Policy 96018: Blepharoplasty, Blepharoptosis Repair, and Brow
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Blepharoplasty, Ptosis and Canthoplasty
ENVOLVE VISION BENEFITS, INC. INCLUDING ALL ASSOCIATED SUBSIDIARIES CLINICAL POLICY AND PROCEDURE DEPARTMENT: Utilization DOCUMENT NAME: Blepharoplasty, Ptosis Management and Canthoplasty PAGE: 1 of 8 REFERENCE NUMBER: OC.UM.CP.0007 EFFECTIVE DATE: 01/01/2017 REPLACES DOCUMENT: 118-UM-R6 RETIRED: REVIEWED: 10/25/2017 SPECIALIST REVIEW: Yes REVISED: 11/7/2016 PRODUCT TYPE: COMMITTEE APPROVAL: 01/09/2018 IMPORTANT REMINDER: This Clinical Policy has been developed by appropriately experienced and licensed health care professionals based on a thorough review and consideration of generally accepted standards of medical practice, peer-reviewed medical literature, government agency/program approval status, and other indicia of medical necessity. The purpose of this Clinical Policy is to provide a guide to medical necessity. Benefit determinations should be based in all cases on the applicable contract provisions governing plan benefits (“Benefit Plan Contract”) and applicable state and federal requirements including Local Coverage Determinations (LCDs), as well as applicable plan-level administrative policies and procedures. To the extent there are any conflicts between this Clinical Policy and the Benefit Plan Contract provisions, the Benefit Plan Contract provisions will control. Clinical policies are intended to be reflective of current scientific research and clinical thinking. This Clinical Policy is not intended to dictate to providers how to practice medicine, nor does it constitute a contract or guarantee regarding results. Providers are expected to exercise professional medical judgment in providing the most appropriate care, and are solely responsible for the medical advice and treatment of members. SUBJECT: Medical necessity determination of eyelid procedures for treatment of dermatochalasis and ptosis. -

T20 FUNCTIONAL UPPER EYELID BLEPHAROPLASTY Policy Author
Policy T20 Blepharoplasty THRESHOLD POLICY – T20 FUNCTIONAL UPPER EYELID BLEPHAROPLASTY Policy author: West Suffolk CCG and Ipswich and East Suffolk CCG, with support from Public Health Suffolk. Policy start date: January 2008 Subsequent reviews July 2012 September 2014 February 2017 Next review date: February 2020 1. Policy Summary 1.1 Blepharoplasty is considered a low priority treatment and will only be funded by Ipswich and East Suffolk CCG & West Suffolk CCG when the following criteria are met. It will not be funded for cosmetic reasons. 1.2 This policy doesn’t apply to anyone <19 years of age. 2. Eligibility Criteria 2.1 Upper eyelid blepharoplasty is considered medically necessary for the following indications: a) To repair defects predisposing to corneal or conjunctival irritation such as entropion or pseudotrichiasis. OR b) To treat periorbital sequelae of thyroid disease, nerve palsy, blepharochalasis, floppy eyelid syndrome and chronic inflammatory skin conditions. OR c) To relieve symptoms of blepharospasm or significant dermatitis on the upper eyelid caused by redundant tissue. OR d) Following skin grafting for eyelid reconstruction. OR e) At the same time as ptosis correction for the upper eyelid if the surplus skin is felt to be excess on lifting the ptotic eyelid 2.2 For all other individuals, the following criteria apply: a) Documented patient complaints of interference with vision or visual field related activities such as difficulty reading or driving due to upper eye lid skin drooping, looking through the eyelids or seeing the upper eye lid skin AND b) There is redundant skin overhanging the upper eye lid margin and resting on the eyelashes when gazing straight ahead AND S:\Clinical Quality\00 Chief Nursing Office\Clinical Oversight Group\POLICIES\T\Policies\T20 blepharoplasty\T20 Blepharoplasty E.docx 1 Policy T20 Blepharoplasty c) Supporting evidence from visual field testing that eyelids impinge on visual fields reducing field to 120° horizontally and/or 40° or less vertically. -

