Emergency Medical Retrieval Service (EMRS)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
15-Coned-Ccrn-Cardiovascular.Pdf
1 Cardiovascular Introduction A. Anatomy & Physiology B. Cardiac Assessment 1. Cardiac Risk Factors Non Modifiable Age Gender Family History Race Modifiable Smoking Hypertension Diabetes Obesity Stress Exercise Hyperlipidemia 2. Medical & Surgical History 3. Social History 4. Medication History 5. Physical Exam 2 Color Pulses Rate & Rhythm PMI Location Extremity Temperature Dyspnea Fatigue Level Fluid Retention Palpitations Dizziness 6. Chest Pain Exam PQRST Assessment P: Pain, Placement, Provocation Q: Quality (sharp, stabbing, pressure) , Quantity R: Radiation, Relief S: Severity, Systems (nausea, sweaty, dizziness) T: Timing (when it started, how long did it last, what makes it better or worse) C. Diagnostic Tests & Procedures 1. 12 Lead ECG 2. Echocardiography (Transthoracic and Transesepheal) 3. Stress Test 4. Cardiac Catheterization 5. Doppler Ultrasound 6. Blood Work Acute Coronary Syndrome Cardiac Enzymes: CK-MB, Amino Acids: Troponins Heme Proteins: Myoglobin Lipid Profile Triglycerides Cholesterol Low Density Lipoproteins High Density Lipoprotein Coagulation Profile PT/INR aPTT ACT 3 Misc B Type Naturetic Peptide – BNP C Reactive Protein Homocysteine Hemodynamic Monitoring/Assessment CARDIAC OUTPUT HEART RATE X STROKE VOLUME PRELOAD + AFTERLOAD + CONTRACTILITY + The volume of blood in the The pressure or resistance the LV must contract The ability of the against or overcome to eject the blood or create ventricle at end diastole. systole. myocardium to contract. Total Blood Volume -
Keys to Successful Cardioversion
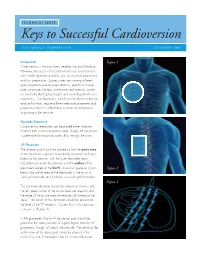
TECHNICAL NOTE: Keys to Successful Cardioversion ZOLL MEDICAL CORPORATION DECEMBER 2009 Introduction Figure 1 Cardioversion is the most direct treatment for atrial fibrillation. However, the success of a cardioversion can be enhanced with careful attention to details, such as electrode placement and skin preparation. Success rates vary among different types of patients and among institutions, and this technical note summarizes the keys to enhance cardioversion success as shared by electrophysiologists and cardiologists with vast experience. Cardioversions, which are intended to terminate atrial arrhythmias, require different electrode placement and preparation than for defibrillation to terminate arrhythmias originating in the ventricle. Electrode Placement Cardioversion electrodes can be placed either Anterior– Posterior (AP) or Anterior-Anterior (AA), though AP placement is preferable for maximum current flow through the atria. AP Placement The anterior pad should be placed so that the active area of the electrode is placed immediately adjacent and right lateral to the sternum, with the outer electrode foam circumference under the clavicle and the midline of the electrode located at the fourth intracostal space as shown Figure 2 below (the active area of the electrodes is the tin on a solid gel electrode and the foam on a wet gel electrode). Figure 3 The posterior electrode should be placed as shown, with the left upper corner of the active area sub-scapular and the edge of the active area immediately left lateral to the spine. The center of the electrode should be placed at the level of the T7 vertebra. Current flow in this position is shown in (Figure 3) . In AA placement (Figure 4) the sternal pad should be placed in the same position or slightly higher than for AP placement, though still below the clavicle. -

State of Missouri Physician Manual
STATE OF MISSOURI PHYSICIAN MANUAL Physician SECTION 1-PARTICIPANT CONDITIONS OF PARTICIPATION ........................................22 1.1 INDIVIDUALS ELIGIBLE FOR MO HEALTHNET, MANAGED CARE OR STATE FUNDED BENEFITS........................................................................................................................22 1.1.A DESCRIPTION OF ELIGIBILITY CATEGORIES.............................................................22 1.1.A(1) MO HealthNet...............................................................................................................22 1.1.A(2) MO HealthNet for Kids.................................................................................................23 1.1.A(3) Temporary MO HealthNet During Pregnancy (TEMP)................................................25 1.1.A(4) Voluntary Placement Agreement for Children .............................................................25 1.1.A(5) State Funded MO HealthNet.........................................................................................25 1.1.A(6) MO Rx...........................................................................................................................26 1.1.A(7) Women’s Health Services .............................................................................................26 1.1.A(8) ME Codes Not in Use ...................................................................................................27 1.2 MO HEALTHNET AND MO HEALTHNET MANAGED CARE ID CARD......................27 1.2.A FORMAT OF MO HEALTHNET -

AACN Essentials of Critical-Care Nursing Pocket Handbook, Second
AACN Essentials of Critical Care Nursing—Pocket Handbook Notice Medicine is an ever-changing science. As new research and clinical experience broaden our knowledge, changes in treatment and drug therapy are required. The editor and publisher of this work have checked with sources believed to be reliable in their efforts to provide information that is complete and generally in accord with the standards accepted at the time of publication. However, in view of the possibility of human error or changes in medical sciences, neither the editors nor the publisher nor any other party who has been involved in the preparation or publication of this work warrants that the information contained herein is in every respect accurate or complete, and they disclaim all responsibility for any errors or omissions or for the results obtained from use of the information contained in this work. Readers are encouraged to confirm the information contained herein with other sources. For example and in particular, readers are advised to check the product information sheet included in the package of each drug they plan to administer to be certain that the information contained in this work is accurate and that changes have not been made in the recommended dose or in the contraindications for administration. This recommendation is of particular importance in connection with new or infrequently used drugs. AACN Essentials of Critical Care Nursing Pocket Handbook Second Edition Marianne Chulay, RN, PhD, FAAN Consultant, Critical Care Nursing and Clinical Research Gainesville, Florida Suzanne M. Burns RN, MSN, RRT, ACNP, CCRN, FAAN, FCCM, FAANP Professor of Nursing, Acute and Specialty Care School of Nursing Advanced Practice Nurse Level 2, Director Professional Nursing Staff Organization Research Program University of Virginia Health System Charlottesville, Virginia New York Chicago San Francisco Lisbon London Madrid Mexico City Milan New Delhi San Juan Seoul Singapore Sydney Toronto Copyright © 2010, 2006 by The McGraw-Hill Companies, Inc. -
Mastering Pacing, Cardioversion and Defibrillation
Mastering Pacing, Cardioversion and Defibrillation Mike McEvoy, PhD, NRP, RN, CCRN Sr. Staff RN – Cardiovascular Surgical ICU Albany Medical Center NTI class code: EXED223 Pacing, Cardioversion, Defib Indications Too many to list… (Patient Must Be Symptomatic and Documented with ECG) Too slow Too fast Too irregular Unstable VT Cardiovert or Defibrillate? Cardioversion is synchronized with… R on T Leads? Pads? Do you need to place the leads? Where’s the best place for the pads? Synchronized Cardioversion Now, too slow… Pacing pads can be applied any time! Better to have them in place before you need them – easier to move the patient Transcutaneous Pacing Pads Conduct through skin Transcutaneous Set Rate Set Output TCP – Transcutaneous Pacing Pads on patient –Leads usually needed Turn on Pacing –Starts @ 0 mA, 80/min Increase mA until capture observed Confirm mechanical capture (pulse, SpO2) Capture TCP: What Mode? VOO VVI What’s the problem/solution? Loss of capture – increase mA Stimulation Threshold The minimum output needed to consistently capture the heart 100 mA 75 mA 50 mA Something’s not right here… Intrinsic Beat Paced Beat Intrinsic Beat Paced Beat Fusion Beat Pseudofusion Beat Fusion Beat Pseudofusion Beat Pause Button Drops rate to 25% programed value Won’t STOP pacing (10 ppm minimum) Really bad - vfib Rule # 1: Show Up & Shock Goal for defibrillation: Hospital: 3 minutes Community: 5 minutes Albert Einstein “The definition of insanity is doing the same thing over and over again and expecting different results.” Rule #2: Think Birthday Cake Optimal defib field = 90% myocardium What would Einstein do? energy Change pad location NTI class code: EXED223 Mike McEvoy [email protected] [email protected] www.mikemcevoy.com @mcevoymike mcevoymike. -

Technical Tips
The Journal of Emergency Medicine, Vol. 32, No. 1, pp. 105–111, 2007 Copyright © 2007 Elsevier Inc. Printed in the USA. All rights reserved 0736-4679/07 $–see front matter doi:10.1016/j.jemermed.2006.05.037 Technical Tips TEMPORARY TRANSVENOUS PACEMAKER PLACEMENT IN THE EMERGENCY DEPARTMENT Richard A. Harrigan, MD,* Theodore C. Chan, MD,† Steven Moonblatt, MD,* Gary M. Vilke, MD,† and Jacob W. Ufberg, MD* *Department of Emergency Medicine, Temple University School of Medicine, Philadelphia, Pennsylvania, and †Department of Emergency Medicine, University of California, San Diego Medical Center, San Diego, California e Abstract—Emergency Department placement of a tem- patient management in the ED—depending upon patient porary transvenous cardiac pacemaker offers potential life- stability—placement of a transvenous cardiac pacemaker saving benefits, as the device can definitively control heart (TVP) usually is performed after other less invasive rate, ensure effective myocardial contractility, and provide means of treatment (e.g., pharmacologic, treating the adequate cardiac output in select circumstances. The pro- cedure begins with establishment of central venous access, underlying cause, transcutaneous pacing) have been ex- usually by a right internal jugular or left subclavian vein plored and exhausted. approach, although the femoral vein is an acceptable alter- Although a variety of pacemaker modalities exist— native, especially in patients who are more likely to bleed transesophageal, epicardial, endocardial, transcutaneous, should vascular access become complicated. The indica- and transvenous—it is the latter two methods that have tions for the procedure, as well as the equipment needed, applicability in the ED. Transcutaneous pacing, which is are reviewed. Both blind and ECG-guided techniques of usually employed initially as a temporizing measure, will insertion are described. -

Management of Exposed Pacemaker Caused by Burns
Exposed pacemaker Romanian Journal of Anaesthesia and Intensive Care 2019 Vol 26 No 1, 79-82 CASE REPORT DOI: http://dx.doi.org/10.2478/rjaic-2019-0012 Management of exposed pacemaker caused by burns Christopher William Maxwell, Jr.1, Joshua Carson2, Michael R. Kaufmann3, Brenda G. Fahy1 1 Department of Anesthesiology, University of Florida College of Medicine, Gainesville, Florida, USA 2 Department of Surgery, University of Florida College of Medicine, Gainesville, Florida, USA 3 Department of Medicine, University of Florida College of Medicine, Gainesville, Florida, USA Abstract Annual implants of cardiovascular implantable devices (CIEDs) are increasing, thus increasing the risk of device exposure. This case presents CIED management issues following traumatic thermal injury. A 59- year-old female presented to intensive care with 42% total body surface area burn involving tissue over her pacemaker generator. Electrophysiologists interrogated and reprogrammed the pacer and observed the patient over 72 hours without pacing. Serratia bacteremia developed and cardiology recommended device removal. The pacemaker generator and leads were removed by cardiothoracic and burn surgery. Postoperatively, asystole required emergency transvenous pacing wire placement. During bacteremia treatment, cardiology planned to pace with an active-fixation screw-in lead with long-term plans to place a single right ventricular chamber leadless pacemaker because of the extensive burns. The patient developed fungemia and the family opted for comfort care. This case report discusses the management of a CIED exposed after a traumatic thermal burn, including device extraction. Keywords: burns, pacemaker, bacteremia Received: November 7, 2018 / Accepted: March 19, 2019 Rom J Anaesth Intensive Care 2019; 26: 79-82 as well as geriatric trauma, it is reasonable to expect traumatic CIED exposures to present more frequently at trauma centers. -

Definition, Precision, and Suitability of Electrocardiographic Signals of Electro
