What Is a Kidney Stone and What Happens If I Get One?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Protection and Transmission of Chinese Nanyin by Prof
Protection and Transmission of Chinese Nanyin by Prof. Wang, Yaohua Fujian Normal University, China Intangible cultural heritage is the memory of human historical culture, the root of human culture, the ‘energic origin’ of the spirit of human culture and the footstone for the construction of modern human civilization. Ever since China joined the Convention for the Safeguarding of the Intangible Cultural Heritage in 2004, it has done a lot not only on cognition but also on action to contribute to the protection and transmission of intangible cultural heritage. Please allow me to expatiate these on the case of Chinese nanyin(南音, southern music). I. The precious multi-values of nanyin decide the necessity of protection and transmission for Chinese nanyin. Nanyin, also known as “nanqu” (南曲), “nanyue” (南乐), “nanguan” (南管), “xianguan” (弦管), is one of the oldest music genres with strong local characteristics. As major musical genre, it prevails in the south of Fujian – both in the cities and countryside of Quanzhou, Xiamen, Zhangzhou – and is also quite popular in Taiwan, Hongkong, Macao and the countries of Southeast Asia inhabited by Chinese immigrants from South Fujian. The music of nanyin is also found in various Fujian local operas such as Liyuan Opera (梨园戏), Gaojia Opera (高甲戏), line-leading puppet show (提线木偶戏), Dacheng Opera (打城戏) and the like, forming an essential part of their vocal melodies and instrumental music. As the intangible cultural heritage, nanyin has such values as follows. I.I. Academic value and historical value Nanyin enjoys a reputation as “a living fossil of the ancient music”, as we can trace its relevance to and inheritance of Chinese ancient music in terms of their musical phenomena and features of musical form. -

Secret in the Stone
Also by Kamilla Benko The Unicorn Quest WPS: Prepress/Printer’s Proof 9781408898512_txt_print.pdf November 15, 2018 13:06:25 WPS: Prepress/Printer’s Proof 9781408898512_txt_print.pdf November 15, 2018 13:06:25 “WAR CHANT” Axes chop And hammers swing, Soldiers stomp, But diamonds gleam. Mothers weep And fathers worry, But only war Can bring me glory. Emeralds shine And rubies mourn, But there’s no mine For unicorn’s horn. Axes chop And hammers swing, My heart stops, But war cries ring. Gemmer Army Marching Chant Lyrics circa 990 Craft Era Composer unknown CHAPTER 1 Graveyard. That was the first word that came to Claire Martinson’s mind as she took in the ruined city ahead of her. The second and third words were: Absolutely not. There was no way this could be the city they’d been seeking—the Gem- mer school where Claire would learn how to perfect her magic. Where she was going to figure out how to bring unicorns back to Arden. This was . “A ghost town,” Claire whispered. “Are you sure it’s Stonehaven?” Sophie asked, and Claire was glad to hear some apprehension in her older sister’s voice. If Sophie, who at the age of thirteen had already explored a magical land by herself, defeated a mysterious illness, and passed sixth grade, wasn’t feeling great about their final desti- nation, then maybe Claire wasn’t such a coward after all. “It looks so . .” “Creepy?” Claire offered. Sophie tightened the ribbon on her ponytail. “Desolate,” she finished. Desolate, indeed. Stone houses stood abandoned, their win- dows as empty as the sockets of a skull. -
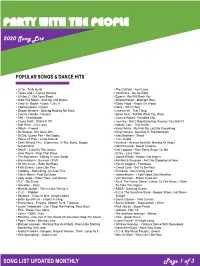
View the Full Song List
PARTY WITH THE PEOPLE 2020 Song List POPULAR SONGS & DANCE HITS ▪ Lizzo - Truth Hurts ▪ The Outfield - Your Love ▪ Tones And I - Dance Monkey ▪ Vanilla Ice - Ice Ice Baby ▪ Lil Nas X - Old Town Road ▪ Queen - We Will Rock You ▪ Walk The Moon - Shut Up And Dance ▪ Wilson Pickett - Midnight Hour ▪ Cardi B - Bodak Yellow, I Like It ▪ Eddie Floyd - Knock On Wood ▪ Chainsmokers - Closer ▪ Nelly - Hot In Here ▪ Shawn Mendes - Nothing Holding Me Back ▪ Lauryn Hill - That Thing ▪ Camila Cabello - Havana ▪ Spice Girls - Tell Me What You Want ▪ OMI - Cheerleader ▪ Guns & Roses - Paradise City ▪ Taylor Swift - Shake It Off ▪ Journey - Don’t Stop Believing, Anyway You Want It ▪ Daft Punk - Get Lucky ▪ Natalie Cole - This Will Be ▪ Pitbull - Fireball ▪ Barry White - My First My Last My Everything ▪ DJ Khaled - All I Do Is Win ▪ King Harvest - Dancing In The Moonlight ▪ Dr Dre, Queen Pen - No Diggity ▪ Isley Brothers - Shout ▪ House Of Pain - Jump Around ▪ 112 - Cupid ▪ Earth Wind & Fire - September, In The Stone, Boogie ▪ Tavares - Heaven Must Be Missing An Angel Wonderland ▪ Neil Diamond - Sweet Caroline ▪ DNCE - Cake By The Ocean ▪ Def Leppard - Pour Some Sugar On Me ▪ Liam Payne - Strip That Down ▪ O’Jay - Love Train ▪ The Romantics -Talking In Your Sleep ▪ Jackie Wilson - Higher And Higher ▪ Bryan Adams - Summer Of 69 ▪ Ashford & Simpson - Ain’t No Stopping Us Now ▪ Sir Mix-A-Lot – Baby Got Back ▪ Kenny Loggins - Footloose ▪ Faith Evans - Love Like This ▪ Cheryl Lynn - Got To Be Real ▪ Coldplay - Something Just Like This ▪ Emotions - Best Of My Love ▪ Calvin Harris - Feel So Close ▪ James Brown - I Feel Good, Sex Machine ▪ Lady Gaga - Poker Face, Just Dance ▪ Van Morrison - Brown Eyed Girl ▪ TLC - No Scrub ▪ Sly & The Family Stone - Dance To The Music, I Want ▪ Ginuwine - Pony To Take You Higher ▪ Montell Jordan - This Is How We Do It ▪ ABBA - Dancing Queen ▪ V.I.C. -

Management of Ureteral Stones
Management of Ureteral Stones Ureteral stone disease is among the most painful and prevalent of urologic disorders. As many as 5 percent of Americans will be affected by urinary stones at some point in their lives. Fortunately, most stones pass out of the body without any intervention. If you are not so lucky, the following information should help you and your doctor address the causes, symptoms and possible complications created by your ureteral stone disease. How does the urinary tract work under normal conditions? The urinary tract is similar to a plumbing system, with special pipes that allow water and salts to flow through them. The urinary tract includes two kidneys, two ureters and the urethra. The kidneys act as a filter system for the blood, cleansing it of poisonous materials and retaining valuable glucose, salts and minerals. Urine, the waste product of the filtration, is produced in the kidney and trickles down hours a day through two 10- to 12-inch long tubes called ureters, which connect the kidneys to the bladder. The ureters are about one-fourth inch in diameter and their muscular walls contract to make waves of movement to force the urine into the bladder. The bladder is expandable and stores the urine until it can be conveniently disposed of. It also closes passageways into the ureters so that urine cannot flow back into the kidneys. The tube through which the urine flows out of the body is called the urethra. What is a ureteral stone? A ureteral stone is a kidney stone that has moved down into the ureter. -

4.7 the Sword in the Stone
4.7 The Sword in the Stone (King Arthur, famous in legends and history as one of the bravest and noblest Kings of Britain, grew up as an orphaned youth, before Destiny intervened, in the form of his protector and guardian, Merlin the Magician, to reveal his true identity to the people of Britain.) In ancient Britain, at a time when the land was invaded by wild barbarians, the good and noble Lord Uther fought them bravely and drove them away from his land. The people made him king of Britain and gave him the title, Pendragon, meaning Dragon’s head. King Uther Pendragon ruled Britain wisely and well; the people were content. But very soon, the king died; it was thought that he had been poisoned by some traitors. There was no heir to the throne of British. The powerful Lords and Knights who had been kept under control by King Uther, now began to demand that one of them should be crowned King of Britain. Rivalry grew amongst the Lords, and the country as a whole began to suffer. Armed robbers roamed the countryside, pillaging farms and fields. People felt unsafe and insecure in their own homes. Fear gripped the country and lawlessness prevailed over the divided kingdom. Nearly sixteen years had passed since the death of Lord Uther. All the Lords and Knights of Britain had assembled at the Great Church of London for Christmas. On Christmas morning, just as they were leaving the Church, a strange sight drew their attention. In the churchyard was a large stone, and on it an anvil of steel, and in the steel a naked sword was held, and about it was written in letters of gold, ‘Whoso pulleth out this sword is by right of birth King of England.’ Many of the knights could not hold themselves back. -

Stone Mountain State Park
OUR CHANGING LAND Stone Mountain State Park An Environmental Education Learning Experience Designed for Grades 4-8 “The face of places, and their forms decay; And what is solid earth, that once was sea; Seas, in their turn, retreating from the shore, Make solid land, what ocean was before.” - Ovid Metamorphoses, XV “The earth is not finished, but is now being, and will forevermore be remade.” - C.R. Van Hise Renowned geologist, 1898 i Funding for the second edition of this Environmental Education Learning Experience was contributed by: N.C. Division of Land Resources, Department of Environment and Natural Resources, and the N.C. Mining Commission ii This Environmental Education Learning Experience was developed by Larry Trivette Lead Interpretation and Education Ranger Stone Mountain State Park; and Lea J. Beazley, Interpretation and Education Specialist North Carolina State Parks N.C. Division of Parks and Recreation Department of Environment and Natural Resources Michael F. Easley William G. Ross, Jr. Governor Secretary iii Other Contributors . Park volunteers; Carl Merschat, Mark Carter and Tyler Clark, N.C. Geological Survey, Division of Land Resources; Tracy Davis, N.C. Division of Land Resources; The N.C. Department of Public Instruction; The N.C. Department of Environment and Natural Resources; and the many individuals and agencies who assisted in the review of this publication. 385 copies of this public document were printed at a cost of $2,483.25 or $6.45 per copy Printed on recycled paper. 10-02 iv Table of Contents 1. Introduction • Introduction to the North Carolina State Parks System.......................................... 1.1 • Introduction to Stone Mountain State Park ........................................................... -

Flexible Ureteroscopic Laser Lithotripsy for Upper Urinary Tract Stone Disease in Patients with Spinal Cord Injury
Urolithiasis DOI 10.1007/s00240-015-0786-0 ORIGINAL PAPER Flexible ureteroscopic laser lithotripsy for upper urinary tract stone disease in patients with spinal cord injury Abdulkadir Tepeler1 · Brian C. Sninsky1 · Stephen Y. Nakada1 Received: 12 January 2015 / Accepted: 12 May 2015 © Springer-Verlag Berlin Heidelberg 2015 Abstract The objective of this study is to present the hyperuricosuria (n: 1) were common abnormalities in 24-h outcomes of flexible ureteroscopic laser lithotripsy (URS) urine analysis. Ureteroscopic laser lithotripsy can be an for upper urinary tract stone disease in spinal cord injury effective treatment modality for SCI patients with upper (SCI) patients performed by a single surgeon. A retrospec- urinary tract calculi. tive analysis was performed for SCI patients treated with flexible URS for proximal ureter and kidney stone disease Keywords Spinal cord injury · Urolithiasis · by a single surgeon between 2003 and 2013. Patient char- Ureteroscopy · Laser lithotripsy acteristics, operative outcomes, metabolic evaluation, and stone analyses were assessed in detail. A total of 27 URS procedures were performed for urolithiasis in 21 renal Introduction units of 19 patients. The mean age was 52.1 15.6 years ± (16–72) and mean BMI was 29.2 7.3 kg/m2 (20–45.7). Spinal cord injury (SCI) causes neurologic problems ± Etiology of SCI was trauma (n: 10), multiple sclerosis (n: including deterioration of sensorial, motor and autonomic 6), cerebrovascular accident (n: 1), or undetermined (n: 2). functions, leading to restricted physical activity, bladder The mean stone size was 15.9 8.6 (6–40) mm. In the and bowel dysfunction, and metabolic alterations. -

Acta SLIKE Za INTERNET.Pmd
ACTA CARSOLOGICA 32/2 13 161-174 LJUBLJANA 2003 COBISS: 1.01 LANDUSE AND LAND COVER CHANGE IN THE LUNAN STONE FOREST, CHINA UPORABA POVRŠJA IN SPREMEMBE RASTLINSKEGA POKROVA V LUNANSKEM KAMNITEM GOZDU, KITAJSKA CHUANRONG ZHANG & MICHAEL DAY & WEIDONG LI 1 Department of Geography, University of Wisconsin-Milwaukee, Milwaukee, Wisconsin 53201, USA. E-mail: [email protected] [email protected] [email protected] Prejeto / received: 4. 7. 2003 161 Acta carsologica, 32/2 (2003) Abstract UDC: 551.44:504.03(510) Chuanrong Zhang & Michael Day & Weidong Li: Landuse and Land Cover Change in the Lunan Stone Forest, China The Lunan Stone Forest is the World’s premier pinnacle karst landscape, with attendant scientific and cultural importance. Ecologically fragile, it is also a major tourist attraction, currently receiving over 1.5million visitors each year. Conservation efforts have been undermined by conflicting economic priorities, and landscape degradation threatens the very foundation of the national park. Assessment of the current land cover in the 35km2 core of the Stone Forest and an analysis of land cover change since 1974 in the 7km2 Major Stone Forest reveal the extent of recent landscape change. Exposed pinnacle karst covers 52% of the 35km2 study area, and about half of this is vegetated. Land use is dominated by agriculture, particularly in the valleys, but much of the shilin is devegetated and about six percent of the area is now built-up. Within the 7km2 Major Stone Forest the built-up area increased from 0.15ha in 1974 to 38.68ha by 2001, and during that same period road length increased by 95%, accompanied by a 3% decrease in surface water area. -

Calcium Kidney Stones Are Associated with Increased Risk Of
Journal of Clinical Medicine Article Calcium Kidney Stones are Associated with Increased Risk of Carotid Atherosclerosis: The Link between Urinary Stone Risks, Carotid Intima-Media Thickness, and Oxidative Stress Markers Ho Shiang Huang 1,2, Pao Chi Liao 3 and Chan Jung Liu 1,* 1 Department of Urology, National Cheng Kung University Hospital, College of Medicine, National Cheng Kung University, Tainan 70403, Taiwan; [email protected] 2 Department of Urology, College of Medicine, National Cheng Kung University, Tainan 70403, Taiwan 3 Department of Environmental and Occupational Health, Medical College, National Cheng Kung University, Tainan 70403, Taiwan; [email protected] * Correspondence: [email protected]; Tel.: +886-6-235-3535 (ext. 5251); Fax: +886-6-276-6179 Received: 7 February 2020; Accepted: 6 March 2020; Published: 8 March 2020 Abstract: Previous studies have suggested that kidney stone formers are associated with a higher risk of cardiovascular events. To our knowledge, there have been no previous examinations of the relationship between carotid intima-media thickness (IMT) and urinary stone risk factors. This study was aimed toward an investigation of the association between dyslipidemia, IMT, and 24-hour urinalysis in patients with calcium oxalate (CaOx) or calcium phosphate (CaP) stones. We prospectively enrolled 114 patients with kidney stones and 33 controls between January 2016 and August 2016. All patients were divided into four groups, according to the stone compositions—CaOx 50% group, CaP group, struvite group, and uric acid stones group. Carotid IMT and the carotid ≥ score (CS) were evaluated using extracranial carotid artery doppler ultrasonography. The results of a multivariate analysis indicated that a higher serum total cholesterol (TC) and low-density lipoprotein (LDL) were all associated with lower urinary citrate and higher CS in both the CaOx 50% and CaP ≥ groups. -

Repertoire Step The
Repertoire Step the Gap Valerie Amy Winehouse Think Aretha Franklin Seven Nation Army Ben L’oncle Soul Shake Your Tailfeather Blues Brothers Soul Man Blues Brothers Treasure Bruno Mars Uptown Funk Bruno Mars Good Times Chic Relight My Fire Dan Hartman Smoorverliefd Doe Maar Hot Stuff Donna Summer Long Train Running Doobie Brothers Boogie Nights Earth Wind and Fire Getaway Earth Wind and Fire I Will Survive Gloria Gaynor Proud Mary Ike & Tina Turner Blame It on the Boogie Jackson 5 I Want You Back Jackson 5 Rock With You Michael Jackson Lady Marmalade Patti LaBelle I’m So Excited Pointer Sisters, The I Wish Stevie Wonder Signed Sealed Delivered Stevie Wonder Sir Duke Stevie Wonder Soul With a Capital S Tower of Power Disco Inferno Trammps I Wanna Dance With Somebody Whitney Houston Play That Funky Music Wild Cherry Kool Brothers and Sisters Medley Stomp! Brothers Johnson Celebration Kool and the Gang Get Down On It Kool and the Gang Ladies Night Kool and the Gang Straight Ahead Kool and the Gang He’s The Greatest Dancer Sister Sledge Lost In Music Sister Sledge Getting Jiggy With It Will Smith Michael Jackson Medley Can You Feel It Jackson 5 Shake Your Body Jackson 5 Billie Jean Michael Jackson Black or White Michael Jackson Don’t Stop ‘Til You Get Enough Michael Jackson Love Never Felt So Good Michael Jackson Thriller Michael Jackson Wanna Be Startin’ Somethin’ Michael Jackson Workin’ Day and Night Michael Jackson Short Disco Medley Candi Station Young Hearts, Run Free Cheryl Lynn Got To Be Real Diana Ross I’m Coming Out George Benson Gimme the Night Luther Vandross Never Too Much McFadden, Whitehead Ain’t No Stopping Us Now Foute Medley Ring My Bell Anita Ward Yes Sir, I Can Boogie Baccara Rasputin Boney M. -

UNJ Dec 2005-427.Ps 11/29/05 3:43 PM Page 427
UNJ Dec 2005-427.ps 11/29/05 3:43 PM Page 427 C Urolithiasis/Nephrolithiasis: O N What’s It All About? T I Joan Colella Bernadette Galli N Eileen Kochis Ravi Munver U I N G he term nephrolithiasis Urolithiasis (urinary tract calculi or stones) and nephrolithiasis (kid- (kidney calculi or stones) ney calculi or stones) are well-documented common occurrences in refers to the entire clini- the general population of the United States. The etiology of this disor- E cal picture of the forma- der is mutifactorial and is strongly related to dietary lifestyle habits or D Ttion and passage of crystal agglom- practices. Proper management of calculi that occur along the urinary U erates called calculi or stones in tract includes investigation into causative factors in an effort to pre- the urinary tract (Wolf, 2004). vent recurrences. Urinary calculi or stones are the most common C Urolithiasis (urinary calculi or cause of acute ureteral obstruction. Approximately 1 in 1,000 adults in A stones) refers to calcifications that the United States are hospitalized annually for treatment of urinary T form in the urinary system, pri- tract stones, resulting in medical costs of approximately $2 billion per marily in the kidney (nephrolithi- I year (Ramello, Vitale, & Marangella, 2000; Tanagho & McAninch, 2004). asis) or ureter (ureterolithiasis), O and may also form in or migrate N into the lower urinary system (bladder or urethra) (Bernier, 2005). Urinary tract stone disease the rest of the world. Researchers Kidney stones are most has been documented historically attribute the incidence of prevalent between the ages of 20 as far back as the Egyptian mum- nephrolithiasis in the United to 40, and a substantial number mies (Wolf, 2004). -

Historic Stone Highway Culverts in New Hampshire Asset Management Manual
Historic Stone Highway Culverts in New Hampshire Asset Management Manual Prepared for: New Hampshire Department of Transportation, Bureau of Environment, Concord. Prepared by: Historic Documentation Company, Inc., Portsmouth, RI September 2009 TABLE OF CONTENTS 1.0 INTRODUCTION .........................................................................................................1 1.1 Purpose......................................................................................................................1 1.2 Why Preserve Historic Stone Culverts .....................................................................2 2.0 IDENTIFYING HISTORIC STONE CULVERTS.......................................................4 2.1 General Information .................................................................................................4 2.2 New Hampshire Stone Culverts................................................................................7 2.3 Stone Box Culverts ...................................................................................................8 2.4 Stone Arch Culverts................................................................................................14 3.0 MAINTAINING HISTORIC STONE CULVERTS ..................................................16 3.1 General Maintenance Discussion ...........................................................................16 3.2 Inspection & Maintenance Program ......................................................................17 3.3 Clear Waterway .....................................................................................................18