Saharsa District Health Action Plan 2010-2011
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Chapter-4 Taxes on Vehicles
Chapter-3: Revenue and Land Reforms Chapter-4 Taxes on Vehicles k Audit Report (Revenue Sector) for the year ended 31 March 2017 l CHAPTER 4: TAXES ON VEHICLES 4.1 Tax administration The Transport Department levies and collects taxes on vehicles in the State, in terms of the Motor Vehicles (MV) Act, 1988, Central Motor Vehicles (CMV) Rules, 1989, Bihar Motor Vehicle Taxation (BMVT) Act, 1994 and BMVT Rules, 1994. The Department is headed by the Principal Secretary, Transport Department at the Government level and by the State Transport Commissioner (STC) at the apex level of the Department. The STC is assisted by two Joint State Transport Commissioners at the headquarters. The State is divided into nine Regional Transport Authorities1 (RTAs) and 38 District Transport Offices. They are assisted by Motor Vehicle Inspectors (MVIs). The main function of the RTAs is to issue road permits to the vehicles and the responsibility of registration of motor vehicles, levy and collection of fees and taxes and grant of driving licences are assigned to the District Transport Officers (DTOs) in the State. 4.2 Results of audit During 2016-17, the Accountant General test checked records of 342 out of 49 units of the Transport Department. Revenue collected by the Department during 2015-16 was ` 1,181.22 crore of which, the audited units collected ` 888.87 crore. Audit scrutiny revealed non/short levy of taxes, leviable taxes not realised from transport vehicles, and other irregularities involving ` 147.10 crore in 362 cases as shown in Table - 4.1. Table - 4.1 (` in crore) Sl. -
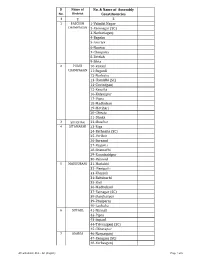
AC with District Dist
Sl Name of No. & Name of Assembly No. District Constituencies 1 2 3 1 PASCHIM 1-Valmiki Nagar CHAMPARAN 2-Ramnagar (SC) 3-Narkatiaganj 4-Bagaha 5-Lauriya 6-Nautan 7-Chanpatia 8-Bettiah 9-Sikta 2 PURVI 10-Raxaul CHAMPARAN 11-Sugauli 12-Narkatia 13-Harsidhi (SC) 14-Govindganj 15-Kesaria 16-Kalyanpur 17-Pipra 18-Madhuban 19-Motihari 20-Chiraia 21-Dhaka 3 SHEOHAR 22-Sheohar 4 SITAMARHI 23-Riga 24-Bathnaha (SC) 25-Parihar 26-Sursand 27-Bajpatti 28-Sitamarhi 29-Runnisaidpur 30-Belsand 5 MADHUBANI 31-Harlakhi 32- Benipatti 33-Khajauli 34-Babubarhi 35-Bisfi 36-Madhubani 37-Rajnagar (SC) 38-Jhanjharpur 39-Phulparas 40-Laukaha 6 SUPAUL 41-Nirmali 42-Pipra 43-Supaul 44-Triveniganj (SC) 45-Chhatapur 7 ARARIA 46-Narpatganj 47-Raniganj (SC) 48-Forbesganj AC with district Dist. - AC (English) Page 1 of 6 Sl Name of No. & Name of Assembly No. District Constituencies 1 2 3 49-Araria 50-Jokihat 51-Sikti 8 KISHANGANJ 52-Bahadurganj 53-Thakurganj 54-Kishanganj 55-Kochadhaman 9 PURNIA 56-Amour 57-Baisi 58-Kasba 59-Banmankhi (SC) 60-Rupauli 61-Dhamdaha 62-Purnia 10 KATIHAR 63-Katihar 64-Kadwa 65-Balrampur 66-Pranpur 67-Manihari (ST) 68-Barari 69-Korha (SC) 11 MADHEPURA 70-Alamnagar 71-Bihariganj 72-Singheshwar (SC) 73-Madhepura 12 SAHARSA 74-Sonbarsha (SC) 75-Saharsa 76-Simri Bakhtiarpur 77-Mahishi 13 DARBHANGA 78-Kusheshwar Asthan (SC) 79-Gaura Bauram 80-Benipur 81-Alinagar 82-Darbhanga Rural 83-Darbhanga 84-Hayaghat 85-Bahadurpur 86-Keoti 87-Jale 14 MUZAFFARPUR 88-Gaighat 89-Aurai 90-Minapur 91-Bochaha (SC) 92-Sakra (SC) 93-Kurhani 94-Muzaffarpur 95-Kanti 96-Baruraj AC with district Dist. -

