Formoterol and Salbutamolinhibit Bradykinin- and Histamine-Induced
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

1 Effect of Indacaterol, a Novel Long-Acting Beta 2
ERJ Express. Published on November 29, 2006 as doi: 10.1183/09031936.00032806 EFFECT OF INDACATEROL, A NOVEL LONG-ACTING BETA 2-AGONIST, ON HUMAN ISOLATED BRONCHI Emmanuel Naline (1), Alexandre Trifilieff (2), Robin A. Fairhurst (2), Charles Advenier (1), Mathieu Molimard (3) (1) Research Unit EA220, Université de Versailles, Faculté de Médecine, Pharmacology, Hôpital Foch, 40 rue Worth, 92150 Suresnes, France (2) Novartis Institute for BioMedical Research, Horsham, England (3) Département de Pharmacologie, Université Victor Segalen Bordeaux 2; CHU Pellegrin; INSERM U657, Bordeaux, France Correspondence: Mathieu Molimard Département de Pharmacologie CHU de Bordeaux - Université Victor Segalen-INSERM U657 33076 Bordeaux cedex, France Phone: 33 (0)5 57 57 15 60 Fax: 33 (0)5 57 57 46 71 E-mail: [email protected] Short title: Indacaterol effect on isolated human bronchi 1 Copyright 2006 by the European Respiratory Society. Abstract Indacaterol is a novel β2-adrenoceptor agonist in development for the once-daily treatment of asthma and COPD. This study evaluated the relaxant effect of indacaterol on isolated human bronchi obtained from lungs of patients undergoing surgery for lung carcinoma. Potency (-logEC50), intrinsic efficacy (Emax) and onset of action were determined at resting tone. Duration of action was determined against cholinergic neural contraction induced by electrical field stimulation (EFS). At resting tone, -logEC50 and Emax values were, respectively, 8.82±0.41 and 77±5% for indacaterol, 9.84±0.22 and 94±1% for formoterol, 8.36±0.16 and 74±4% for salmeterol, and 8.43±0.22 and 84±4% for salbutamol. In contrast to salmeterol, indacaterol did not antagonize the isoprenaline response. -

Trimbow, INN-Beclometasone / Formoterol / Glycopyrronium Bromide
23 May 2017 EMA/CHMP/290028/2017 – Rev 1 Committee for Medicinal Products for Human Use (CHMP) Summary of opinion1 (initial authorisation) Trimbow beclometasone / formoterol / glycopyrronium bromide On 18 May 2017, the Committee for Medicinal Products for Human Use (CHMP) adopted a positive opinion, recommending the granting of a marketing authorisation for the medicinal product Trimbow, intended for the maintenance treatment of moderate to severe chronic obstructive pulmonary disease (COPD). The applicant for this medicinal product is Chiesi Farmaceutici S.p.A., Italy. Trimbow is a triple combination of an inhaled glucocorticoid (beclometasone dipropionate), a long-acting beta2 receptor agonist (formoterol fumarate dihydrate) and a long-acting muscarinic antagonist (glycopyrronium bromide). It will be available as a pressurised metered dose inhaler delivering a solution with a nominal dose per actuation of 87 micrograms / 5 micrograms / 9 micrograms of the active substances respectively. Beclometasone reduces inflammation in the lungs, whereas formoterol and glycopyrronium produce relaxation of bronchial smooth muscle helping to dilate the airways and make breathing easier (ATC code: R03AL09). The benefits with Trimbow are its ability to relieve and prevent symptoms such as shortness of breath, wheezing and cough and to reduce exacerbations of COPD symptoms. The most common side effects of Trimbow are oral candidiasis, muscle spasm and dry mouth. The full indication is: “Maintenance treatment in adult patients with moderate to severe -