Eyelid Conjunctival Tumors
EYELID &CONJUNCTIVAL TUMORS PHOTOGRAPHIC ATLAS Dr. Olivier Galatoire Dr. Christine Levy-Gabriel Dr. Mathieu Zmuda EYELID & CONJUNCTIVAL TUMORS 4 EYELID & CONJUNCTIVAL TUMORS Dear readers, All rights of translation, adaptation, or reproduction by any means are reserved in all countries. The reproduction or representation, in whole or in part and by any means, of any of the pages published in the present book without the prior written consent of the publisher, is prohibited and illegal and would constitute an infringement. Only reproductions strictly reserved for the private use of the copier and not intended for collective use, and short analyses and quotations justified by the illustrative or scientific nature of the work in which they are incorporated, are authorized (Law of March 11, 1957 art. 40 and 41 and Criminal Code art. 425). EYELID & CONJUNCTIVAL TUMORS EYELID & CONJUNCTIVAL TUMORS 5 6 EYELID & CONJUNCTIVAL TUMORS Foreword Dr. Serge Morax I am honored to introduce this Photographic Atlas of palpebral and conjunctival tumors,which is the culmination of the close collaboration between Drs. Olivier Galatoire and Mathieu Zmuda of the A. de Rothschild Ophthalmological Foundation and Dr. Christine Levy-Gabriel of the Curie Institute. The subject is now of unquestionable importance and evidently of great interest to Ophthalmologists, whether they are orbital- palpebral specialists or not. Indeed, errors or delays in the diagnosis of tumor pathologies are relatively common and the consequences can be serious in the case of malignant tumors, especially carcinomas. Swift diagnosis and anatomopathological confirmation will lead to a treatment, discussed in multidisciplinary team meetings, ranging from surgery to radiotherapy. -

Involutional Type of Entropion in a Child with Cutis Laxa
1432 Br J Ophthalmol 2000;84:1432–1438 Br J Ophthalmol: first published as 10.1136/bjo.84.12.1432 on 1 December 2000. Downloaded from LETTERS TO THE EDITOR Involutional type of entropion in a child with cutis laxa EDITOR,—The diVuse elastic tissue disease called cutis laxa (CL) is a serious, even lethal systemic illness, involving not only the skin but connective tissues throughout the body.1 The skin hangs in loose folds, producing the appearance of premature ageing. Internal manifestations such as emphysema, ectasia of the aorta, and multiple hernias are usually present. We report a child with cutis laxa, who presented with an unusual ophthalmic mani- festation of the disease. CASE REPORT Our patient, who is nowa4yearoldboyand Figure 2 Eyelid tissue stained for elastic fibres showing marked granular degeneration of the elastic the third child to a normal first degree cousin fibres. Aldehyde-fuscin, ×400. couple, was noted to have redundant skin and a hoarse cry at the age of 3 months. Skin biopsy Surgical correction was carried out using a arrangements; hence the term “generalised was consistent with cutis laxa (elastin stain lateral tarsal strip in addition to two full elastolysis”. showed focal thickening of the elastic fibres thickness lid sutures. A small piece of resected Goltz and coworkers suggested an imbalance with tapered ends). His 7 month old sister was eyelid tissue was sent for pathological examina- between the circulating pancreatic elastase and also diagnosed as having cutis laxa at 3 months tion. its inhibitor (pancreatic elastase inhibiting sub- of age. Her ophthalmic examination revealed Staining for elastic tissue revealed marked stance, EIS), with a diminution of the latter in no abnormalities. -

Official Newsletter of APSOPRS 2016 Volume 2 Issue 4
Official Newsletter of APSOPRS 2016 Volume 2 Issue 4 Asia-Pacific Society of Ophthalmic Plastic and Reconstructive Surgery President Message: Hirohiko Kakizaki APSOPRS President Dear APSOPRS colleagues, Hirohiko Kakizaki (Japan) Season’s greetings during mid-summer! It has been 2 years since the new council APSOPRS Vice-Presidents started, and now at the last Hunter Yuen (Hong Kong, SAR) corner. Gangadhara Sundar (Singapore) The first thing we did was Kasturi Bhattacharjee (India) the move of the secretariat from Singapore to Japan. The most important matter was managing the members. At the time, the number of the official members were only 77, which means only Editor 77 members paid the fee to the society. The society Audrey Looi (Singapore) had 197 past (unpaid) members, though. I was very surprised at this reality as the APSOPRS is the representative society in this area and an affiliated Editorial Board society of APAO. In addition, the APSOPRS has been a reciprocal society of the ASOPRS. This matter was Ashok Grover (India) simply caused by the bothersome payment system. We before had only two methods of payment: one Kelvin Chong (Hong Kong, SAR) was the direct payment at a conference venue and Yoon-Duck, Kim (South Korea) the other was via bank transfer, the latter of which needs a complicated procedure. We therefore Lily Li Dong Mei (China) simplified the payment system using the Paypal via Raoul Henson (Philippines) web. As a result, the number of the paying members has increased to 112 by now. This is not Sunny Shen (Singapore) enough, of course, so please invite your colleagues and try to catch up with the ASOPRS and ESOPRS! In relation to this membership management, we have launched the “life membership” system. -