Katihar Saharsa Barauni Raxaul Darbhanga Muzaffarpur Chhapra
22A Muzaffar- Saharsa Muzaffar- Chhapra Raxaul Raxaul Yesvant- Sitamarhi Katihar Muzaffarpur/ Dar- Howrah Jaynagar Raxaul Dar- Muzaf- Raxaul Kanpur Chhapra Chhapra pur Adarsh pur Lok- Delhi Sadh- Delhi pur Anand Amritsar Gorakhpur bhanga Kath- Amritsar Delhi bhanga farpur Lok- Kath- Gorakh Delhi Anand Nagar Porbandar manya bhavana Sadh- Muzaf- vihar (T) Express Bandra(T) Ahmeda- godam Saryu Satya- New Ambala manya godam pur Express Vihar (T) Delhi Express Tilak (T) Express bhavana- farpur Lichchavi Avadh bad Bagh Yamuna graha Delhi Cantt. Tilak (T) Garib Intercity TRAIN NAME Garib Poora- Godaan Express Express Express Express Sabar- Express Express Express Bihar Harihar Jan Rath Express Rath biya Express mati Sampark Express Sadharan Express Express Express Express Kranti Express Express 14007#/ 19040/ Train Number 12211 15279 19270 11060 14015$ 14017# 15227 14005 15707 19038 19166 13019 14649 15273 12565 14523 15267 12209 15105 15115* 3A 3A 1A,2A3A 2A,3A 3A 3A 2A,3A 2A,3A 2A,3A 2A,3A 2A 2A,3A 2A,3A 3A 1A,2A,3A 3A 3A 2A,3A 2A,3A Class of accommodation SL,II SL,II SL,II SL,II SL,II SL,II,P SL,II,P SL,II SL,II,P SL,II SL,II SL,II SL,II SL,II,P SL,II II SL,II SL,II via via From Table No. 29A via 63 37A 64A 64 64A 64A via 63 64 24A Days of departure at M,Th, Th,Sa/ Tu,Th,Su/ M,W, Except originating station F Th,Su Su,M Sa M,W F W Daily Daily M,W,F,Sa Sa Daily Tu,F,S u Daily Daily M,Th Sa Tu Su Sa a 22.00 Km. -

Flood Disaster and Its Impact on the People in Kosi Region, Bihar
© 2019 IJRAR May 2019, Volume 6, Issue 2 www.ijrar.org (E-ISSN 2348-1269, P- ISSN 2349-5138) FLOOD DISASTER AND ITS IMPACT ON THE PEOPLE IN KOSI REGION, BIHAR Dr. Sanjiv Kumar Research Fellow Univ. Deptt. of Geography, T.M.B.U., Bhagalpur Introduction The Kosi, a trans-boundary river between Nepal and India is often referred to as the “Sorrow of Bihar”. The flow of the river contains excessive silt and sand, resulting in changing the courses of the river. During the past, the river has kept on changing its courses between Purnea district in the east and Darbhanga and Madhubani districts in the west. The recent disaster was created by the breach in the eastern Kosi embankment upstream of the Indian border at Kursela in the neighbouring Nepal on the 18th of August 2008. A tragedy of unparalleled dimension unleashed was over three million people living in 995 villages spreading in seven districts of Kosi region, viz. Supaul, Araria, Madhepura, Saharsa, Purnia, Khagaria and Katihar. Objectives: The purpose of the paper is to investigate the damage caused by the devastating floods due to the turbulent river Kosi recurrently and its impact on the socio-economic life of the people inhabiting in the region which is densely populated but with poor economy. The objective refers to the sustainability of an agricultural region to the occurrence of a natural disaster. The objective is to achieve in order to create a sustainable system in environmental, social and economic terms. The other objective aims to preserve or improve characteristics of the environment such as biodiversity, soil, and water and air quality. -

Patna University, Ashok Rajpath, Patna-800005 Mode of Likely Date Name of the Ph.D
