Third National Survey on Iodine Deficiency Status in Sri Lanka - 2010
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Initial Environmental Examination
Initial Environmental Examination September 2014 SRI: Integrated Road Investment Program – Project 2 Sabaragamuwa Province Prepared by Environmental and Social Development Division, Road Development Authority, Ministry of Highways, Ports and Shipping for the Asian Development Bank CURRENCY EQUIVALENTS (as of 12 September 2014) Currency unit – Sri Lanka rupee (SLRe/SLRs) SLRe1.00 = $ 0.00767 $1.00 = SLR 130.300 ABBREVIATIONS ABC - Aggregate Base Coarse AC - Asphalt Concrete ADB - Asian Development Bank CBO - Community Based Organizations CEA - Central Environmental Authority DoF - Department of Forest DSDs - Divisional Secretary Divisions DOFC - Department of Forest Conservation DWLC - Department of Wild Life Conservation EC - Environmental Checklsit EIA - Environmental Impact Assessment EMP - Environmental Management Plan EPL - Environmental Protection License ESDD - Environmental and Social Development Division FBO - Farmer Based Organizations GoSL - Government of Sri Lanka GRC - Grievance Redress Committee GRM - Grievance Redress Mechanism GSMB - Geological Survey and Mines Bureau IEE - Initial Environmental Examination LAA - Land Acquisition Act MER - Manage Elephant Range MOHPS - Ministry of Highways, Ports and Shipping NAAQS - National Ambient Air Quality Standards NBRO - National Building Research Organization NEA - National Environmental Act NWS&DB- National Water Supply and Drainage Board OPRC - Output and Performance - based Road Contract PIC - Project Implementation Consultant PIU - Project Implementation Unit PRDA - Provincial Road Development Authority PS - Pradeshiya Sabha RDA - Road Development Authority ROW - Right of Way TOR - Terms of Reference NOTE In this report, "$" refers to US dollars unless otherwise stated. This initial environmental examination is a document of the borrower. The views expressed herein do not necessarily represent those of ADB's Board of Directors, Management, or staff, and may be preliminary in nature. -

The Household Water Usage Community Awareness Regarding
Original Article DOI: http://doi.org/10.4038/jmj.v32i1.90 The household water usage Community awareness regarding water pollution and factors associated with it among adult residents in MOH area, Uduvil 1Rajeev G , 2Murali V 1 RDHS Jaffna,2 Ministry of Health Abstract Introduction Introduction: Water pollution is a one of the Water is the driving force of nature and most public health burdens and the consumption of important natural resource that permeates all contaminated water has adverse health effects and aspects of the life on Earth. It is essential for even affects fetal development. The objective was human health and contributes to the sustainability to describe the household water usage pattern, of ecosystems. Safe water access and adequate community awareness of water pollution and sanitation are two basic determinants of good health factors associated with it among adult residents in (1). Both of these are important to protect people MOH area, Uduvil. from water related diseases like diarrhoeal diseases and typhoid (2). Method: A descriptive cross-sectional study was conducted on a community-based sample Clean drinking water is important for overall health of 817 adult residents with multi stage cluster and plays a substantial role in health of children sampling method. The data was collected by and their survival. Giving access to safe water is an interviewer administered questionnaire. one of the most effective ways to promote health Statistically significance for selected factors and and reduce poverty. All have the right to access awareness were analyzed with chi square and enough, continuous, safe, physically accessible, Mann-Whitney U test. -

Characterization of Irrigation Water Quality of Chunnakam Aquifer in Jaffna Peninsula
Tropical Agricultural Research Vol. 23 (3): 237 – 248 (2012) Characterization of Irrigation Water Quality of Chunnakam Aquifer in Jaffna Peninsula A. Sutharsiny, S. Pathmarajah1*, M. Thushyanthy2 and V. Meththika3 Postgraduate Institute of Agriculture University of Peradeniya Sri Lanka ABSTRACT. Chunnakam aquifer is the main lime stone aquifer of Jaffna Peninsula. This study focused on characterization of Chunnakam aquifer for its suitability for irrigation. Groundwater samples were collected from wells to represent different uses such as domestic, domestic with home garden, public wells and farm wells during January to April 2011. Important chemical parameters, namely electrical conductivity (EC), chloride, calcium, magnesium, carbonate, bicarbonate, sulfate, sodium and potassium were determined in water samples from 44 wells. Sodium percentage, Sodium adsorption ratio (SAR), and residual Sodium Carbonate (RSC) levels were calculated using standard equations to map the spatial variation of irrigation water quality of the aquifer using GIS. Groundwater was classified based on Chadha diagram and US salinity diagram. Two major hydro chemical facies Ca-Mg-Cl-SO4 and Na-Cl-SO4 were identified using Chadha diagram. Accordingly, it indicates permanent hardness and salinity problems. Based on EC, 16 % of the monitored wells showed good quality and 16 % showed unsuitable water for irrigation. Based on sodium percentage, 7 % has excellent and 23 % has doubtful irrigation water quality. However, according to SAR and RSC values, most of the wells have water good for irrigation. US salinity hazard diagram showed, 16 % as medium salinity and low alkali hazard. These groundwater sources can be used to irrigate all types of soils with little danger of increasing exchangeable sodium in soil. -
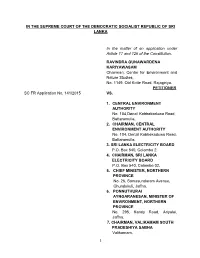
Documents in Support of Their Respective Positions
IN THE SUPREME COURT OF THE DEMOCRATIC SOCIALIST REPUBLIC OF SRI LANKA In the matter of an application under Article 17 and 126 of the Constitution. RAVINDRA GUNAWARDENA KARIYAWASAM Chairman, Centre for Environment and Nature Studies, No. 1149, Old Kotte Road, Rajagiriya. PETITIONER SC FR Application No. 141/2015 VS. 1. CENTRAL ENVIRONMENT AUTHORITY No. 104,Denzil Kobbekaduwa Road, Battaramulla. 2. CHAIRMAN, CENTRAL ENVIRONMENT AUTHORITY No. 104, Denzil Kobbekaduwa Road, Battaramulla. 3. SRI LANKA ELECTRICITY BOARD P.O. Box 540, Colombo 2. 4. CHAIRMAN, SRI LANKA ELECTRICITY BOARD P.O. Box 540, Colombo 02. 5. CHIEF MINISTER, NORTHERN PROVINCE No. 26, Somasundaram Avenue, Chundukuli, Jaffna. 6. PONNUTHURAI AYNGARANESAN, MINISTER OF ENVIRONMENT, NORTHERN PROVINCE No. 295, Kandy Road, Ariyalai, Jaffna. 7. CHAIRMAN, VALIKAMAM SOUTH PRADESHIYA SABHA Valikamam. 1 8. NORTHERN POWER COMPANY (PVT) LTD. No. 29, Castle Street, Colombo 10. 9. HON. ATTORNEY GENERAL Attorney General‟s Department, Colombo 12. 10. BOARD OF INVESTMENT OF SRI LANKA Level 26, West Tower, World Trade Center, Colombo 1. 11. NATIONAL WATER SUPPLY AND DRAINAGE BOARD P.O. Box 14, Galle Road, Mt. Lavinia. RESPONDENTS 1. DR. RAJALINGAM SIVASANGAR Chunnakam East, Chunnakam. 2. SINNATHURAI SIVAMAINTHAN Chunnakam East, Chunnakam. 3. SIVASAKTHIVEL SIVARATHEES Chunnakam East, Chunnakam. ADDED RESPONDENTS BEFORE: Priyantha Jayawardena, PC, J. Prasanna Jayawardena, PC, J. L.T.B. Dehideniya, J. COUNSEL: Nuwan Bopage with Chathura Weththasinghe for the Petitioner. Dr. Avanti Perera, SSC for the 1st to 4th, 9th, 10th and 11th Respondents. Dr. K.Kanag-Isvaran,PC with L.Jeyakumar instructed by M/S Sinnadurai Sundaralingam and Balendra for the 5th Respondent. Dinal Phillips,PC with Nalin Dissanayake and Pulasthi Hewamanne instructed by Ms. -

Sri Lanka: Health System Enhancement Project ABBREVIATIONS
Project Administration Manual Project Number: 51107-002 Loan and Grant Number: L3727 and G0618 April 2020 Sri Lanka: Health System Enhancement Project ABBREVIATIONS ADB Asian Development Bank AGD Auditor General’s Department APFS audited project financial statements ATR action taken report BCCM behavior change communication and community mobilization CBSL Central Bank of Sri Lanka CIGAS computerized integrated government accounting system DMF design and monitoring framework EARF environment assessment and review framework EGM effective gender mainstreaming EMP environment management plan EMR electronic medical record ERD Department of External Resources ERTU education, training and research unit ESP essential service package FHB Family Health Bureau FHC field health center FMA financial management assessment GAP gender action plan GBV gender-based violence GOSL Government of Sri Lanka HCWM healthcare waste management HIT health information technology HPB Health Promotion Bureau HRH human resources for health HSEP Health System Enhancement Project IEC information, education and communication IHR International Health Regulations MIS management information system MOFMM Ministry of Finance and Mass Media MOH medical officer of health MOHNIM Ministry of Health, Nutrition and Indigenous Medicine MOMCH medical officer maternal and child health NCD noncommunicable disease OCB open competitive bidding PBS patient based system PCC project coordination committee PCR project completion report PDHS provincial director health services PFM public financial management PHC primary health care PHI public health inspector PHM public health midwife PHN patient healthcare number PIU project implementation unit PMCU primary medical care unit PMU project management unit POE point of entry PPER project performance evaluation report PPTA project preparatory technical assistance PSC project steering committee QCBS quality- and cost-based selection RDHS regional director of health services SOE statement of expenditure TOT training of trainers CONTENTS I. -
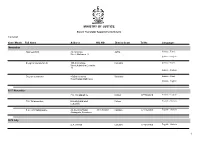
Name List of Sworn Translators in Sri Lanka
MINISTRY OF JUSTICE Sworn Translator Appointments Details 1/29/2021 Year / Month Full Name Address NIC NO District Court Tel No Languages November Rasheed.H.M. 76,1st Cross Jaffna Sinhala - Tamil Street,Ninthavur 12 Sinhala - English Sivagnanasundaram.S. 109,4/2,Collage Colombo Sinhala - Tamil Street,Kotahena,Colombo 13 Sinhala - English Dreyton senaratna 45,Old kalmunai Baticaloa Sinhala - Tamil Road,Kalladi,Batticaloa Sinhala - English 1977 November P.M. Thilakarathne Chilaw 0777892610 Sinhala - English P.M. Thilakarathne kirimathiyana East, Chilaw English - Sinhala Lunuwilla. S.D. Cyril Sadanayake 26, De silva Road, 331490350V Kalutara 0771926906 English - Sinhala Atabagoda, Panadura 1979 July D.A. vincent Colombo 0776738956 English - Sinhala 1 1/29/2021 Year / Month Full Name Address NIC NO District Court Tel No Languages 1992 July H.M.D.A. Herath 28, Kolawatta, veyangda 391842205V Gampaha 0332233032 Sinhala - English 2000 June W.A. Somaratna 12, sanasa Square, Gampaha 0332224351 English - Sinhala Gampaha 2004 July kalaichelvi Niranjan 465/1/2, Havelock Road, Colombo English - Tamil Colombo 06 2008 May saroja indrani weeratunga 1E9 ,Jayawardanagama, colombo English - battaramulla Sinhala - 2008 September Saroja Indrani Weeratunga 1/E/9, Jayawadanagama, Colombo Sinhala - English Battaramulla 2011 July P. Maheswaran 41/B, Ammankovil Road, Kalmunai English - Sinhala Kalmunai -2 Tamil - K.O. Nanda Karunanayake 65/2, Church Road, Gampaha 0718433122 Sinhala - English Gampaha 2011 November J.D. Gunarathna "Shantha", Kalutara 0771887585 Sinhala - English Kandawatta,Mulatiyana, Agalawatta. 2 1/29/2021 Year / Month Full Name Address NIC NO District Court Tel No Languages 2012 January B.P. Eranga Nadeshani Maheshika 35, Sri madhananda 855162954V Panadura 0773188790 English - French Mawatha, Panadura 0773188790 Sinhala - 2013 Khan.C.M.S. -