European Heart Journal Supplements (2017) 19 (Supplement D), D190–D211 The Heart of the Matter doi:10.1093/eurheartj/sux031 ANMCO/AIIC/SIT Consensus Information Document: definition, precision, and suitability of electrocardiographic signals of electrocardiographs, ergometry, Holter electrocardiogram, telemetry, and bedside monitoring systems Michele Massimo Gulizia, FACC, FESC (Coordinator)1*, Giancarlo Casolo, FACC, FESC (Coordinator)2, Guerrino Zuin, FACC (Coordinator)3, Loredana Morichelli4, Giovanni Calcagnini5, Vincenzo Ventimiglia6, Federica Censi5, Pasquale Caldarola7, Giancarmine Russo8, Lorenzo Leogrande9, and Gian Franco Gensini10 1Cardiology Department, Ospedale Garibaldi-Nesima, Azienda di Rilievo Nazionale e Alta Specializzazione “Garibaldi”, Via Palermo, 636 – 95122 Catania, Italy 2Cardiology Unit, Nuovo Ospedale Versilia, Lido di Camaiore, LU, Italy 3Cardiology Unit, Angelo Hospital, Mestre, VE, Italy 4Cardiology-Unit-UTIC, San Filippo Neri Hospital, Rome, Italy 5Technology and Health Department, Higher Healthcare Institute, Rome, Italy 6Member of the Italian Association of Clinical Engineers (AIIC), Crespiatica, LO, Italy 7Cardiology-Unit, San Paolo Hospital, Bari, Italy 8Italian Society for Telemedicine and eHealth (Digital SIT), Rome, Italy 9Italian Clinical Engineers’ Association (AIIC), Rome 10Italian Society for Telemedicine and eHealth (Digital SIT), Florence, Italy Document Revisors: Roberto Cemin, Domenico Gabrielli, Marco Sicuro. Consensus Document Approval Faculty in the Appendix *Corresponding author. Tel: þ095 7598502, Fax: þ095 7598505, Email: [email protected] VC The Author 2017. Published on behalf of the European Society of Cardiology. This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http:// creativecommons.org/licenses/by-nc/4.0/), which permits non-commercial re-use, distribution, and reproduction in any medium, provided the original work is properly cited. -

Open Heart Surgery in a Patient with Dual Chamber Pacemaker Lakshmi a Sathyanarayana
RIA Lakshmi A Sathyanarayana 10.5005/jp-journals-10049-0054 CASE REPORT Open Heart Surgery in a Patient with Dual Chamber Pacemaker Lakshmi A Sathyanarayana ABSTRACT involvement of cardiologist, electrophysiologist, device 1 With changing cohort of cardiac patients, elderly patients with manufacturer, anesthesiologist and cardiac surgeon. comorbidities like a patient with a pacemaker may be encoun- To the best of our knowledge, there are no case reports tered in clinical practice. In patients with a pacemaker undergo- or guidelines about a patient with a pacemaker coming ing noncardiac surgery, electromagnetic interference can alter for cardiac surgery, and we report the perioperative man- the function of a permanent pacemaker. Additional concerns agement of a pacemaker dependent patient undergoing during open heart surgery in a patient with a permanent pace- aortic valve replacement for severe aortic stenosis. maker are lead displacement with venous cannulation, electri- cal activity during cardioplegia and damage to the device by defibrillation. Management of a patient with a pacemaker for a CASE REPORT surgery calls for a multidisciplinary approach with involvement An elderly patient aged 71 years presented with a history of cardiologist, electrophysiologist, device manufacturer, anes- of breathlessness for three months. He had been inserted thesiologist, and cardiac surgeon. To the best of our knowledge, there are no case reports or guidelines about a patient with with a dual chamber pacemaker with rate modulation a pacemaker coming for cardiac surgery, and we report the (DDDR) eight years back for syncope due to complete heart perioperative management of a pacemaker dependent patient block. On precordial examination, there was grade V ejec- undergoing aortic valve replacement for severe aortic stenosis. -

Bradycardia Protocol
Michigan Adult Cardiac Protocols BRADYCARDIA Date: June 5, 2009 Page 1 of 4 Bradycardia This is a protocol for patients with serious symptomatic bradycardia. Serious symptomatic bradycardia may be defined as patients with heart rate less than 60 bpm and any of the following symptoms: chest pain, difficulty breathing, decreased level of consciousness, hypotension, or shock. Titrate treatments to a heart rate above 60 bpm. If the patient remains hypotensive refer to the cardiogenic shock protocol. Pre-Medical Control 1. Follow the General Pre-Hospital Care Protocol. 2. Administer Atropine 0.5 mg IV repeating every 3-5 minutes to a total dose of 3 mg IV, until a heart rate of greater than 60/minute is reached. 3. Transcutaneous pacing (TCP) when available may be initiated prior to establishment of IV access and/or before Atropine begins to take effect. Pacing is the treatment of choice for high degree A-V block. Follow the External Pacing Protocol. 4. Provide sedation as needed. Sedation : (Select Options) (Titrate to minimum amount necessary) □ Midazolam 1-5 mg IV/ IO (0.05 mg/kg) titrated slowly may repeat every 5 minutes until maximum of 0.1 mg/kg □ Diazepam 5-10 mg IV/ IO (0.1 mg/kg) titrated slowly may repeat every 5 minutes until maximum 0.3 mg/kg □ Lorazepam 1-2 mg IV/ IO (0.1 mg/kg, max 4 mg/dose) titrated may repeat every 5 minutes until maximum of 8 mg □ Fentanyl 1 mcg/kg IV/IO Post-Medical Control 1. Consider Dopamine Drip 2-10 mcg/kg/min. -

Clinical Information
Clinical Information Noninvasive Pacing Capture Some of the most frequent queries addressed 0 7 : 18 24NOV92 LEAD I I X 1 . 0 PACE RATE 100 70 MA by the clinical specialists at Physio-Control relate to noninvasive pacing. Although the therapy has become relatively commonplace over the past 20 years, it is not so common the clinicians administer it frequently. As with anything else, the more experience one has the greater the learning and the easier the job becomes. Interpretation of the externally paced ECG is not always simple. This article will illustrate typical paced ECGs and discuss pacing capture. Figure 1 All patients who are being noninvasively paced should be continually monitored by 16 : 57 19AUG91 LEAD I I X 0 . 5 PACE RATE 90 56 MA ECG, under constant direct observation, and be frequently assessed for mechanical and electrical capture. Electrical capture occurs when a pacing stimulus leads to depolarization of the ventricles. It is confirmed by ECG changes typical of ventricular complexes — a widening of the QRS complex and a tall, broad T wave, — displayed on the monitor (See Figures 1–3). The deflection of the captured complex may be positive or negative. Capture accompanying noninvasive pacing resembles Figure 2 that seen in permanent or temporary invasive pacing. LEAD I I X 1 . 0 Mechanical capture is the contraction of the myocardium and is evidenced by presence of a pulse and signs of improved cardiac output. Both electrical and mechanical capture must occur to benefit the patient. Many patients achieve capture at 50 to 90 mA, although individual thresholds vary markedly.1,2,3 Capture thresholds are not related to body surface area or weight,2,4 but recent thoracic surgery, pericardial effusion, pericardial tamponade, hypoxia, acidosis and Figure 3 other physiological variable may lead to higher capture thresholds.2 CONTINUED t Clinical Information Noninvasive Pacing Capture The most common error in noninvasive LEAD I I X 1 . -
Non-Invasive Transcutaneous Pacing Application Note
PUBLISH Non-Invasive Transcutaneous Pacing Application Note Introduction This Application Note provides an overview of non-invasive transcutaneous pacing. It includes a brief history of pacing, describes the electrical activity of the heart, and explains how pacing works. Non-Invasive Transcutaneous Pacing What is Non-Invasive Transcutaneous Pacing? Non-invasive transcutaneous pacing is a technique of cardiac depolarization and myocardial contraction. electrically stimulating the heart externally through a set Pacing is one method of treating patients when their of electrode pads. The stimulus is intended to cause heart’s own conduction system slows dangerously. Electrical Activity of the Heart The unique physiologic characteristics of cardiac muscle In order for the heart to beat with a smooth and efficient cells produce intrinsic pacing and efficient conduction, pumping action, the various parts of the myocardium leading to optimal synchrony and contractility (see must contract in a well-defined sequence. The atria must Figure 1). contract before the ventricles, the ventricles must begin 1 contracting near the apex, etc. An orderly sequence of Figure 1 The Cardiac Cycle contraction during systole is provided for by specialized conductive pathways in the myocardium. These pathways consist of highly specialized myocardial R cells which have the ability to conduct a depolarization wave at a much greater velocity than ordinary myocardial P T cells. Q The normal sequence of myocardial depolarization and S contraction, is described below: Atrial systole Ventricular systole Diastole 1. A cluster of highly conductive cells called the sino-atrial (SA) node is located near the back wall of the right atrium (see Figure 2).