Name and Address of the University : Patna University, Ashok Rajpath, Patna-800005 Mode of Likely Date Name of the Ph.D. Availing Funding Name of the Ph.D.(Full Registration Date of of Sl. No. Faculty Department Scholar with Unique Research Topic Fellowship Agency of Supervisor Time/Part Number Registration completion ID/Photo ID Yes/No Fellowship Time of Ph.D. ऩटनाका नगयीकयण एवॊ Dr. Surendra Acad/557 Social व्माऩारयक औय साॊस्कृ तिक कᴂ द्र January, 1 History Kumar, Associate Anita Kumari Full Time dt.09-06- February, 2016 No Sciences 2020 Professor 2016 के रूऩ भᴂ उत्कष ष - एक अवरोकन (16 व ॊ से 18 व ॊ सदी) ईस्टइॊडडमा कॊ ऩन के सभम बायि Dr. P.N Das, Acad/557 Social भᴂ देश शशऺा व्मवस्था: एक January, 2 History Associate Sanjiv Kumar Full Time dt.09-06- February, 2016 No Sciences 2020 Professor 2016 आरोचनात्भक अध्ममन (सन ् 1600 - 1757 ई. िक) बफहायके भहहराओॊ के उत्थान भᴂ Dr. Ranjan Sinha, Acad/557 Social January, 3 History Associate Niraj Kumar Jaiswal Full Time dt.09-06- February, 2016 खादी आॊदोरन की बूशभका No Sciences 2020 Professor 2016 (1920-1947): एक अध्ममन नक्सरवादीआॊदोरन भᴂ बफहाय के Acad/557 Social Dr. Ran Vijoy January, 4 History Ravi Shankar Kumar Full Time dt.09-06- February, 2016 भध्मभवग ष की बूशभका: बफहाय के No Sciences Kumar, Professor 2020 2016 ववशॊष सॊदब ष भᴂ Acad/557 Social Dr. Ran Vijoy बायिभᴂ भहहरा सॊगठनⴂ का उद्भव January, 5 History Shobha Verti Kumari Full Time dt.09-06- February, 2016 No Sciences Kumar, Professor 2020 2016 एवॊ ववकास - 1917 - 1947 ई. -

Final Report- Community Participation of Embankment Surveillance
Volume-I FINAL REPORT Submitted to: Joint Director, Flood Management Improvement Support Centre Water Resources Department 2nd Floor, Jal Sansadhan Bhawan Anisabad, Patna-800002 Tel.: 91612-2256999, 91612-2254802 JPS Associates (P) Ltd. New Delhi Acknowledgement We at JPS take opportunity to thank all the officials at WRD namely Mr. Er Indu Bhusan Kumar, Chief Engineer (Planning and Monitoring) Mr. Narendra Prasad Mandal, Additional Project Director (BAPEPS), Official in BAPEPS namely Mr. Ravi Kumar Gupta, State Project Specialist (Environment), Officials at FMISC Mr. A.K.Samaiyar (Ex-Joint Director), Mr. Sitaram Agarwal (Ex-Joint Director), Er. Anil Kumar (Deputy Director I), Mr. Dilip Kumar Singh (Ex-Deputy Director), Mr. Nagan Prasad (Joint Director), Mr. Zakauallah (Asst.Director), Mr. Mukesh Mathur (GIS Expert) and Mr. Syed Niyaz Khurram (Web Master) for their able guidance and constant support to us in the conduct of the assignment in a smooth manner. We are also thankful to WRD field officials Mr. Prakash Das (Chief Engineer), Birpur Division, Mr. Vijender Kumar (Chief Engineer) Samastipur Division, Mr. Vijender Kumar (Executive Er. Birpur Division), Mr. Vinod Kumar (Executive Er. Nirmali Division) and Mr. Mithilesh Kumar (Executive Er.) Jhanjharpur Division and all the Asst. Engineers and the Junior Divisions of all the 11 Field Divisions for their constant support and hospitality to our team of experts and field staff during the conduct of assignment at the field level. Our thanks are also due to SRC members, Mr. Sachidanand Tiwari (Embankment Expert), and Mr. Santosh Kumar (Hydrologist), Mr. Bimalendu Kumar .Sinha, Flood Management Advisor (FMISC) and Mr. S.K. -

Saharsa, Bihar DISTRICT DEMOGRAPHIC PROFILE1 Total Population 1,900,661