Eleventh Edition
SUPPLEMENT TO April 15, 2009 A JOBSON PUBLICATION www.revoptom.com Eleventh Edition Joseph W. Sowka, O.D., FAAO, Dipl. Andrew S. Gurwood, O.D., FAAO, Dipl. Alan G. Kabat, O.D., FAAO Supported by an unrestricted grant from Alcon, Inc. 001_ro0409_handbook 4/2/09 9:42 AM Page 4 TABLE OF CONTENTS Eyelids & Adnexa Conjunctiva & Sclera Cornea Uvea & Glaucoma Viitreous & Retiina Neuro-Ophthalmic Disease Oculosystemic Disease EYELIDS & ADNEXA VITREOUS & RETINA Blow-Out Fracture................................................ 6 Asteroid Hyalosis ................................................33 Acquired Ptosis ................................................... 7 Retinal Arterial Macroaneurysm............................34 Acquired Entropion ............................................. 9 Retinal Emboli.....................................................36 Verruca & Papilloma............................................11 Hypertensive Retinopathy.....................................37 Idiopathic Juxtafoveal Retinal Telangiectasia...........39 CONJUNCTIVA & SCLERA Ocular Ischemic Syndrome...................................40 Scleral Melt ........................................................13 Retinal Artery Occlusion ......................................42 Giant Papillary Conjunctivitis................................14 Conjunctival Lymphoma .......................................15 NEURO-OPHTHALMIC DISEASE Blue Sclera .........................................................17 Dorsal Midbrain Syndrome ..................................45 -

Freedman Eyelid Abnormalities
1/16/2018 1 1/16/2018 Upper Lid Lower Lid Protractors Retractors: Levator m. 3rd nerve function Muller’s m. Cranial Nerve VII function Sympathetic Function Inferior Tarsal Muscle Things to Note Lid Apposition to Globe Position of Lid Margins MRD = 3‐5 mm Canthal Insertions Brow Positions 2 1/16/2018 Ptosis Usually age related levator dehiscence, but sometimes a sign of neurologic, mechanical orbital or inflammatory disease Blepharospasm Sign of External Irritation or Neurologic Disease 3 1/16/2018 First Consider Underlying Orbital Disease Orbital Cellulitis, Pseudotumor, Wegener’s Graves Ophthalmopathy, Orbital Varix Orbital Tumors that can mimic inflammatory process: Lacrimal Gland CA, Lymphoma, Lymphangioma, etc. Lacrimal Gland – Dacryoadenitis or tumor Sinus Mucocele Without Inflammatory Appearance, consider above but also… Allergic Eyelid Edema Hormonal Shifts Systemic Disorder – Cardiac, Renal, Hepatic, Thyroid with edema Cutaneous Lymphoma Graves Ophthalmopathy –can just have lid edema w/o inflammatory appearance Lymphedema after trauma, surgery to lids or orbit (e.g. lymphatics in lateral canthus) Traumatic Leak of CSF into upper eyelid (JAMA Oph 2014;312:1485) Blepharochalasis Not True Edema, but might mimic it: Dermatochalasis, Hidden Eyelid or Sub‐Conjunctival Mass, Prolapsed Orbital Fat When your concerned about: Orbital Cellulitis Orbital Pseudotumor Orbital Malignancy Vascular – e.g. CC fistula Proptosis Chemosis Poor Motility Poor Vision Pupil abnormality – e.g. RAPD Orbital Pseudotumor 4 1/16/2018 Good Vision Good Motility -