22518Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 22518Orig1s000 CLINICAL PHARMACOLOGY AND BIOPHARMACEUTICS REVIEW(S) 7 CLINICAL PHARMACOLOGY REVIEW NDA: 22-518 Brand Name: Dulera Generic Name: Mometosone furoate / formoterol fumarate Indication: Asthma (b) (4) in adults and children 12 years of age and older Dosage Form: Inhalation aerosol Strengths: (b) (4) 100/5, 200/5 mcg Route of Administration: Oral Inhalation Dosing regimen: Two inhalations twice daily (morning and evening) Applicant: Schering-Plough and Novartis OCP Division: DCP2 Clinical Division: DPAP (OND-570) Submission Date: May 21, 2009 Reviewers: Ying Fan, Ph.D., Liang Zhao, Ph.D. Team Leader (Acting): Partha Roy, Ph. D. TABLE OF CONTENTS 1 EXECUTIVE SUMMARY.................................................................................................... 3 1.1 Recommendations ........................................................................................................................3 1.2 Phase IV commitments.................................................................................................................3 1.3 Summary of Clinical Pharmacology and Biopharmaceutics findings.....................................3 2 QUESTION BASED REVIEW............................................................................................. 9 2.1 General Attributes/Background..................................................................................................9 2.1.1 What is the pertinent regulatory background of DULERA? ..................................... -

Leukotriene D4induced Caco2 Cell Proliferation Is Mediated By
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Diposit Digital de la Universitat de Barcelona Physiological Reports ISSN 2051-817X ORIGINAL RESEARCH Leukotriene D4-induced Caco-2 cell proliferation is mediated by prostaglandin E2 synthesis Marisol Cabral, Raquel Martın-Venegas & Juan J. Moreno Departament de Fisiologia, Facultat de Farmacia, Universitat de Barcelona, Barcelona, Spain Keywords Abstract 5-lipoxygenase, arachidonic acid cascade, cell cycle, cell growth, colon cancer. Leukotriene D4 (LTD4) is a pro-inflammatory mediator formed from arachi- donic acid through the action of 5-lipoxygenase (5-LOX). Its biological effects Correspondence are mediated by at least two G-coupled plasmatic cysteinyl LT receptors (Cys- Juan Jose Moreno, Departament de LT1-2R). It has been reported an upregulation of the 5-LOX pathway in tumor Fisiologia, Facultat de Farmacia, Universitat tissue unlike in normal colon mucosa. Colon tumors generally have an de Barcelona, Avda. Joan XXIII s/n, 08028 increased expression of CysLT1R and colon cancer patients with high expres- Barcelona, Spain. sion levels of CysLT R have poor prognosis. We previously observed that the Tel: +34 93 402 4505 1 Fax: +34 93 403 5901 cyclooxygenase pathway is involved in the control of intestinal epithelial can- E-mail: [email protected] cer cell growth through PGE2 production. The aim of this study was therefore to assess the effect of LTD4 binding with CysLT1R on Caco-2 cell growth. We Funding Information note a number of key findings from this research. We observed that at a con- This research was supported by Spanish centration similar to that found under inflammatory conditions, LTD4 was Ministry of Science and Innovation (BFU2007- able to induce Caco-2 cell proliferation and DNA synthesis. -