DISTRICT NUTRITION PROFILE Saharsa, Bihar DISTRICT DEMOGRAPHIC PROFILE1 Total Population 1,900,661 52.5% 47.5% MALE FEMALE 8.2% 91.8% URBAN RURAL Saharsa ranks 582nd amongst 599 16.7% 0.3% 83.0% 2 SC ST OTHERS districts in India DISTRICT DEVELOPMENT INDEX (2015) THE STATE OF NUTRITION IN SAHARSA3,4,5 43,9% CHILDREN 68.4 STUNTED 63.5 48.3 43.9 44.4 43.9 24,0% 34.6 30.4 CHILDREN 24.0 WASTED 20.8 11.6 9.5 44,4% 0 0.6 Children stunted Children wasted Children Children with any Women Children with Adults who are CHILDREN (<5 yr) (%) (<5 yr) (%) underweight anemia underweight (BMI birthweight obese in the UNDERWEIGHT NFHS 4 (2015-2016) NFHS 4 (2015-2016) (<5 yr) (%) (0-59 mo) (%) <18.5) <2500gms district NFHS 4 (2015-2016) NFHS 4 (2015-2016) (15-49 yr) (%) (0-2 mo) (%) (18-59 yr) (%) NFHS 4 (2015-2016) CHHNS 7 (2015) CAB (2014) Saharsa Bihar CHANGES OVER TIME IN ANEMIA3,5,6,7 97.6 78.0 80.7 63.5 PREVALENCE OF 99.9 ANEMIA AMONGST 68.4 CHILDREN UNDER-SIX No Data 74.8 DECREASED IN THE DISTRICT BETWEEN !2002 AND 2016 DLHS 2 (2002-2004)^ NFHS 3 (2005-2006)^^ CAB (2014)^^ NFHS 4 (2015-2016)^^ ^Children aged 0-71 months Saharsa Bihar ^^Children aged 0-59 months Page 1 13 HOW CAN NUTRITION IMPROVE? WHAT FACTORS CAUSE UNDERNUTRITION? The most crucial period for child nutrition is Optimum fetal and child nutrition and development from pre-pregnancy to the second year of life2 IMMEDIATE CAUSES 100 Breastfeeding, nutrient rich foods, and eating routine 90 Feeding and caregiving practices, parenting stimulation 80 Low burden of infectious diseases 70 60 -

Disaster in Bihar: a Report from the TISS Assessment Team
Disaster in Bihar: A Report from the TISS Assessment Team Report prepared by Dr. Manish K. Jha & Mr. Vijay Raghavan TISS Assessment Team (Dr. Manish K. Jha, Mr. Vijay Raghavan, Mr. Mahesh Kamble, Mr. Dheeraj) Tata Institute of Social Sciences Mumbai September, 2008 Acknowledgements Government of Bihar Shri R.Jaya Mohan Pillai, Chief Secretary, Government of Bihar (GoB) Shri Vijay Raghavan, Development Commissioner, GoB Shri Afzal Amanullah, Principal Secretary to Government, Deptt. Of Home, GoB Shri Pratyay Amrit, Addl. Secretary, Department of Disaster Management, GoB Shri Mishra, Sub Divisional Magistrate, Saharsa Shri Chandrama Singh, District Development Commissioner Delhi School of Social Work, University of Delhi Dr. Manoj K. Jha, Associate Professor Shri Kaivalya Desai Shri Shantonu Hazarika Shri Digvijay Phukan Shri Uday Bhaskar Shri Rajeev Jena, Mr. Pushpam Civil Society Shri Vinay Odhar, Actionaid, Patna Shri Rakesh, Nidaan, Patna Shri Rajan Khosla and Shri Ram Kishan, Christian Aid Individuals Shri Sriraman, President, Dagar Bigar (an NGO) & Visiting Faculty, Patna’s Women’s College Shri Ajay K. Singh, LPG Distributer and Proprieter and local media person Ms. Nisha Bharti, TISS intern with Nidan (an NGO) Prof. Jawahar Jha and Prof. Madhuri Jha Shri Sanjay Jha Shri Chandan TISS Prof. S. Parasuraman, Director Prof. Janki Andharia, Chairperson, Jamshetji Tata Centre for Disaster Management Prof. Surinder Jaswal, School of Social Work Secretariat, School of Social Work Maintenance, and Finance and Accounts Section 2 Introduction This report is prepared on the basis of a 5-day visit to the flood affected parts of Bihar, caused by the changing of the course of the river, Kosi, by a four-member team from the Tata Institute of Social Sciences. -