Involutional Lateral Entropion of the Upper Eyelids a New Physical Finding in Asian Patients
CLINICAL SCIENCES Involutional Lateral Entropion of the Upper Eyelids A New Physical Finding in Asian Patients Jorge G. Camara, MD; Ly T. Nguyen, MD; Marither Sangalang-Chuidian, MD; Jesus N. Ong, MD; Jessica P. Fernandez-Suntay, MD; Ronald B. Zabala, MD; Roderick B. D. Domondon, MD Objective: To describe a new physical finding called in- the lateral aspect of the upper eyelid bilaterally. The pre- volutional lateral entropion (ILE) of the upper eyelid senting symptoms were foreign-body sensation (85%), found in Asian patients. tearing (77%), eye redness (34%), eye pain (26%), and itchiness at the lateral canthal area (25%). Clinical find- Methods: A prospective case series study of 53 con- ings included lateral dermatochalasis (100%), trichiasis secutive patients with ILE of the upper eyelid, from the (100%), lateral canthal eyelid laxity (100%), localized lat- practice of one of the authors (J.G.C.), was performed. eral conjunctivitis (42%), punctate epithelial keratopa- All of the patients in this series were Asian. Clinical find- thy (11%), blepharitis (11%), and distichiasis (8%). ings on ocular examination, symptoms, age, and sex were obtained and tabulated. Conclusion: We describe ILE of the upper eyelid in Asian patients and explain the anatomic correlates respon- Results: The mean±SD age of patients was 68.9±10.1 sible for this condition. years (range, 41-88 years); 70% were women and 30% were men. All patients presented with in-turning of only Arch Ophthalmol. 2002;120:1682-1684 CCORDING TO Dryden and Asian patients as young as in the fifth Doxanas1 and Fox,2 invo- decade of life. -

Mythbusters All Droopy Eyelids Are Created Equal
Financial disclosures Mythbusters Oculoplastic Edition Jed T. Poll, M.D. Utah Optometric Association June 3, 2016 Myth #1 Seriously…They’re all the same • Causes of “Droopy Eyelids” • Dermatochalasis All droopy • Blepharoptosis • Brow ptosis eyelids are • Pseudoptosis created equal I’m still not convinced… Different kinds-o-ptosis? Most common Usually congenital Dermatochalasis Ptosis Stretched tendon Weak muscle Excess skin problem Eyelid muscle problem High lid crease Absent lid crease Weighs down eyelid Lid margin / lashes low Involutional Myogenic Normal lid function Possible lid dysfunction Uncommon Uncommon Myasthenia / Botox Lesion / Mass Fluctuating Treat mass effect Many patients have both Neurogenic Mechanical 1 So…They’re not all the same Myth #1 • Correct Dx = Correct treatment – Not always surgical • Potential comorbidities All droopy – Droopy lid with… eyelids are • Anisocoria - Horner’s syndrome / CN III palsy • Fluctuations - Myasthenia Gravis created equal Myth #2 Will my insurance cover this? • Most common question for dermato and ptosis • 3 Elements: All eyelid – Complaint of visual impairment that improves with eyelid elevation surgery is – Supported by clinical exam – Documented with clinical photographs and cosmetic taped/untaped visual fields Dermatochalasis Evaluation Ptosis Evaluation • Exam: PF: lid margin to lid margin – “Grading” the amount of dermatochalasis MRD: light reflex to lid margin • 1+ to 4+ scale or mild to severe 1+ 2+ 3+ 4+ Dermatochalasis continuum Barely any Barely seeing 2 Ptosis Evaluation -

