Novel Genes and Oligogenic Inheritance in Holoprosencephaly
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Genetic Diagnosis in First Or Second Trimester Pregnancy Loss Using Exome Sequencing: a Systematic Review of Human Essential Genes
Journal of Assisted Reproduction and Genetics (2019) 36:1539–1548 https://doi.org/10.1007/s10815-019-01499-6 REVIEW Genetic diagnosis in first or second trimester pregnancy loss using exome sequencing: a systematic review of human essential genes Sarah M. Robbins1,2 & Matthew A. Thimm3 & David Valle1 & Angie C. Jelin4 Received: 18 December 2018 /Accepted: 29 May 2019 /Published online: 4 July 2019 # Springer Science+Business Media, LLC, part of Springer Nature 2019 Abstract Purpose Non-aneuploid recurrent pregnancy loss (RPL) affects approximately 100,000 pregnancies worldwide annually. Exome sequencing (ES) may help uncover the genetic etiology of RPL and, more generally, pregnancy loss as a whole. Previous studies have attempted to predict the genes that, when disrupted, may cause human embryonic lethality. However, predictions by these early studies rarely point to the same genes. Case reports of pathogenic variants identified in RPL cases offer another clue. We evaluated known genetic etiologies of RPL identified by ES. Methods We gathered primary research articles from PubMed and Embase involving case reports of RPL reporting variants identified by ES. Two authors independently reviewed all articles for eligibility and extracted data based on predetermined criteria. Preliminary and amended analysis isolated 380 articles; 15 met all inclusion criteria. Results These 15 articles described 74 families with 279 reported RPLs with 34 candidate pathogenic variants in 19 genes (NOP14, FOXP3, APAF1, CASP9, CHRNA1, NLRP5, MMP10, FGA, FLT1, EPAS1, IDO2, STIL, DYNC2H1, IFT122, PA DI6, CAPS, MUSK, NLRP2, NLRP7) and 26 variants of unknown significance in 25 genes. These genes cluster in four essential pathways: (1) gene expression, (2) embryonic development, (3) mitosis and cell cycle progression, and (4) inflammation and immunity. -

Variant Allele Frequency Enrichment Analysis in Vitro Reveals Sonic Hedgehog Pathway to Impede Sustained Temozolomide Response in GBM
OPEN Variant allele frequency enrichment SUBJECT AREAS: analysis in vitro reveals sonic hedgehog CNS CANCER CANCER GENOMICS pathway to impede sustained Received temozolomide response in GBM 22 September 2014 Nidhan K. Biswas1*, Vikas Chandra1*, Neeta Sarkar-Roy1, Tapojyoti Das1, Rabindra N. Bhattacharya2, Accepted Laxmi N. Tripathy3, Sunandan K. Basu3, Shantanu Kumar1, Subrata Das1, Ankita Chatterjee1, 22 December 2014 Ankur Mukherjee1, Pryiadarshi Basu1, Arindam Maitra1, Ansuman Chattopadhyay4, Analabha Basu1 Published & Surajit Dhara1 21 January 2015 1National Institute of Biomedical Genomics, Kalyani, West Bengal 741251, India, 2AMRI Hospitals, JC-16 Salt Lake City, Kolkata 700098, India, 3Medica Superspeciality Hospital, 127 Mukundapur, Kolkata 700099, India, 4University of Pittsburgh, 3550 Correspondence and Terrace Street, Pittsburgh, PA 15261, USA. requests for materials should be addressed to S.D. ([email protected]. Neoplastic cells of Glioblastoma multiforme (GBM) may or may not show sustained response to temozolomide (TMZ) chemotherapy. We hypothesize that TMZ chemotherapy response in GBM is in) or S.D. predetermined in its neoplastic clones via a specific set of mutations that alter relevant pathways. We (Surajit_dhara@ describe exome-wide enrichment of variant allele frequencies (VAFs) in neurospheres displaying hotmail.com) contrasting phenotypes of sustained versus reversible TMZ-responses in vitro. Enrichment of VAFs was found on genes ST5, RP6KA1 and PRKDC in cells showing sustained TMZ-effect whereas on genes FREM2, AASDH and STK36, in cells showing reversible TMZ-effect. Ingenuity pathway analysis (IPA) revealed that * These authors these genes alter cell-cycle, G2/M-checkpoint-regulation and NHEJ pathways in sustained TMZ-effect cells contributed equally to whereas the lysine-II&V/phenylalanine degradation and sonic hedgehog (Hh) pathways in reversible this work. -

