two semi detached dwellings • Generously proportioned plots with integral garaging and off road parking • Sought after location, rarely available for development Guide Price £300,000 Wolsingham 01388 529579 [email protected] The Area Directions Thornley Gate is a small settlement sat between Catton and From the A69, leave the road at Haydon Bridge, onto the Allendale, situated close to Hexham amidst delightful and A686. Follow the road for approximately 2.5 miles, then turn unspoilt countryside. Allendale has a range of shopping, left onto the B6295 towards Langley. Continue on the course educational and recreational facilities and the renowned of the road for around 4 further miles, driving through the Market Town of Hexham lies 9 miles distant. For the village of Catton, towards Allendale Town, at the cross roads commuter the A69, A1(M) and M6 provide links with the major turn right. Upon approaching the next crossroads, bear right commercial centres of the North. East and West Coast railway and the property is on the right hand side and is identified by a services and Newcastle International Airport provide further George F White for sale board. communication with the rest of the country. Many of the region’s beauty spots and attractions can be found within a Planning short drive beyond including the delights of North Yorkshire, The property benefits from full planning permission application The Lake District, The Scottish Borders and the North East number 19/01950/FUL. -

Haydon Parish Plan • 2008 – 2018 & Village Design Statement
HAYDON BRIDGE GATEWAY TO HADRIAN’S WALL COUNTRY HAYDON PARISH PLAN • 2008 – 2018 & VILLAGE DESIGN STATEMENT Final Reports and Action Plan October 2008 HAYDON PARISH PLAN 2008-2018 Page FOREWORD 3 EXECUTIVE SUMMARY 3 1 INTRODUCTION AND STRUCTURE OF THE PLAN 5 2 HOW THE WORK FOR THE PLAN WAS CARRIED OUT 6 3 PARISH PROFILE 10 4 WHAT WE HAVE FOUND – KEY ISSUES 19 5 PUTTING OUR PLAN IN A WIDER CONTEXT 23 6 THE WAY AHEAD 26 7 ACTION PLAN 37 APPENDIX 1 48 HAYDON PARISH PLAN 2008-2018 FOREWARD It is just over 10 years since we last completed a Parish Plan (then called a Parish Appraisal). It resulted in some major and tangible achievements, including the building of the new Community Centre. This Parish Plan comes at a time of change for the Parish itself, for example the potential impact of the bypass on both the economy and well-being of our community. There is also wider change in the structures of local government with the disappearance of Tynedale Council, and the creation of the new Northumberland wide unitary council in 2009. Parish Plans are important for three main reasons. Firstly, they identify issues of importance to our community through the public consultation that goes with the plan. Secondly, they provide the evidence to support applications for public, private and charitable funding to support initiatives or projects identified by groups in the Parish. Thirdly, they provide information for a range of organisations – for example local and regional government, the health service, and other public, private and third sector organisations – about the Parish, the services it needs and the potential for investment as partners in our future. -

The Haydon News
THE HAYDON NEWS UN-STABLE INSIDE THIS ISSUE PAGE Editorial 2 Parish Council Notes 3 Historical Notes 4/5 Bygone Chesterwood 6 Cricket fixtures 7 Issue 06 Tula’s Travels 7 Poets’ Corner 7 Dr. Steve Ford 8/9 June Church Pages 10/11 Village Project ? 12 2005 HAYDONPublished NEWS by The Friends Of Haydon Bridge Page 1 FRIENDS OF HAYDON BRIDGE EDITORIAL COMMENT. MEMBERSHIP/SUBSCRIPTION FORM. From the Friends of Haydon Bridge a ‘THANK YOU’ to all Please find enclosed membership/subscription fee of £………… our advertisers for their prompt payment for adverts and their continuing support of the Haydon News. Name……………………………………………………. A ‘THANK YOU’ is also due to the many people who have given their support to the Haydon News by paying Address………………………………………………… membership of the ‘Friends’ and/or making a donation . All the money goes towards meeting the cost of producing the ………………………………………………… Haydon News. Cheques made payable to ‘The Friends of Haydon Bridge’ Did you get to this years ‘Haydon Local Artists’ Summer Exhibition ? A great display of local talent. Enquiries in the first instance to [email protected] There are several events in the village in the coming month all advertised in this edition. Unless you live locally and you may leave it at Finally, can I draw your attention to the electrifying feature J.& M. Clarke (newsagents) for collection. from our ‘special correspondent’ on page 12 ? Addressed to The Haydon News It should generate a great deal of interest ! P.S. Bright sparks will make the connection with the ’fair Thank you. wind’ item in Dr Ford’s Page, though none was intended. -