Provisional Population Totals, Series-11, Bihar
CENSUS OF INDIA 2001 SERIES- 11 BIHAR PAPER 1 OF 2001 PROVISIONAL POPULATION TOTALS SUDHIR KUMAR RAKESH Director of Census Operations, Bihar Lord Buddha Dedicated to the people of Bihar and enumerators - the data producers. For the benefit of policy makers and research workers - the data consumers. CONTENTS SL. NO. PARTICULARS PAGE NO. 1. Foreword v 2 List of Officers! Officials involved in preparation of Provisional Population Totals vii 3 Figures at a Glance ix 4 State Highlights x 5 Map showing Administrative Division of India Highlighting State xi 6 Map showing Administrative Division of State, 2001 Census xiii 7 Introduction 1 8 Analysis of Results 7· 9 Provisional Population Tables 25 10 Maps 31 11 Diagrams and Charts 39 12 Organisational Chart of Census Hierarchy 49 13 Specimen Copy of Houselist Schedule 51 - 14 Specimen Copy of Household Schedule 53 15 Pictorial 55 FOREWORD After the successful completion of Census of India 2001, it gives me great pleasure to present these provisional population totals for the state of Bihar. This paper gives some basic characteristics of the population of Bihar as on 1st March, 2001 (00.00 hrs.) as recorded during the population enumeration related with the Census of India 2001. These figures are only provisional ones, compiled on the basis of the abstracts of population data prepared by the enumerators. These provisional population figures are being published with the intention of meeting the immediate need of the Government, various organisations, researchers and the general public. It would help provide them the basic population figures as quickly as possible after the population enumeration work has been completed. -
Saharsa Introduction
DISTRICT PROFILE SAHARSA INTRODUCTION Saharsa is one of the thirty-eight districts of Bihar. Saharsa district became a separate district in 1954 prior to which it was a part of Kosi division. The important rivers flowing through the district are Kosi, Baghmati. HISTORICAL BACKGROUND Earlier Saharsa district was within the Bhagalpur Division. Kosi Division was formed on 2nd October 1972 comprising of Saharsa, Purnia and Katihar district with its head quarters at Saharsa. Formerly it had no independent status and parts of Saharsa were included in the old districts of Munger & Bhagalpur. Ancient Times: In ancient times, Vaishali was the strongest republic in North-Bihar and beyond that lay the famous territory of Anguttarap. There was a small Janpad, named Apna, in Anguttarap and it included a portion of the district of Saharsa. Various sites of the district, now completely eroded and destroyed by the Kosi, viz. Biratpur, Budhiagarhi, Budhnaghat, Buddhadi, Pitahahi and Mathai are associated with Buddhism Both Anga and North Bihar (including Saharsa) continued to be independent till the early part of the sixth century B.C Between 320 and 1097 A.D Under the Guptas (from 320 A.D.), the entire North Bihar was consolidated as a Tirbhukti (province) with its capital at Vaishali. The extent of Saharsa during the period under review was upto the confines of Pundravardhanbhukti which included some of its present area. From the geographical point of view, Saharsa was the most strategically suited from being the Jayaskandharar (temporary Capital) of the Palas at the time when they were surrounded on all sides by enemies. -

Ground Water Information Booklet Darbhanga District, Bihar State
भूजल सूचना पुस्तिका दरभंगा स्जला, बिहार Ground Water Information Booklet Darbhanga District, Bihar State 85°-45' 86°-0' 86°-15' ADMINISTRATIVE MAP BIHAR STATE DARBHANGA DISTRICT, BIHAR. 0 5 10 15 Km Ganga R. Jale Scale Keotiranway 26° 26° 15' 15' Manigachi Singwara DARBHANGA Bahadurpur Alinagar Benipur Hayaghat Ghanshyampur 26° 26° 0' 0' Baheri Goura bouram Kiratpur Biraul LEGEND District Boundary Block Boundary Road Kusheshwar Kusheshwar Railway Asthan Asthan (E) District Headquarter 25° Block Headquarter 25° 45' River 45' 85°-45' 86°-0' 86°-15' के न्द्रीय भमू िजल िो셍 ड Central Ground water Board Ministry of Water Resources जल संसाधन िंत्रालय (Govt. of India) (भारि सरकार) Mid-Eastern Region िध्य-पर्वू ी क्षेत्र Patna पटना मसिंिर 2013 September 2013 1 PREPARED BY - Shri S. Sahu Sc. B UNDER SUPERVISION OF - Shri A.K.Agrawal, Scientist’D’ CARTOGRAPHY - Shri Lokendra Kumar, Draughtsman UPDATED BY - Shri S.N.Dwivedi, Sc-C & Dr. Fakhre Alam, STA (Hg) 2 CONTENTS DISTRICT AT A GLANCE 5 – 6 1. INTRODUCTION 7 - 11 1.1 Location, Area and Population 1.2 Basin/Sub-Basin and Drainage 1.3 Land use, agriculture and irrigation practices 1.4 Studies/Activities carried by CGWB 2. CLIMATE AND RAINFALL 11 - 12 3. GEOMORPHOLOGY AND SOIL 12 - 13 3.1 Geomorphology 3.2 Soil 4. HYDROGEOLOGY 13 - 17 4.1 Water Bearing Formations 4.2 Mode of Occurrence of Ground Water 4.3 Hydraulic Characteristics of Aquifers 4.4 Depth to water level 4.5 Ground Water Quality 5. GROUND WATER RESOURCES 17 - 18 5.1 Status of groundwater development 6. -

Dynamics of a River System– the Case of the Kosi River in North Bihar
e-Journal Earth Science India Vol.2 (I), January, 2009, pp. 33- 45 http://www.earthscienceindia.info/; ISSN: 0974 - 8350 Dynamics of a River System– the Case of the Kosi River in North Bihar Rajiv Sinha Engineering Geosciences Group, Department of Civil Engineering Indian Institute of Technology, Kanpur Email: [email protected] Abstract The paper presents an account of the Kusaha breach of the Kosi river which has been widely perceived as a flood event in the media and scientific circles. It is true that a large area was inundated after this event but it is important to appreciate that this inundation was different from a regular flooding event. It is argued that this event marked a mega-avulsion of the Kosi river. While the basic mechanism of this avulsion needs a detailed study, this paper aims to document the avulsion event and speculates the causative factors of the dynamics of the Kosi in general based on limited field evidence and available maps. Introduction The Year 2008 witnessed one of the greatest fluvial disasters in recent history when the Kosi river draining the parts of north Bihar shifted by ~120 kilometers eastward triggered by the breach of the eastern afflux bund at Kusaha in Nepal. The Kosi river in north Bihar plains, eastern India is a major tributary to the Ganga river system (see Fig. 1 for major morphological and hydrological characteristics; Sinha and Friend, 1994) and has long been considered as a dynamic river due to frequent changes in its course and extensive flooding (Sinha and Jain, 1998; Sinha, 1998).