Identification of Common Key Genes in Breast, Lung and Prostate Cancer and Exploration of Their Heterogeneous Expression
1680 ONCOLOGY LETTERS 15: 1680-1690, 2018 Identification of common key genes in breast, lung and prostate cancer and exploration of their heterogeneous expression RICHA K. MAKHIJANI1, SHITAL A. RAUT1 and HEMANT J. PUROHIT2 1Department of Computer Science and Engineering, Visvesvaraya National Institute of Technology, Nagpur, Maharashtra 440010; 2Environmental Genomics Division, National Environmental Engineering Research Institute, Nagpur, Maharashtra 440020, India Received March 8, 2017; Accepted October 20, 2017 DOI: 10.3892/ol.2017.7508 Abstract. Cancer is one of the leading causes of mortality cancer and may be used as biomarkers for the development of worldwide, and in particular, breast cancer in women, prostate novel diagnostic and therapeutic strategies. cancer in men, and lung cancer in both women and men. The present study aimed to identify a common set of genes which Introduction may serve as indicators of important molecular and cellular processes in breast, prostate and lung cancer. Six microarray The highest rates of cancer-related mortality are associated gene expression profile datasets [GSE45827, GSE48984, with breast, prostate and lung cancer, as reported by the World GSE19804, GSE10072, GSE55945 and GSE26910 (two Health Organization (1), the World Cancer Report (2) and datasets for each cancer)] and one RNA-Seq expression dataset Cancer facts and figures (3) A plethora of cancer microarray (GSE62944 including all three cancer types), were downloaded and RNA sequencing (RNA-Seq) studies are publicly avail- from the Gene Expression Omnibus database. Differentially able in databases, including the Gene Expression Omnibus expressed genes (DEGs) were identified in each individual (GEO) (4), Array Express (5) and The Cancer Genome Atlas cancer type using the LIMMA statistical package in R, and (TCGA; http://cancergenome.nih.gov/). -

Multivariate Meta-Analysis of Differential Principal Components Underlying Human Primed and Naive-Like Pluripotent States
bioRxiv preprint doi: https://doi.org/10.1101/2020.10.20.347666; this version posted October 21, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. This article is a US Government work. It is not subject to copyright under 17 USC 105 and is also made available for use under a CC0 license. October 20, 2020 To: bioRxiv Multivariate Meta-Analysis of Differential Principal Components underlying Human Primed and Naive-like Pluripotent States Kory R. Johnson1*, Barbara S. Mallon2, Yang C. Fann1, and Kevin G. Chen2*, 1Intramural IT and Bioinformatics Program, 2NIH Stem Cell Unit, National Institute of Neurological Disorders and Stroke, National Institutes of Health, Bethesda, Maryland 20892, USA Keywords: human pluripotent stem cells; naive pluripotency, meta-analysis, principal component analysis, t-SNE, consensus clustering *Correspondence to: Dr. Kory R. Johnson ([email protected]) Dr. Kevin G. Chen ([email protected]) 1 bioRxiv preprint doi: https://doi.org/10.1101/2020.10.20.347666; this version posted October 21, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. This article is a US Government work. It is not subject to copyright under 17 USC 105 and is also made available for use under a CC0 license. ABSTRACT The ground or naive pluripotent state of human pluripotent stem cells (hPSCs), which was initially established in mouse embryonic stem cells (mESCs), is an emerging and tentative concept. To verify this important concept in hPSCs, we performed a multivariate meta-analysis of major hPSC datasets via the combined analytic powers of percentile normalization, principal component analysis (PCA), t-distributed stochastic neighbor embedding (t-SNE), and SC3 consensus clustering. -