The 9Th Sri Lankan Junior Astronomy Olympiad Competition (SLJAO) -2019
The 9th Sri Lankan Junior Astronomy Olympiad Competition (SLJAO) -2019 Those who received marks above 50% will receive a GOLD(80-100), SILVER(70-79), BRONZE(60-69) MEDAL or a MERIT AWARD-CERTIFICATE(50-59). The award ceremony will be held on 2019.11.23 at 1.30 p.m. at the Colombo University premises (This will be notified by post to all medal winners) Merit Award Certificates will be sent by post on 2019.12.30 Index Number Name School City Normalised Medal/ Marks Award SLJAO9-C-S-0001 P.H.T. Dulmini Anula Vidyalaya Nugegoda 67 BRONZE SLJAO9-C-S-0002 W.M.P.T. Perera Aloysius College Rathnapura 38 SLJAO9-C-S-0003 N.N.Rajapaksha Kottawa Darmapala Vidyalaya Kottawa 46 SLJAO9-C-S-0004 M.M.S.V. Cooray Sri Palee College Horana 55 MERIT SLJAO9-C-S-0005 L.S.Kodagoda Lindsay Girls' School Colombo 03 40 SLJAO9-C-S-0006 M.T.U.I.Shamal Kuliyapitiya Central College Kuliyapitiya 37 SLJAO9-C-S-0007 K.A.G.Senesh Mahinda College Galle 80 GOLD SLJAO9-C-S-0008 J.M.S.S.Jayathilaka Kuliyapitiya Central College Kuliyapitiya 64 BRONZE SLJAO9-C-S-0009 S.A.C.H.Subasingha Kuliyapitiya Central College Kuliyapitiya 58 MERIT SLJAO9-C-S-0010 H.M.D.S.Bandara Central College Kuliyapitiya 65 BRONZE SLJAO9-C-S-0011 W.M.J.D.B.Wijekoon Ananda College Colombo 10 64 BRONZE SLJAO9-C-S-0012 L.P.A.M.Perera Mahanama College Colombo 03 46 SLJAO9-C-S-0013 N.P.Marasinghe Samudradevi Balika vidyalaya Nugegoda 46 SLJAO9-C-S-0014 H.S.D.Peiris Malabe Boys' Model School Malabe 57 MERIT SLJAO9-C-S-0015 W.M.R.N.Wickramanayake Central College Kuliyapitiya 70 SILVER SLJAO9-C-S-0016 W.K.A.G.Premachandra -

Tides of Violence: Mapping the Sri Lankan Conflict from 1983 to 2009 About the Public Interest Advocacy Centre
Tides of violence: mapping the Sri Lankan conflict from 1983 to 2009 About the Public Interest Advocacy Centre The Public Interest Advocacy Centre (PIAC) is an independent, non-profit legal centre based in Sydney. Established in 1982, PIAC tackles barriers to justice and fairness experienced by people who are vulnerable or facing disadvantage. We ensure basic rights are enjoyed across the community through legal assistance and strategic litigation, public policy development, communication and training. 2nd edition May 2019 Contact: Public Interest Advocacy Centre Level 5, 175 Liverpool St Sydney NSW 2000 Website: www.piac.asn.au Public Interest Advocacy Centre @PIACnews The Public Interest Advocacy Centre office is located on the land of the Gadigal of the Eora Nation. TIDES OF VIOLENCE: MAPPING THE SRI LANKAN CONFLICT FROM 1983 TO 2009 03 EXECUTIVE SUMMARY ....................................................................................................................... 09 Background to CMAP .............................................................................................................................................09 Report overview .......................................................................................................................................................09 Key violation patterns in each time period ......................................................................................................09 24 July 1983 – 28 July 1987 .................................................................................................................................10 -

Traditional Knowledge Systems and the Conservation and Management of Asia’S Heritage Rice Field in Bali, Indonesia by Monicavolpin (CC0)/Pixabay
ICCROM-CHA 3 Conservation Forum Series conservation and management of Asia’s heritage conservation and management of Asia’s Traditional Knowledge Systems and the Systems Knowledge Traditional ICCROM-CHA Conservation Forum Series Forum Conservation ICCROM-CHA Traditional Knowledge Systems and the conservation and management of Asia’s heritage Traditional Knowledge Systems and the conservation and management of Asia’s heritage Rice field in Bali, Indonesia by MonicaVolpin (CC0)/Pixabay. Traditional Knowledge Systems and the conservation and management of Asia’s heritage Edited by Gamini Wijesuriya and Sarah Court Forum on the applicability and adaptability of Traditional Knowledge Systems in the conservation and management of heritage in Asia 14–16 December 2015, Thailand Forum managers Dr Gamini Wijesuriya, Sites Unit, ICCROM Dr Sujeong Lee, Cultural Heritage Administration (CHA), Republic of Korea Forum advisors Dr Stefano De Caro, Former Director-General, ICCROM Prof Rha Sun-hwa, Administrator, Cultural Heritage Administration (CHA), Republic of Korea Mr M.R. Rujaya Abhakorn, Centre Director, SEAMEO SPAFA Regional Centre for Archaeology and Fine Arts Mr Joseph King, Unit Director, Sites Unit, ICCROM Kim Yeon Soo, Director International Cooperation Division, Cultural Heritage Administration (CHA), Republic of Korea Traditional Knowledge Systems and the conservation and management of Asia’s heritage Edited by Gamini Wijesuriya and Sarah Court ISBN 978-92-9077-286-6 © 2020 ICCROM International Centre for the Study of the Preservation and Restoration of Cultural Property Via di San Michele, 13 00153 Rome, Italy www.iccrom.org This publication is available in Open Access under the Attribution Share Alike 3.0 IGO (CCBY-SA 3.0 IGO) license (http://creativecommons.org/licenses/by-sa/3.0/igo). -

Urban Development Plan
Urban Development Plan (2018 – 2030) Urban Development Authority Sabaragamuwa Province Volume 01 RATNAPURA DEVELOPMENT PLAN VOLUME I Urban Development Authority “Sethsiripaya” Battaramulla 2018 - 2030 RATNAPURA DEVELOPMENT PLAN VOLUME I Urban Development Authority 2018 - 2030 Minister’s Foreword Local Authority Chairman’s Forward DOCUMENT INFORMATION Report Title : Ratnapura Development Plan Locational Boundary (Declared area) : Ratnapura Municipal Council Area Gazette No : Client / Stakeholder (Shortly) : Local residents of Ratnapura, Relevant Institutions, Commuters. Submission Date : 17/12/2018 Document Status : Final Document Submission Details Author UDA Ratnapura District Office Version No Details Date of Submission Approved for Issue 1 English Draft 07/12/2018 2 English Final 07/01/2019 This document is issued for the party which commissioned it and for specific purposes connected with the above-captioned project only. It should not be relied upon by any other party or used for any other purpose. We accept no responsibility for the consequences of this document being relied upon by any other party, or being used for any other purpose, or containing any error or omission which is due to an error or omission in data supplied to us by other parties. This document contains confidential information and proprietary intellectual property. It should not be shown to other parties without consent from the party which commissioned it. Preface This development plan has been prepared for the implementation of the development of Ratnapura Municipal Council area within next two decades. Ratnapura town is the capital of the Ratnapura District. The Ratnapura town has a population of approximately 49,083 and act as a regional center servicing the surrounding hinterland area and providing major services including administration, education and health. -

Wesley Times – November ’11
Wesley Times – November ’11 Newsletter of Wesley College Colombo Old Boys Union Australia Branch Inc. Message from the President IN THIS ISSUE From the Editor’s desk 2 Swimming Pool project 3 As 2011 draws to a close, it gives me Carol Service Notice 4 great satisfaction to reflect on yet another Condolences 5 Committee Contacts 5 great year for the “Wesley Family” in Membership renewal 5 Australia. There have been the usual Message from the Principal 6 activities that brought so many of us Dates to remember 7 together during the past 12 months and UK Branch Report 8 provided an opportunity for us to enjoy Seniors Lunch Notice 8 each other’s fellowship and add to the Where are they now? Amaresh Rajaratnam 9 good times that we seem to invariably Memories of Wesley have whenever we meet. The Double Blues and the 11 Blue , Gold and Blue I am very grateful to have had the total From the archives support of the terrific committee that we Wesley cricket 50 years 13 have, whose tireless efforts in organising ago Articles 16 all activities during the year are How famous cricketer recognised and appreciated. It is simply not what they do to Sathasivam was help the organisation, but the competent and enthusiastic way charged, tried and acquitted … in which they approach whatever the task which is most 17 appreciated. We have attempted to keep all our Old Boys Haleem Ishak – a tribute informed of the activities of the Association by way of personal Round the traps & in the News contact as well as the informative and regular newsletter that Class of 96 refurbish you would have continued to receive during 2011. -

Kalawana Gamini Central College
Site Specific Environmental and Social Management Plan (SSE & SMP) Site No. 14 Kalawana Gamini Central College Ratnapura District - Package 2 September 2018 Prepared for: Sri Lanka Landslide Mitigation Project Asia Infrastructure Investment Bank (AIIB) Prepared by: Environmental Studies and Services Division National Building Research Organization 99/1, Jawatta Rd Colombo 05 Tel: 011-2588946, 011-2503431, 011-22500354 Table of Contents 1. Introduction .......................................................................................................................................... 1 2. Location details and site description .................................................................................................... 1 3. Landslide hazard incident details ......................................................................................................... 2 4. Description of any remedial measures already undertaken to reduce the potential risk ...................... 4 5. Description of the area of the landslide and areas adjacent to the landslide and current level of risk . 4 6. Brief description on the surrounding environment with special reference to sensitive elements that may be affected by the project actions ................................................................................................. 5 7. Description of the works envisaged under the project ......................................................................... 5 8. Identification of social and environmental impacts and risks related to the