10218 the London Gazette, I?Th September 1970
10218 THE LONDON GAZETTE, I?TH SEPTEMBER 1970 the Council as registration authority aid the above C.L.I 10 Chainley Burn Freestone Quarry and address: Way, Bardon Mill. (a) in the case of an objection to a registration C.L.I 11 West End Town Freestone Quarry, made before 1st July 1968, not later than 30ith Bardon Mill. September 1970, and C.L.I 12 Thorngra-fton Peat Moss and Way, Bardon Mill. (b) in (the case of an objection to a registration C.L.124 Land near Sportsman's Arms, Coanwood. made after 30th June 1968, not later than 31st C.L.125 Land adjoining Beaconshill Plantation, July 1972. Coanwood. Registrations are independent of each other, so .that, Hexham R.D. for example, a registration of land as common land C.L.I *fPart Allendale Common. made before 1st July 1968, and not objected to before C.L.2 *tHexhamshire Common. 1st October 1970, will become final and definitive on C.L.5 f Stagshaw Common. the later date, but if registrations of rights over that C.L.74 Burnside, Ovington. land, or claims to ownership thereof, are made after C.L.75 Beautifiers, Ovington. 30th June 1968, objections to such registrations can C.L.76 The Green, Ovington. be made in the second objection period. C.L.80 Village Green, Ovingham. Every objection which is not rejected is noted on C.L.81 Red Pond, Ovingham. the register as soon as possible after receipt, and par- C.L.83 Jimmy Johnson's Park, Ovingham. ticulars sent by the registration authority to the C.L.84 The Pant, Oyingham. -

XI the Great Inundation of 1771 and the Rebuilding of the North-East's
XI The Great Inundation of 1771 and the Rebuilding of the North-East’s Bridges R. W. Rennison n 1771 a major flood on the rivers of north- All but one of the bridges were of masonry – east England led to the destruction of many arched in form – and the majority of those Ibridges. As an entity, the programme of damaged or destroyed were the responsibility reconstruction has never before been recorded of the Counties’ Justices and administered and this paper has been prepared in an eVort to through Quarter Sessions; some bridges, how- rectify this omission. The majority of the bridges ever, were built under the aegis of private indi- were the property of the respective County viduals or bodies. Rebuilding work was the administrations and, in order to describe the responsibility of either the oYcers of the Coun- rebuilding, the Quarter Sessions records of the ties’ government or consultants. Brief bio- four counties aVected have been used extensively. graphical details of some of these are given in the Appendix – their names are followed by an asterisk (*) where they appear in the text. INTRODUCTION Bridge rebuilding took place at the time of the formation of a civil engineering profession – In the history of river crossings in the north the Society of Civil Engineers was founded in east of England, the major flood of 1771 – the 1771 – and it brought to the area two of its ‘Great Inundation’ – was a landmark, resulting earliest and most distinguished members, John as it did in the destruction of a score of bridges Smeaton and Robert Mylne, although they on the rivers Tyne, Wear and Tees. -

Haydon Parish Housing Needs Survey Final Report
Haydon Parish Housing Needs Survey Final Report May 2020 Produced for Haydon Parish Council 1 Contents Page no. Introduction 2 Population profile 3 The housing needs survey 4 Research findings 5 A selection of individual responses 14 Key messages from the survey 15 Appendix 1: The questionnaire 16 Appendix 2: Parish Council covering letter 26 2 Introduction In November 2019, Haydon Parish Council commissioned Community Action Northumberland (CAN) to undertake a Local Housing Needs Survey for the Haydon parish covering the village of Haydon Bridge, Chesterwood, Langley and all outlying hamlets within the parish. This was designed to provide information useful to the Parish Council and Neighbourhood Planning Steering Group as part of work designed to assess the wider needs of the community. Since April 2017, CAN has been funded by Northumberland County Council, and more recently by Community-led Homes, to establish a Community-led Housing Hub to act as a support platform for local communities in the area wishing to explore the potential for community- led housing in its various forms and to deliver local affordable homes where they are needed. This hub is called ‘Communities CAN (North East).’ This work has been funded through the government’s Community Housing Fund and has sought to support all stages of development, including the initial identification of housing need. As part of this work, CAN has been funded to undertake Local Housing Needs Surveys where requested to do so and where there is a realistic prospect of any need identified resulting in the delivery of additional affordable homes. In undertaking Housing Needs Surveys, CAN follows the principles set out in national guidelines drawn up by the Rural Housing Enablers Network as follows: 1.