Beclometasone / Formoterol / Glycopyrronium Bromide Pressurised Metered Dose Inhaler (Trimbow®) for the Treatment of COPD
Beclometasone / formoterol / glycopyrronium bromide pressurised metered dose inhaler (Trimbow®) for the treatment of COPD Commissioning Statement Fylde and Wyre Clinical Commissioning Group has agreed to fund the prescribing of Beclometasone / formoterol / glycopyrronium bromide pressurised metered dose inhaler (Trimbow®) for the treatment of COPD Restriction: Triple therapy should be reserved for patients who have failed to achieve or maintain an adequate response to an appropriate course of dual therapy This medicine is classified as GREEN (Restricted) for this indication Summary of supporting evidence TRILOGY shows that in patients with COPD who have severe or very severe airflow limitation,symptoms, and an exacerbation history, triple therapy with BDP/FF/GB (beclomethasone dipropionate / formoterol fumarate / glycopyrronium bromide) had a greater effect on pre-dose and 2-h post-dose FEV1 than BDP/FF. For the co-primary endpoint measuring breathlessness (Transition Dyspnea Index, TDI), superiority of BDP/FF/GB over BDP/FF was not shown. The rate of moderate-to-severe COPD exacerbations was 23% lower with BDP/FF/GB compared with BDP/FF, with the time to first exacerbation significantly longer with triple therapy. Thus, the greater improvement in lung function with BDP/FF/GB compared with BDP/FF was more clearly accompanied by a reduction in exacerbations than an improvement in breathlessness in this group of patients. Furthermore, BDP/FF/GB had a greater effect on health related quality of life than BDP/FF. TRINITY met the primary and both key secondary endpoints. Extrafine fixed triple (i.e. extra fine inhaled particle fraction, ICS/LABA/LAMA in one inhaler) resulted in a 20% (95% CI 8– 31) reduction in the rate of moderate-to-severe COPD exacerbations compared with tiotropium, together with a 0·061L mean improvement in pre-dose FEV1. -
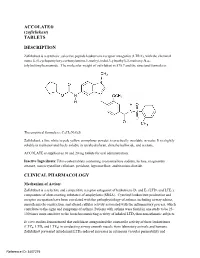
ACCOLATE® (Zafirlukast) TABLETS DESCRIPTION
ACCOLATE® (zafirlukast) TABLETS DESCRIPTION Zafirlukast is a synthetic, selective peptide leukotriene receptor antagonist (LTRA), with the chemical name 4-(5-cyclopentyloxy-carbonylamino-1-methyl-indol-3-ylmethyl)-3-methoxy-N-o tolylsulfonylbenzamide. The molecular weight of zafirlukast is 575.7 and the structural formula is: The empirical formula is: C31H33N3O6S Zafirlukast, a fine white to pale yellow amorphous powder, is practically insoluble in water. It is slightly soluble in methanol and freely soluble in tetrahydrofuran, dimethylsulfoxide, and acetone. ACCOLATE is supplied as 10 and 20 mg tablets for oral administration. Inactive Ingredients: Film-coated tablets containing croscarmellose sodium, lactose, magnesium stearate, microcrystalline cellulose, povidone, hypromellose, and titanium dioxide. CLINICAL PHARMACOLOGY Mechanism of Action: Zafirlukast is a selective and competitive receptor antagonist of leukotriene D4 and E4 (LTD4 and LTE4), components of slow-reacting substance of anaphylaxis (SRSA). Cysteinyl leukotriene production and receptor occupation have been correlated with the pathophysiology of asthma, including airway edema, smooth muscle constriction, and altered cellular activity associated with the inflammatory process, which contribute to the signs and symptoms of asthma. Patients with asthma were found in one study to be 25 100 times more sensitive to the bronchoconstricting activity of inhaled LTD4 than nonasthmatic subjects. In vitro studies demonstrated that zafirlukast antagonized the contractile activity of three leukotrienes (LTC4, LTD4 and LTE4) in conducting airway smooth muscle from laboratory animals and humans. Zafirlukast prevented intradermal LTD4-induced increases in cutaneous vascular permeability and Reference ID: 3407275 inhibited inhaled LTD4-induced influx of eosinophils into animal lungs. Inhalational challenge studies in sensitized sheep showed that zafirlukast suppressed the airway responses to antigen; this included both the early- and late-phase response and the nonspecific hyperresponsiveness. -

New Zealand Data Sheet
NEW ZEALAND DATA SHEET 1. PRODUCT NAME TRELEGY ELLIPTA 100/62.5/25 fluticasone furoate (100 micrograms)/umeclidinium (as bromide) (62.5 micrograms)/vilanterol (as trifenatate) (25 micrograms), powder for inhalation 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each delivered dose (the dose leaving the mouthpiece of the inhaler) contains 92 micrograms fluticasone furoate, 55 micrograms umeclidinium (equivalent to 65 micrograms umeclidinium [as bromide]) and 22 micrograms vilanterol (as trifenatate). This corresponds to a pre-dispensed dose of 100 micrograms fluticasone furoate, 62.5 micrograms umeclidinium (equivalent to 74.2 micrograms umeclidinium bromide) and 25 micrograms vilanterol (as trifenatate). Excipient with known effect: Each delivered dose contains approximately 25 milligrams of lactose (as monohydrate). For the full list of excipients, see Section 6.1 List of excipients. 3. PHARMACEUTICAL FORM Powder for inhalation. White powder in a light grey inhaler (Ellipta) with a beige mouthpiece cover and a dose counter. 4. CLINICAL PARTICULARS 4.1. Therapeutic indications TRELEGY ELLIPTA is indicated for the maintenance treatment of adults with moderate to severe chronic obstructive pulmonary disease (COPD) who require treatment with a long- acting muscarinic receptor antagonist (LAMA) + long-acting beta2-receptor agonist (LABA) + inhaled corticosteroid (ICS). TRELEGY ELLIPTA should not be used for the initiation of COPD treatment. 4.2. Dose and method of administration Patients can be changed from their existing inhalers to TRELEGY ELLIPTA at the next dose. However it is important that patients do not take other LABA or LAMA or ICS while taking TRELEGY ELLIPTA. A stepwise approach to the management of COPD is recommended, including the cessation of smoking and a pulmonary rehabilitation program. -

Montelukast, a Leukotriene Receptor Antagonist, Reduces the Concentration of Leukotrienes in the Respiratory Tract of Children with Persistent Asthma
Montelukast, a leukotriene receptor antagonist, reduces the concentration of leukotrienes in the respiratory tract of children with persistent asthma Benjamin Volovitz, MD,a,b Elvan Tabachnik, MD,c Moshe Nussinovitch, MD,b Biana Shtaif, MSc,b Hanna Blau, MD,a Irit Gil-Ad, PhD,b Abraham Weizman, MD,b and Itzhak Varsano, MDa,b Petah Tikva, Tel Aviv, and Rehovot, Israel Background: Leukotrienes are bronchoactive mediators secreted by inflammatory cells in the respiratory mucosa on Abbreviations used exposure to asthma triggers. BAL: Bronchoalveolar lavage Objective: We investigated the effect of montelukast, a CysLT1: Cysteinyl leukotriene 1 (receptor) leukotriene receptor antagonist, on the release of leukotrienes ECP: Eosinophilic cationic protein in the respiratory mucosa of children with persistent asthma. LTC4: Leukotriene C4 Method: Twenty-three children aged 6 to 11 years with moder- LTD4: Leukotriene D4 ately severe asthma were treated in a cross-over design start- LTE4: Leukotriene E4 ing, after a 2-week run in period, with either montelukast (n = 12) or cromolyn (n = 11) for 4 weeks with a 2-week washout period between treatments. Twelve of them were then treated Cysteinyl leukotrienes are potent proinflammatory with either montelukast or beclomethasone for 6 months. The mediators produced from a variety of inflammatory use of β -agonists was recorded on a diary card. The concen- 2 cells, including mast cells, eosinophils, basophils and tration of leukotriene C4 (LTC4) was measured by HPLC in nasal washes obtained before and at the end of each treatment macrophages. Leukotriene C4 (LTC4) is metabolized period. Eosinophilic cationic protein (ECP) was measured in enzymatically to leukotriene D4 (LTD4) and subsequent- the nasal washes by RIA. -

Asthma Medications
Relievers / Rescue / Bronchodilators Asthma Short-acting Beta Agonists 2 Medications Ipratropium Bromide ProAir ProAir RespiClick Proventil Ventolin Xopenex albuterol sulfate albuterol sulfate dry powder albuterol sulfate albuterol sulfate levalbuterol tartrate 90mcg 90mcg 90mcg 90mcg 45mcg Teva Teva Merck GlaxoSmithKline Sunovion Atrovent* Combivent Respimat* ipratropium bromide ipratropium bromide 20mcg, 17mcg albuterol sulfate 100mcg Boehringer Ingelheim Boehringer Ingelheim Nebulized Albuterol Xopenex Inhalation Solution Xopenex Inhalation Solution Xopenex Inhalation Solution * Ipratropium bromide is not a recommended rescue inhaler albuterol sulfate levalbuterol HCl levalbuterol HCl levalbuterol HCl outside of use in the emergency room or urgent care but may, 2.5mg/3mL 0.31mg/3mL 0.63mg/3mL 1.25mg/3mL on occasion, be prescribed to supplement short-acting Beta 2 generic Sunovion Sunovion Sunovion agonists. Controllers Inhaled Corticosteroids (ICS): Metered-Dose Inhalers (MDI) Aerospan Alvesco Alvesco Asmanex Asmanex Flovent Flovent Flovent flunisolide ciclesonide ciclesonide mometasone furoate mometasone furoate fluticasone propionate fluticasone fluticasone propionate 80mcg 80mcg 160mcg 100mcg 200mcg 44mcg propionate 220mcg Meda Pharmaceuticals Sunovion Sunovion Merck Merck GlaxoSmithKline 110mcg GlaxoSmithKline GlaxoSmithKline Inhaled Corticosteroids (ICS): Dry Powder Inhalers(continued on back) QVAR QVAR beclomethasone beclomethasone dipropionate dipropionate 40mcg 80mcg ArmonAir RespiClick ArmonAir RespiClick ArmonAir RespiClick -

Formoterol Fumarate) Inhalation Solution Do Not Initiate PERFOROMIST Inhalation Solution in Acutely Initial U.S
HIGHLIGHTS OF PRESCRIBING INFORMATION -----------------CONTRAINDICATIONS------------------ These highlights do not include all the information needed to use All LABA, including PERFOROMIST, are contraindicated in patients PERFOROMIST Inhalation Solution safely and effectively. See full with asthma without use of a long-term asthma control medication. (4) prescribing information for PERFOROMIST Inhalation Solution. -----------WARNINGS AND PRECAUTIONS----------- PERFOROMIST® (formoterol fumarate) Inhalation Solution Do not initiate PERFOROMIST Inhalation Solution in acutely Initial U.S. Approval: 2001 deteriorating patients. (5.2) Do not use for relief of acute symptoms. Concomitant short-acting WARNING: ASTHMA-RELATED DEATH beta2-agonists can be used as needed for acute relief. (5.2) See full prescribing information for complete boxed warning Do not exceed the recommended dose. Excessive use of Long-acting beta2-adrenergic agonists (LABA) increase the risk PERFOROMIST Inhalation Solution, or use in conjunction with other of asthma-related death. (5.1) medications containing long-acting beta2-agonists, can result in A placebo-controlled study with another long-acting beta2- clinically significant cardiovascular effects, and may be fatal. (5.3, 5.5) adrenergic agonist (salmeterol) showed an increase in asthma- Life-threatening paradoxical bronchospasm can occur. Discontinue related deaths in patients receiving salmeterol. (5.1) PERFOROMIST Inhalation Solution immediately. (5.4) The finding of an increased risk of asthma-related death with Use with caution in patients with cardiovascular or convulsive disorders, salmeterol is considered a class effect of LABA, including thyrotoxicosis, or with sensitivity to sympathomimetic drugs. (5.6, 5.7) formoterol, the active ingredient in PERFOROMIST. The safety and efficacy of PERFOROMIST in patients with asthma ------------------ADVERSE REACTIONS----------------- have not been established. -

Beta Adrenergic Agents
Beta2 Adrenergic Agents –Long Acting Review 04/10/2008 Copyright © 2007 - 2008 by Provider Synergies, L.L.C. All rights reserved. Printed in the United States of America. All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, digital scanning, or via any information storage and retrieval system without the express written consent of Provider Synergies, L.L.C. All requests for permission should be mailed to: Attention: Copyright Administrator Intellectual Property Department Provider Synergies, L.L.C. 5181 Natorp Blvd., Suite 205 Mason, Ohio 45040 The materials contained herein represent the opinions of the collective authors and editors and should not be construed to be the official representation of any professional organization or group, any state Pharmacy and Therapeutics committee, any state Medicaid Agency, or any other clinical committee. This material is not intended to be relied upon as medical advice for specific medical cases and nothing contained herein should be relied upon by any patient, medical professional or layperson seeking information about a specific course of treatment for a specific medical condition. All readers of this material are responsible for independently obtaining medical advice and guidance from their own physician and/or other medical professional in regard to the best course of treatment for their specific medical condition. This publication, inclusive of all forms contained herein, is intended to be educational in nature and is intended to be used for informational purposes only. Comments and suggestions may be sent to [email protected]. -

Strict Regio-Specificity of Human Epithelial 15-Lipoxygenase-2
Strict Regio-specificity of Human Epithelial 15-Lipoxygenase-2 Delineates its Transcellular Synthesis Potential Abigail R. Green, Shannon Barbour, Thomas Horn, Jose Carlos, Jevgenij A. Raskatov, Theodore R. Holman* Department Chemistry and Biochemistry, University of California Santa Cruz, 1156 High Street, Santa Cruz CA 95064, USA *Corresponding author: Tel: 831-459-5884. Email: [email protected] FUNDING: This work was supported by the NIH NS081180 and GM56062. Abbreviations: LOX, lipoxygenase; h15-LOX-2, human epithelial 15-lipoxygenase-2; h15-LOX-1, human reticulocyte 15-lipoxygenase-1; sLO-1, soybean lipoxygenase-1; 5-LOX, leukocyte 5-lipoxygenase; 12-LOX, human platelet 12-lipoxygenase; GP, glutathione peroxidase; AA, arachidonic acid; HETE, hydoxy-eicosatetraenoic acid; HPETE, hydroperoxy-eicosatetraenoic acid; diHETEs, dihydroxy-eicosatetraenoic acids; 5-HETE, 5-hydroxy-6E,8Z,11Z,14Z-eicosatetraenoic acid; 5-HPETE, 5-hydro peroxy-6E,8Z,11Z,14Z-eicosatetraenoic acid; 12-HPETE, 12-hydroperoxy-5Z,8Z,10E, 14Z-eicosatetraenoic acid; 15-HPETE, 15-hydroperoxy-5Z,8Z,10Z,13E- eicosatetraenoic acid; 5,15-HETE, 5S,15S-dihydroxy-6E,8Z,10Z,13E-eicosatetraenoic acid; 5,15-diHPETE, 5,15-dihydroperoxy-6E,8Z,10Z,13E-eicosatetraenoic acid; 5,6- diHETE, 5S,6R-dihydroxy-7E,9E,11Z,14Z-eicosatetraenoic acid; LTA4, 5S-trans-5,6- oxido-7E,9E,11Z,14Z-eicosatetraenoic acid; LTB4, 5S,12R-dihydroxy-6Z,8E,10E,14Z- eicosatetraenoic acid; LipoxinA4 (LxA4), 5S,6R,15S-trihydroxy-7E,9E,11Z,13E- eicosatetraenoic acid; LipoxinB4 (LxB4), 5S,14R,15S-trihydroxy-6E,8Z,10E,12E- eicosatetraenoic acid. Abstract Lipoxins are an important class of lipid mediators that induce the resolution of inflammation, and arise from transcellular exchange of arachidonic acid (AA)- derived lipoxygenase products.