Dissertation
Aus dem Institut für Medizinische Genetik und Humangenetik der Medizinischen Fakultät Charité – Universitätsmedizin Berlin DISSERTATION Molecular genetic and cytogenetic analyses of autosomal recessive primary microcephaly (MCPH): Mouse model, new locus and novel mutations zur Erlangung des akademischen Grades Doctor of Philosophy in Medical Neurosciences (PhD in Medical Neurosciences) vorgelegt der Medizinischen Fakultät Charité – Universitätsmedizin Berlin Mahdi Ghani-Kakhki aus dem IRAN Gutachter: 1) Prof. Dr. K. Sperling 2) Prof. Dr. med. E. Schröck 3) Prof. Dr. med. E. Schwinger Datum der Promotion: 01.02.2013 Table of Contents Zusammenfassung ........................................................................................................................................ 4 Abstract ....................................................................................................................................................... 5 Introduction ................................................................................................................................................. 6 Aims of the PhD thesis .................................................................................................................................. 6 Hypotheses .................................................................................................................................................. 7 Methods...................................................................................................................................................... -

Molecular Genetics of Microcephaly Primary Hereditary: an Overview
brain sciences Review Molecular Genetics of Microcephaly Primary Hereditary: An Overview Nikistratos Siskos † , Electra Stylianopoulou †, Georgios Skavdis and Maria E. Grigoriou * Department of Molecular Biology & Genetics, Democritus University of Thrace, 68100 Alexandroupolis, Greece; [email protected] (N.S.); [email protected] (E.S.); [email protected] (G.S.) * Correspondence: [email protected] † Equal contribution. Abstract: MicroCephaly Primary Hereditary (MCPH) is a rare congenital neurodevelopmental disorder characterized by a significant reduction of the occipitofrontal head circumference and mild to moderate mental disability. Patients have small brains, though with overall normal architecture; therefore, studying MCPH can reveal not only the pathological mechanisms leading to this condition, but also the mechanisms operating during normal development. MCPH is genetically heterogeneous, with 27 genes listed so far in the Online Mendelian Inheritance in Man (OMIM) database. In this review, we discuss the role of MCPH proteins and delineate the molecular mechanisms and common pathways in which they participate. Keywords: microcephaly; MCPH; MCPH1–MCPH27; molecular genetics; cell cycle 1. Introduction Citation: Siskos, N.; Stylianopoulou, Microcephaly, from the Greek word µικρoκεϕαλi´α (mikrokephalia), meaning small E.; Skavdis, G.; Grigoriou, M.E. head, is a term used to describe a cranium with reduction of the occipitofrontal head circum- Molecular Genetics of Microcephaly ference equal, or more that teo standard deviations -
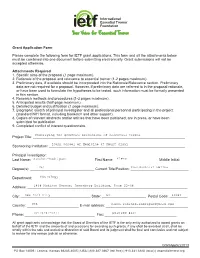
Grant Application Form Please Complete the Following Form for IETF
©2007 IETF Grant Application Form Please complete the following form for IETF grant applications. This form and all the attachments below must be combined into one document before submitting electronically. Grant submissions will not be accepted otherwise. Attachments Required 1. Specific aims of the proposal (1 page maximum). 2. Rationale of the proposal and relevance to essential tremor (1-2 pages maximum). 3. Preliminary data, if available should be incorporated into the Rationale/Relevance section. Preliminary data are not required for a proposal. However, if preliminary data are referred to in the proposal rationale, or have been used to formulate the hypotheses to be tested, such information must be formally presented in this section. 4. Research methods and procedures (1-2 pages maximum). 5. Anticipated results (half-page maximum). 6. Detailed budget and justification (1 page maximum). 7. Biographic sketch of principal investigator and all professional personnel participating in the project (standard NIH format, including biosketch and other support). 8. Copies of relevant abstracts and/or articles that have been published, are in press, or have been submitted for publication. 9. Completed conflict of interest questionnaire. Project Title: ____________________________________________________________________________ Sponsoring Institution: ____________________________________________________________________ Principal Investigator: Last Name: _______________________________ First Name: ______________________ Middle Initial: __ Degree(s): -

Proteomic Expression Profile in Human Temporomandibular Joint
diagnostics Article Proteomic Expression Profile in Human Temporomandibular Joint Dysfunction Andrea Duarte Doetzer 1,*, Roberto Hirochi Herai 1 , Marília Afonso Rabelo Buzalaf 2 and Paula Cristina Trevilatto 1 1 Graduate Program in Health Sciences, School of Medicine, Pontifícia Universidade Católica do Paraná (PUCPR), Curitiba 80215-901, Brazil; [email protected] (R.H.H.); [email protected] (P.C.T.) 2 Department of Biological Sciences, Bauru School of Dentistry, University of São Paulo, Bauru 17012-901, Brazil; [email protected] * Correspondence: [email protected]; Tel.: +55-41-991-864-747 Abstract: Temporomandibular joint dysfunction (TMD) is a multifactorial condition that impairs human’s health and quality of life. Its etiology is still a challenge due to its complex development and the great number of different conditions it comprises. One of the most common forms of TMD is anterior disc displacement without reduction (DDWoR) and other TMDs with distinct origins are condylar hyperplasia (CH) and mandibular dislocation (MD). Thus, the aim of this study is to identify the protein expression profile of synovial fluid and the temporomandibular joint disc of patients diagnosed with DDWoR, CH and MD. Synovial fluid and a fraction of the temporomandibular joint disc were collected from nine patients diagnosed with DDWoR (n = 3), CH (n = 4) and MD (n = 2). Samples were subjected to label-free nLC-MS/MS for proteomic data extraction, and then bioinformatics analysis were conducted for protein identification and functional annotation. The three Citation: Doetzer, A.D.; Herai, R.H.; TMD conditions showed different protein expression profiles, and novel proteins were identified Buzalaf, M.A.R.; Trevilatto, P.C. -

Acropectorovertebral Dysgenesis (F Syndrome)
213 LETTER TO JMG J Med Genet: first published as 10.1136/jmg.2003.014894 on 1 March 2004. Downloaded from Acropectorovertebral dysgenesis (F syndrome) maps to chromosome 2q36 H Thiele, C McCann, S van’t Padje, G C Schwabe, H C Hennies, G Camera, J Opitz, R Laxova, S Mundlos, P Nu¨rnberg ............................................................................................................................... J Med Genet 2004;41:213–218. doi: 10.1136/jmg.2003.014894 he F form of acropectorovertebral dysgenesis, also called F syndrome, is a rare dominantly inherited fully Key points Tpenetrant skeletal disorder.1 The name of the syndrome is derived from the first letter of the surname of the family in N Acropectorovertebral dysgenesis, also called F syn- which it was originally described. Major anomalies include drome, is a unique skeletal malformation syndrome, carpal synostoses, malformation of first and second fingers originally described in a four generation American with frequent syndactyly between these digits, hypoplasia family of European origin.1 The dominantly inherited and dysgenesis of metatarsal bones with invariable synostosis disorder is characterised by carpal and tarsal synos- of the proximal portions of the fourth and fifth metatarsals, toses, syndactyly between the first and the second variable degrees of duplication of distal portions of preaxial fingers, hypodactyly and polydactyly of feet, and toes, extensive webbing between adjacent toes, prominence abnormalities of the sternum and spine. of the sternum with variable pectus excavatum and spina bifida occulta of L3 or S1. Affected individuals also have N We have mapped F syndrome in the original family minor craniofacial anomalies and moderate impairment of and were able to localise the gene for F syndrome to a performance on psychometric tests.3 6.5 cM region on chromosome 2q36 with a maximum Two families have been reported to date. -

Investigation of Adiposity Phenotypes in AA Associated with GALNT10 & Related Pathway Genes
Investigation of Adiposity Phenotypes in AA Associated With GALNT10 & Related Pathway Genes By Mary E. Stromberg A Dissertation Submitted to the Graduate Faculty of WAKE FOREST UNIVERSITY GRADUATE SCHOOL OF ARTS AND SCIENCES in Partial Fulfillment of the Requirements for the Degree of DOCTOR OF PHILOSOPHY In Molecular Genetics and Genomics December 2018 Winston-Salem, North Carolina Approved by: Donald W. Bowden, Ph.D., Advisor Maggie C.Y. Ng, Ph.D., Advisor Timothy D. Howard, Ph.D., Chair Swapan Das, Ph.D. John P. Parks, Ph.D. Acknowledgements I would first like to thank my mentors, Dr. Bowden and Dr. Ng, for guiding my learning and growth during my years at Wake Forest University School of Medicine. Thank you Dr. Ng for spending so much time ensuring that I learn every detail of every protocol, and supporting me through personal difficulties over the years. Thank you Dr. Bowden for your guidance in making me a better scientist and person. I would like to thank my committee for their patience and the countless meetings we have had in discussing this project. I would like to say thank you to the members of our lab as well as the Parks lab for their support and friendship as well as their contributions to my project. Special thanks to Dean Godwin for his support and understanding. The umbrella program here at WFU has given me the chance to meet some of the best friends I could have wished for. I would like to also thank those who have taught me along the way and helped me to get to this point of my life, with special thanks to the late Dr. -

Transcriptomic and Epigenomic Characterization of the Developing Bat Wing
ARTICLES OPEN Transcriptomic and epigenomic characterization of the developing bat wing Walter L Eckalbar1,2,9, Stephen A Schlebusch3,9, Mandy K Mason3, Zoe Gill3, Ash V Parker3, Betty M Booker1,2, Sierra Nishizaki1,2, Christiane Muswamba-Nday3, Elizabeth Terhune4,5, Kimberly A Nevonen4, Nadja Makki1,2, Tara Friedrich2,6, Julia E VanderMeer1,2, Katherine S Pollard2,6,7, Lucia Carbone4,8, Jeff D Wall2,7, Nicola Illing3 & Nadav Ahituv1,2 Bats are the only mammals capable of powered flight, but little is known about the genetic determinants that shape their wings. Here we generated a genome for Miniopterus natalensis and performed RNA-seq and ChIP-seq (H3K27ac and H3K27me3) analyses on its developing forelimb and hindlimb autopods at sequential embryonic stages to decipher the molecular events that underlie bat wing development. Over 7,000 genes and several long noncoding RNAs, including Tbx5-as1 and Hottip, were differentially expressed between forelimb and hindlimb, and across different stages. ChIP-seq analysis identified thousands of regions that are differentially modified in forelimb and hindlimb. Comparative genomics found 2,796 bat-accelerated regions within H3K27ac peaks, several of which cluster near limb-associated genes. Pathway analyses highlighted multiple ribosomal proteins and known limb patterning signaling pathways as differentially regulated and implicated increased forelimb mesenchymal condensation in differential growth. In combination, our work outlines multiple genetic components that likely contribute to bat wing formation, providing insights into this morphological innovation. The order Chiroptera, commonly known as bats, is the only group of To characterize the genetic differences that underlie divergence in mammals to have evolved the capability of flight. -

A High Throughput, Functional Screen of Human Body Mass Index GWAS Loci Using Tissue-Specific Rnai Drosophila Melanogaster Crosses Thomas J
Washington University School of Medicine Digital Commons@Becker Open Access Publications 2018 A high throughput, functional screen of human Body Mass Index GWAS loci using tissue-specific RNAi Drosophila melanogaster crosses Thomas J. Baranski Washington University School of Medicine in St. Louis Aldi T. Kraja Washington University School of Medicine in St. Louis Jill L. Fink Washington University School of Medicine in St. Louis Mary Feitosa Washington University School of Medicine in St. Louis Petra A. Lenzini Washington University School of Medicine in St. Louis See next page for additional authors Follow this and additional works at: https://digitalcommons.wustl.edu/open_access_pubs Recommended Citation Baranski, Thomas J.; Kraja, Aldi T.; Fink, Jill L.; Feitosa, Mary; Lenzini, Petra A.; Borecki, Ingrid B.; Liu, Ching-Ti; Cupples, L. Adrienne; North, Kari E.; and Province, Michael A., ,"A high throughput, functional screen of human Body Mass Index GWAS loci using tissue-specific RNAi Drosophila melanogaster crosses." PLoS Genetics.14,4. e1007222. (2018). https://digitalcommons.wustl.edu/open_access_pubs/6820 This Open Access Publication is brought to you for free and open access by Digital Commons@Becker. It has been accepted for inclusion in Open Access Publications by an authorized administrator of Digital Commons@Becker. For more information, please contact [email protected]. Authors Thomas J. Baranski, Aldi T. Kraja, Jill L. Fink, Mary Feitosa, Petra A. Lenzini, Ingrid B. Borecki, Ching-Ti Liu, L. Adrienne Cupples, Kari E. North, and Michael A. Province This open access publication is available at Digital Commons@Becker: https://digitalcommons.wustl.edu/open_access_pubs/6820 RESEARCH ARTICLE A high throughput, functional screen of human Body Mass Index GWAS loci using tissue-specific RNAi Drosophila melanogaster crosses Thomas J.