Blepharoplasty Fact Sheet
FACT Blepharoplasty SHEET LCD L33944 Medicare does not cover cosmetic surgery or expenses Any procedure(s) involving blepharoplasty and billed to this contractor MUST be supported by incurred in connection with documented patient complaints which justify functional surgery. such surgery. This exclusion This documentation must address the signs and symptoms commonly found in association does not appy to surgery in with ptosis, pseudoptosis, blepharochalasis and/or dermatochalasis. connection with the treatment These include, but are not limited to: of an accidental injury or for the improvement of the • Significant interference with vision or superior or lateral visual field (i.e.. difficulty seeing functioning of a malformed objects approaching from the periphery) body member. (CMS • Difficulty reading due to superior visual field loss Publication 100-2, chapter • Looking through the eyelashes or seeing the upper eyelid skin 16, section 120, http://www. cms.gov/Regulations-and- Guidance/Guidance/Manuals/ Downloads/bp102c16.pdf) Visual Field Testing • Demonstrate a significant loss of superior visual field and potential correction of the visual field by the proposed procedure(s). • A minimum 12 degree OR 30 percent loss of upper field of vision with upper lid skin and/ or upper lid margin in repose and elevated (by taping of the lid) to demonstrate potential correction by the proposed procedure or procedures is required. • Testing of eye(s) both at rest and with lid elevation (taped, manually retracted) • When planned procedure is for ptosis or the ptosis is concurrent with dermatochalasis; the visual field study should be repeated with the true eyelid taped, so the eyelid margin assumes the correct anatomic position • Include Patient name, date of testing and eye(s) tested • When both eyes are tested the test MUST clearly distinguish right (OD) from left (OS) Visual field studies are not required when the indication for surgery is entropion or extropion. -
Local Coverage Determination for Blepharoplasty (L33944)
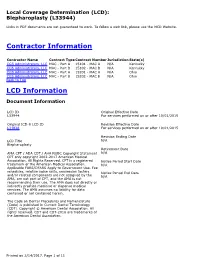
Local Coverage Determination (LCD): Blepharoplasty (L33944) Links in PDF documents are not guaranteed to work. To follow a web link, please use the MCD Website. Contractor Information Contractor Name Contract Type Contract Number Jurisdiction State(s) CGS Administrators, LLC MAC - Part A 15101 - MAC A N/A Kentucky CGS Administrators, LLC MAC - Part B 15102 - MAC B N/A Kentucky CGS Administrators, LLC MAC - Part A 15201 - MAC A N/A Ohio CGS Administrators, LLC MAC - Part B 15202 - MAC B N/A Ohio Back to Top LCD Information Document Information LCD ID Original Effective Date L33944 For services performed on or after 10/01/2015 Original ICD-9 LCD ID Revision Effective Date L31828 For services performed on or after 10/01/2015 Revision Ending Date LCD Title N/A Blepharoplasty Retirement Date AMA CPT / ADA CDT / AHA NUBC Copyright Statement N/A CPT only copyright 2002-2017 American Medical Association. All Rights Reserved. CPT is a registered Notice Period Start Date trademark of the American Medical Association. N/A Applicable FARS/DFARS Apply to Government Use. Fee schedules, relative value units, conversion factors Notice Period End Date and/or related components are not assigned by the N/A AMA, are not part of CPT, and the AMA is not recommending their use. The AMA does not directly or indirectly practice medicine or dispense medical services. The AMA assumes no liability for data contained or not contained herein. The Code on Dental Procedures and Nomenclature (Code) is published in Current Dental Terminology (CDT). Copyright © American Dental Association. All rights reserved. -

Sleep Apnea and the Eyelids Pathogenesis
3/14/2016 SLEEP APNEA AND THE EYELIDS Sara Nonhof, O.D. Floppy Eyelid Syndrome First described in 1981 Definition: • easily everted eyelids • chronic papillary conjunctivitis • found in obese, milddle-aged men Leibovitch I, Selva D. Floppy eyelid syndrome: clinical features and the association with obstructive sleep apnea. Sleep Medicine. 2006;7:117-22 PATHOGENESIS Mechanical theory Decreased tarsal elastin Lid laxity Tear film abnormalities/Meibomianitis Chronic inflammation Alterations in collagen http://utahoc.com/floppy-eyelid-syndrome-sleep-apnea/ 1 3/14/2016 OCULAR ASSOCIATIONS Eyelids Conjunctiva Cornea Glaucoma OCULAR ASSOCIATIONS: EYELIDS Function: protect ocular surface Become easily distorted and everted http://www.drvisionworld.com/demodex-infestation/ Other pathologies reported Ptosis Dermatochalasis Blepharochalasis Upper lid lash ptosis Entropion/Ectropion Blepharitis, Meibomianitis, Demodex http://optometrist.com.au/blepharochalasis/ OCULAR ASSOCIATIONS: CONJUNCTIVA Chronic papillary conjunctivitis Hallmark sign Epithelial and stromal changes are non-specific May delay in diagnosis http://www.improveeyesighthq.com/giant-papillary-conjunctivitis.html 2 3/14/2016 OCULAR ASSOCIATIONS: CORNEA Punctate epithelial keratopathy Most common finding Diffuse Typically only involves affected eye Keratoconus Study published in Cornea in May 2015 FES patients have lower CH values http://www.djo.harvard.edu/print.php?url=/physicians/oa/779 Subepithelial scarring Deep neovascularization OCULAR ASSOCIATIONS: