Invasive Disease Due to Mucorales: a Case Report and Review of The
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Plant Life MagillS Encyclopedia of Science
MAGILLS ENCYCLOPEDIA OF SCIENCE PLANT LIFE MAGILLS ENCYCLOPEDIA OF SCIENCE PLANT LIFE Volume 4 Sustainable Forestry–Zygomycetes Indexes Editor Bryan D. Ness, Ph.D. Pacific Union College, Department of Biology Project Editor Christina J. Moose Salem Press, Inc. Pasadena, California Hackensack, New Jersey Editor in Chief: Dawn P. Dawson Managing Editor: Christina J. Moose Photograph Editor: Philip Bader Manuscript Editor: Elizabeth Ferry Slocum Production Editor: Joyce I. Buchea Assistant Editor: Andrea E. Miller Page Design and Graphics: James Hutson Research Supervisor: Jeffry Jensen Layout: William Zimmerman Acquisitions Editor: Mark Rehn Illustrator: Kimberly L. Dawson Kurnizki Copyright © 2003, by Salem Press, Inc. All rights in this book are reserved. No part of this work may be used or reproduced in any manner what- soever or transmitted in any form or by any means, electronic or mechanical, including photocopy,recording, or any information storage and retrieval system, without written permission from the copyright owner except in the case of brief quotations embodied in critical articles and reviews. For information address the publisher, Salem Press, Inc., P.O. Box 50062, Pasadena, California 91115. Some of the updated and revised essays in this work originally appeared in Magill’s Survey of Science: Life Science (1991), Magill’s Survey of Science: Life Science, Supplement (1998), Natural Resources (1998), Encyclopedia of Genetics (1999), Encyclopedia of Environmental Issues (2000), World Geography (2001), and Earth Science (2001). ∞ The paper used in these volumes conforms to the American National Standard for Permanence of Paper for Printed Library Materials, Z39.48-1992 (R1997). Library of Congress Cataloging-in-Publication Data Magill’s encyclopedia of science : plant life / edited by Bryan D. -

Zygomycosis Caused by Cunninghamella Bertholletiae in a Kidney Transplant Recipient
Medical Mycology April 2004, 42, 177Á/180 Case report Zygomycosis caused by Cunninghamella bertholletiae in a kidney transplant recipient D. QUINIO*, A. KARAM$, J.-P. LEROY%, M.-C. MOAL§, B. BOURBIGOT§, O. MASURE*, B. SASSOLAS$ & A.-M. LE FLOHIC* Departments of *Microbiology, $Dermatology, %Pathology and §Kidney Transplantation, Brest University Hospital Brest France Downloaded from https://academic.oup.com/mmy/article/42/2/177/964345 by guest on 23 September 2021 Infections caused by Cunninghamella bertholletiae are rare but severe. Only 32 cases have been reported as yet, but in 26 of these this species was a contributing cause of the death of the patient. This opportunistic mould in the order Mucorales infects immunocompromized patients suffering from haematological malignancies or diabetes mellitus, as well as solid organ transplant patients. The lung is the organ most often involved. Two cases of primary cutaneous infection have been previously reported subsequent to soft-tissue injuries. We report a case of primary cutaneous C. bertholletiae zygomycosis in a 54-year-old, insulin-dependent diabetic man who was treated with tacrolimus and steroids after kidney transplantation. No extracutaneous involvement was found. In this patient, the infection may have been related to insulin injections. The patient recovered after an early surgical excision of the lesion and daily administration of itraconazole for 2 months. This case emphasizes the importance of an early diagnosis of cutaneous zygomycosis, which often presents as necrotic-looking lesions. Prompt institution of antifungal therapy and rapid surgical intervention are necessary to improve the prospects of patients who have contracted these potentially severe infections. Keywords Cunninghamella bertholletiae, cutaneous zygomycosis, diabetes mellitus, kidney transplantation Introduction sub-tropical areas. -

Syzygites Megalocarpus (Mucorales, Zygomycetes) in Illinois
Transactions of the Illinois State Academy of Science received 12/8/98 (1999), Volume 92, 3 and 4, pp. 181-190 accepted 6/2/99 Syzygites megalocarpus (Mucorales, Zygomycetes) in Illinois R. L. Kovacs1 and W. J. Sundberg2 Department of Plant Biology, Mail Code 6509 Southern Illinois University at Carbondale Carbondale, Illinois 62901-6509 1Current Address: Salem Academy; 942 Lancaster Dr. NE; Salem, OR 97301 2Corresponding Author ABSTRACT Syzygites megalocarpus Ehrenb.: Fr. (Mucorales, Zygomycetes), which occurs on fleshy fungi and was previously unreported from Illinois, has been collected from five counties- -Cook, Gallatin, Jackson, Union, and Williamson. In Illinois, S. megalocarpus occurs on 23 species in 18 host genera. Fresh host material collected in the field and appearing uninfected can develop S. megalocarpus colonies after incubation in the laboratory. The ability of S. megalocarpus to colonize previously uninfected hosts was demonstrated by inoculation studies in the laboratory. Because the known distribution of potential hosts in Illinois is much broader than documented here, further attention to S. megalocarpus should more fully elucidate the host and geographic ranges of this Zygomycete in the state. Using light and scanning electron microscopy, the heretofore unmeasured warts on the zygosporangium were 4-6 µm broad and 5-8 µm high, providing additional informa- tion for circumscription of this genus. INTRODUCTION Syzygites (Mucorales, Zygomycetes) is a presumptive mycoparasite that occurs on fleshy fungi (Figs. 1-2) and contains a single species, S. megalocarpus Ehrenb.: Fr. (Hesseltine 1957). It is homothallic and forms erect sporangiophores which are dichotomously branched and bear columellate, multispored sporangia at their apices (Fries 1832, Hes- seltine 1957, Benny and O'Donnell 1978, O'Donnell 1979). -

Epidemiological Alert: COVID-19 Associated Mucormycosis
Epidemiological Alert: COVID-19 associated Mucormycosis 11 June 2021 Given the potential increase in cases of COVID-19 associated mucormycosis (CAM) in the Region of the Americas, the Pan American Health Organization / World Health Organization (PAHO/WHO) recommends that Member States prepare health services in order to minimize morbidity and mortality due to CAM. Introduction In recent months, an increase in reports of cases of Mucormycosis (previously called zygomycosis) is the term used to name invasive fungal infections (IFI) COVID-19 associated Mucormycosis (CAM) has caused by saprophytic environmental fungi, been observed mainly in people with underlying belonging to the subphylum Mucoromycotina, order diseases, such as diabetes mellitus (DM), diabetic Mucorales. Among the most frequent genera are ketoacidosis, or on steroids. In these patients, the Rhizopus and Mucor; and less frequently Lichtheimia, most frequent clinical manifestation is rhino-orbital Saksenaea, Rhizomucor, Apophysomyces, and Cunninghamela (Nucci M, Engelhardt M, Hamed K. mucormycosis, followed by rhino-orbital-cerebral Mucormycosis in South America: A review of 143 mucormycosis, which present as secondary reported cases. Mycoses. 2019 Sep;62(9):730-738. doi: infections and occur after SARS CoV-2 infection. 1,2 10.1111/myc.12958. Epub 2019 Jul 11. PMID: 31192488; PMCID: PMC6852100). Globally, the highest number of cases has been The infection is acquired by the implantation of the reported in India, where it is estimated that there spores of the fungus in the oral, nasal, and are more than 4,000 people with CAM.3 conjunctival mucosa, by inhalation, or by ingestion of contaminated food, since they quickly colonize foods rich in simple carbohydrates. -

Isolation of Mucorales from Biological Environment and Identification of Rhizopus Among the Isolates Using PCR- RFLP
Journal of Shahrekord University of Medical Sciences doi:10.34172/jsums.2019.17 2019;21(2):98-103 http://j.skums.ac.ir Original Article Isolation of Mucorales from biological environment and identification of Rhizopus among the isolates using PCR- RFLP Mahboobeh Madani1* ID , Mohammadali Zia2 ID 1Department of Microbiology, Falavarjan Branch, Islamic Azad University, Isfahan, Iran 2Department of Basic Science, (Khorasgan) Isfahan Branch, Islamic Azad University, Isfahan, Iran *Corresponding Author: Mahboobeh Madani, Tel: + 989134097629, Email: [email protected] Abstract Background and aims: Mucorales are fungi belonging to the category of Zygomycetes, found much in nature. Culture-based methods for clinical samples are often negative, difficult and time-consuming and mainly identify isolates to the genus level, and sometimes only as Mucorales. Therefore, applying fast and accurate diagnosis methods such as molecular approaches seems necessary. This study aims at isolating Mucorales for determination of Rhizopus genus between the isolates using molecular methods. Methods: In this descriptive observational study, a total of 500 samples were collected from air and different surfaces and inoculated on Sabouraud Dextrose Agar supplemented with chloramphenicol. Then, the fungi belonging to Mucorales were identified and their pure culture was provided. DNA extraction was done using extraction kit and the chloroform method. After amplification, the samples belonging to Mucorales were identified by observing 830 bp bands. For enzymatic digestion, enzyme BmgB1 was applied for identification of Rhizopus species by formation of 593 and 235 bp segments. Results: One hundred pure colonies belonging to Mucorales were identified using molecular methods and after enzymatic digestion, 21 isolates were determined as Rhizopus species. -

Jemds.Com Original Research Article
Jemds.com Original Research Article PATHOGENIC FUNGAL CONTAMINATION OF MUNICIPAL DUMPING YARD, KOTTAYAM AND RELATED HEALTH EFFECTS Vipinunni1, Bernaitis L2, Sabarianand3, Preesly M. S4, Revathi P. Shenoy5 1Lecturer, RVS Dental College, Coimbatore. 2Lecturer, RVS Dental College, Coimbatore. 3Lecturer, Mahatma Gandhi Medical College, Pondicherry. 4Lecturer, RVS Siddha Medical College & Hospital, Coimbatore. 5Associate Professor, Kasturba Medical College, Manipal. ABSTRACT BACKGROUND Fungi are ubiquitous soil saprophytes often involved in various human ailments. Fungal diseases are emerging worldwide. However, the mycological health risks associated with dumping yard is not much investigated, especially from developing countries where such sites are very common. Aims and Objectives- The major objective of the study was to analyse the possible mycological threat posed by the municipal dumping yard. The study also aims to assess the health status of interacting community in relation to the dumping yard. MATERIALS AND METHODS A descriptive study was conducted from April to June 2015 in Kottayam Municipal dumping yard at Vadavathoor. Two set of soil samples, a total of 50 from the dumping yard were collected, before and after burning of the dumping yard. One set of samples from leachate and neighbouring open wells were collected after burning of the dumping yard. Samples were collected in sterile containers and transported immediately to the laboratory. The samples were cultured on to suitable fungal culture medium and the growths of the fungus were identified by the microscopic and macroscopic features. RESULTS The isolated fungal pathogens from the soil shows that 49% isolates belonged to the Aspergillus genus; and the remaining 51% was almost equally shared by four other different species Geotrichum, Humicola, Microsporum, Rhizopus. -

Saksenaea Vasiformis Causing Cutaneous Zygomycosis: an Experience from Tertiary Care Hospital in Mumbai Microbiology Section Microbiology
DOI: 10.7860/JCDR/2018/33895.11720 Original Article Saksenaea vasiformis Causing Cutaneous Zygomycosis: An Experience from Tertiary Care Hospital in Mumbai Microbiology Section Microbiology SHASHIR WASUDEORAO WANJARE1, SULMAZ FAYAZ RESHI2, PREETI RAJIV MEHTA3 ABSTRACT was retrieved from medical records department. Diagnosis of Introduction: Zygomycosis, a fungal infection caused by a zygomycosis was based on 10% Potassium Hydroxoide (KOH) group of filamentous fungi, Zygomycetes. Zygomycetes belong examination, culture on Sabouraud’s Dextrose Agar (SDA), to orders Mucorales and Entomorphthorales. Infection occurs identification of fungus by slide culture, Lactophenol Cotton in rhinocerebral, pulmonary, cutaneous, abdominal, pelvic and Blue (LPCB) mount and Water Agar method. disseminated forms. Cutaneous zygomycosis is the third most Results: In the present study, seven cases of cutaneous common presentation, usually occurring as gradual and slowly Zygomycosis caused by emerging pathogen Saksenaea progressive disease but may sometimes become fulminant vasiformis were studied. On analysing these cases, it was found leading to necrotizing lesion and haematogenous dissemination. that break in the skin integrity predisposes to infection. Two Infection caused by Saksenaea vasiformis is rare but are patients were known cases of Diabetes mellitus, while five of emerging pathogens having a tendency to cause infection even them had no underlying associated medical conditions. This in immunocompetent hosts. study shows that although infection with Saksenaea vasiformis Aim: To analyse cases of cutaneous zygomycosis caused is more common in immunocompromised patients but a healthy by Saksenaea vasiformis with respect to risk factors, clinical individuals can be infected and may have a bad prognosis if presentation, causative agents, management and patient diagnosis and treatment is delayed. -

New Species and Changes in Fungal Taxonomy and Nomenclature
Journal of Fungi Review From the Clinical Mycology Laboratory: New Species and Changes in Fungal Taxonomy and Nomenclature Nathan P. Wiederhold * and Connie F. C. Gibas Fungus Testing Laboratory, Department of Pathology and Laboratory Medicine, University of Texas Health Science Center at San Antonio, San Antonio, TX 78229, USA; [email protected] * Correspondence: [email protected] Received: 29 October 2018; Accepted: 13 December 2018; Published: 16 December 2018 Abstract: Fungal taxonomy is the branch of mycology by which we classify and group fungi based on similarities or differences. Historically, this was done by morphologic characteristics and other phenotypic traits. However, with the advent of the molecular age in mycology, phylogenetic analysis based on DNA sequences has replaced these classic means for grouping related species. This, along with the abandonment of the dual nomenclature system, has led to a marked increase in the number of new species and reclassification of known species. Although these evaluations and changes are necessary to move the field forward, there is concern among medical mycologists that the rapidity by which fungal nomenclature is changing could cause confusion in the clinical literature. Thus, there is a proposal to allow medical mycologists to adopt changes in taxonomy and nomenclature at a slower pace. In this review, changes in the taxonomy and nomenclature of medically relevant fungi will be discussed along with the impact this may have on clinicians and patient care. Specific examples of changes and current controversies will also be given. Keywords: taxonomy; fungal nomenclature; phylogenetics; species complex 1. Introduction Kingdom Fungi is a large and diverse group of organisms for which our knowledge is rapidly expanding. -
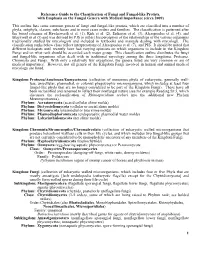
Reference Guide to the Classification of Fungi and Fungal-Like Protists, with Emphasis on the Fungal Genera with Medical Importance (Circa 2009)
Reference Guide to the Classification of Fungi and Fungal-like Protists, with Emphasis on the Fungal Genera with Medical Importance (circa 2009) This outline lists some common genera of fungi and fungal-like protists, which are classified into a number of phyla, subphyla, classes, subclasses and in most cases orders and families. The classification is patterned after the broad schemes of Hawksworth et al. (1), Kirk et al. (2), Eriksson et al. (3), Alexopoulos et al. (4), and Blackwell et al (5) and was devised by PJS to reflect his perception of the relationships of the various organisms traditionally studied by mycologists and included in textbooks and manuals dealing with mycology. The classification ranks below class reflect interpretations of Alexopoulos et al. (7), and PJS. It should be noted that different biologists until recently have had varying opinions on which organisms to include in the Kingdom Fungi and on what rank should be accorded each major group. This classification outline distributes the fungi and fungal-like organisms often dealt with in traditional mycology among the three kingdoms, Protozoa, Chromista and Fungi. With only a relatively few exceptions, the genera listed are very common or are of medical importance. However, not all genera of the Kingdom Fungi involved in human and animal medical mycology are listed. Kingdom: Protozoa/Amebozoa/Eumycetozoa (collection of numerous phyla of eukaryotic, generally wall- less, unicellular, plasmodial, or colonial phagotrophic microorganisms, which includes at least four fungal-like phyla that are no longer considered to be part of the Kingdom Fungi). These have all been reclassified and renamed to reflect their nonfungal nature (see for example Reading Sz 5, which discusses the reclassification of Rhinosporidium seeberi into the additional new Phylum Mezomycetozoea). -

A New European Species of the Opportunistic Pathogenic 2 Genus Saksenaea – S
bioRxiv preprint doi: https://doi.org/10.1101/597955; this version posted April 6, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. 1 A New European Species of The Opportunistic Pathogenic 2 Genus Saksenaea – S. dorisiae Sp. Nov. 3 Roman Labudaa,c*, Andreas Bernreiterb,c, Doris Hochenauerb, Christoph Schüllerb,c, Alena 4 Kubátovád, Joseph Straussb,c and Martin Wagnera,c a 5 Department for Farm Animals and Veterinary Public Health, Institute of Milk Hygiene, Milk Technology and 6 Food Science; Bioactive Microbial Metabolites group (BiMM), University of Veterinary Medicine Vienna, Konrad 7 Lorenz Strasse 24, 3430 Tulln a.d. Donau, Austria 8 bDepartment of Applied Genetics and Cell Biology, Fungal Genetics and Genomics Laboratory, University of 9 Natural Resources and Life Sciences, Vienna (BOKU); Konrad Lorenz Strasse 24, 3430 Tulln a.d. Donau, Austria 10 c Research Platform Bioactive Microbial Metabolites (BiMM), Konrad Lorenz Strasse 24, 3430 Tulln a.d. Donau, 11 Austria 12 d Charles University, Faculty of Science, Department of Botany, Culture Collection of Fungi (CCF), Benátská 2, 13 128 01 Prague 2, Czech Republic 14 15 *Corresponding author. Email: [email protected] 16 17 1 bioRxiv preprint doi: https://doi.org/10.1101/597955; this version posted April 6, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. 18 Abstract: A new species Saksenaea dorisiae (Mucoromycotina, Mucorales), recently isolated 19 from a water sample originating from a private well in a rural area of Serbia (Europe), is 20 described and illustrated. -

Biology, Systematics and Clinical Manifestations of Zygomycota Infections
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by IBB PAS Repository Biology, systematics and clinical manifestations of Zygomycota infections Anna Muszewska*1, Julia Pawlowska2 and Paweł Krzyściak3 1 Institute of Biochemistry and Biophysics, Polish Academy of Sciences, Pawiskiego 5a, 02-106 Warsaw, Poland; [email protected], [email protected], tel.: +48 22 659 70 72, +48 22 592 57 61, fax: +48 22 592 21 90 2 Department of Plant Systematics and Geography, University of Warsaw, Al. Ujazdowskie 4, 00-478 Warsaw, Poland 3 Department of Mycology Chair of Microbiology Jagiellonian University Medical College 18 Czysta Str, PL 31-121 Krakow, Poland * to whom correspondence should be addressed Abstract Fungi cause opportunistic, nosocomial, and community-acquired infections. Among fungal infections (mycoses) zygomycoses are exceptionally severe with mortality rate exceeding 50%. Immunocompromised hosts, transplant recipients, diabetic patients with uncontrolled keto-acidosis, high iron serum levels are at risk. Zygomycota are capable of infecting hosts immune to other filamentous fungi. The infection follows often a progressive pattern, with angioinvasion and metastases. Moreover, current antifungal therapy has often an unfavorable outcome. Zygomycota are resistant to some of the routinely used antifungals among them azoles (except posaconazole) and echinocandins. The typical treatment consists of surgical debridement of the infected tissues accompanied with amphotericin B administration. The latter has strong nephrotoxic side effects which make it not suitable for prophylaxis. Delayed administration of amphotericin and excision of mycelium containing tissues worsens survival prognoses. More than 30 species of Zygomycota are involved in human infections, among them Mucorales are the most abundant. -

Structure and Life Cycle of Rhyzopus Taxonomic Position of Rhizopus Mycota Eumycotina Zygomycetes Mucorales Mucoraceae Rhizopus
COURSE: B.Sc Botany SEMESTER: II PAPER: Mycology and Phytopathology / BOT CC 203 TOPIC: Structure and life cycle of Rhyzopus FACULTY: Dr. Urvashi Sinha Email id: [email protected] Taxonomic position of Rhizopus Mycota Eumycotina Zygomycetes Mucorales Mucoraceae Rhizopus stolinifer General characters: 1. Common fungi growing on stale bread, therefore, also called Bread mould. 2. Lives as a saprophytes 3. Grows on damp decaying fruit, vegetables, pickles etc. 4. Under certain conditions it lives as facultative parasite on strawberry fruit causing leak and soft rot disease 5. This widespread genus includes at least eight species. Structure of thallus: 1. The vegetative plant body is eucarpic and consists of white cottony, much branched mycelium. 2. The mycelial plant body is differentiated into nodes and internodes 3. The internodal region is the aerial and arching hyphae, known as stolon, which when touches the substratum forms the nodal region. 4. The nodal region bears much branched rhizoid grows downward, inside the substratum for anchorage and absorption of food. 5. The hyphal wall is microfibrillar and consists mainly of chitin-chitosan. In addition to chitin- chitosan, other substances like proteins, lipids, purines and salts like calcium and magnesium are also present in the hyphal wall. 6. Inner to the cell wall, cell membrane is present which covers the protoplast. The protoplast contains many nuclei, mitochondria, endoplasmic reticulum, ribosome, oil droplets, vacuoles and other substances. The size of the vacuole enlarges with age by coalescence of smaller vacuoles. Reproduction in Rhizopus: Rhizopus Stolonifer reproduces by vegetative, asexual and sexual mode. 1. Vegetative reproduction: It takes by fragmentation.