Children Are Less Affected by COVID-19: a Family Case Study
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

SUBSTR DESCR International Schools CAMEROON 000944
SUBSTR DESCR International Schools CAMEROON 000944 Universite Yaounde CANADA 001048 Athabasca University 005528 Augustana University College 005516 Bishops University 005525 Concordia Lutheran College 002464 Keyano College 005536 Lethbridge Comm Coll 005536 Lethbridge Community College 002466 Prairie Bible College 009294 Red Deer College 005464 Southern Alberta Inst Tech 005464 Southrn Alb Inst Tec 005464 Southrn Alberta Inst Tech 005567 Univ Alberta 005435 Univ Alberta Calgary Branch 005435 Univ Calgary 005567 University Of Alberta 005469 University Of Lethbridge 003535 Capilano College 008792 Northern Lights Community Coll 006220 Northwest Cmty Coll 002313 Okanagan College 001054 Royal Roads Military Col 002193 Selkirk Col Castlegar Campus 002194 Selkirk Col Rosemont Campus 002195 Selkirk Col Trail Campus 005454 Selkirk College 005597 Simon Fraser University 005569 University Of British Columbia 005590 University Of Victoria 006310 Vancouver Comm College 005515 Brandon University 007078 Sal Army C Booth Bib 001058 United Col Winnipeg 005575 Univ Manitoba 001058 Univ Winnipeg 001058 Wesley Col Winnipeg 005545 Mount Allison University 001051 Universite De Moncton 005578 University Of New Brunswick 005497 Memorial Univ Newfou 005511 Acadia University 005524 Dalhousie University 005478 Mount St Vincent University 005459 Nova Scotia Agricultural Coll 001052 Nova Scotia Col Art Design 005557 St Francis Xavier University 005562 St Marys University International Schools 001057 Tech Univ Nova Scotia 001049 Univ Col Cape Breton 001055 Universite -

Paul K. Nietupski Professor of Asian Religions Department of Theology
Paul K. Nietupski Professor of Asian Religions Department of Theology & Religious Studies John Carroll University 1 John Carroll Boulevard, Cleveland, Ohio 44118-4520 216-397-4704/[email protected] Academic posts 1993-present Professor of Asian Religions, John Carroll University, Cleveland, Ohio 1991-1992 Lecturer, Department of Religion, Indiana University 1986-1987 Language Instructor, Kunming Medical College, Kunming, Yunnan, PRC 1984-1986 Language Instructor, Zunyi Medical College, Zunyi, Guizhou, PRC Publications: Monographs and edited volumes: 2015: Co-editor with Marie-Paule Hille & Bianca Horlemann. Muslims in Amdo Tibetan Society: Multidisciplinary Approaches. Lexington/Rowman & Littlefield, 2015. 2011: Co-editor with Joan O’Mara. Reading Asian Art & Artifacts: Windows to Asia on American College Campuses. Lehigh/Rowman & Littlefield, 2011. 2011: Labrang Monastery: A Tibetan Buddhist Community on the Inner Asian Borderlands 1709-1958. Lexington/Rowman & Littlefield, 2011. 1999: Labrang: A Tibetan Buddhist Monastery at the Crossroads of Four Civilizations. Ithaca: Snow Lion, 1999. Research essays: Amdo: 2015: “Islam and Labrang Monastery: A Muslim Community in a Tibetan Buddhist Estate.” In Muslims in Amdo Tibetan Society: Multidisciplinary Approaches. Edited by Marie-Paule Hille, Bianca Horlemann, & Paul K. Nietupski, 135-152. Lexington/Rowman & Littlefield, 2015. 2015: “The World According to Belmang Paṇḍīta: Belmang Könchok Gyaltsan Palzangpo (1764-1853).” In In Vimalakīrti’s House: A Festschrift in Honor of Robert A.F. Thurman on the Occasion of his 70th Birthday. Edited by Christian K. Wedemeyer, John D. Dunne, and Thomas F. Yarnall, 275-288. New York: American Institute of Buddhist Studies at Columbia University, 2015. 2014: “Understanding Sovereignty in Amdo.” In Trails of the Tibetan Tradition: Papers for Elliot Sperling. -
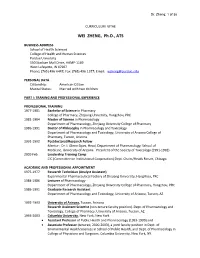
WEI ZHENG, Ph.D., ATS
Dr. Zheng: 1 of 38 CURRICULUM VITAE WEI ZHENG, Ph.D., ATS BUSINESS ADDRESS School of Health Sciences College of Health and Human Sciences Purdue University 550 Stadium Mall Drive, HAMP-1169 West Lafayette, IN 47907 Phone: (765) 496-6447; Fax: (765) 496-1377; Email: [email protected] PERSONAL DATA Citizenship: American Citizen Marital Status: Married with two children PART I: TRANING AND PROFESSIONAL EXPERIENCE PROFESSIONAL TRAINING 1977-1981 Bachelor of Science in Pharmacy College of Pharmacy, Zhejiang University, Hangzhou, PRC 1981-1984 Master of Science in Pharmacology Department of Pharmacology, Zhejiang University College of Pharmacy 1986-1991 Doctor of Philosophy in Pharmacology and Toxicology Department of Pharmacology and Toxicology, University of Arizona College of Pharmacy, Tucson, Arizona 1991-1992 Postdoctoral/Research Fellow Mentor: Dr. I. Glenn Sipes, Head, Department of Pharmacology, School of Medicine, University of Arizona. President of the Society of Toxicology (1991-1992) 2009 Feb Leadership Training Camp CIC (Committee on Institutional Cooperation) Dept. Chairs/Heads Forum, Chicago. ACADEMIC AND PROFESSIONAL APPOINTMENT 1975-1977 Research Technician (Analyst Assistant) Experimental Pharmaceutical Factory of Zhejiang University, Hangzhou, PRC 1984-1986 Lecturer of Pharmacology Department of Pharmacology, Zhejiang University College of Pharmacy, Hangzhou, PRC 1986-1991 Graduate Research Assistant Department of Pharmacology and Toxicology, University of Arizona, Tucson, AZ 1992-1993 University of Arizona, Tucson, Arizona Research Assistant Scientist (non-tenure faculty position). Dept. of Pharmacology and Toxicology, College of Pharmacy, University of Arizona, Tucson, AZ. 1993-2003 Columbia University, New York, New York • Assistant Professor of Public Health and Pharmacology (1993-1999) and • Associate Professor (tenured, 2000-2003), a joint faculty position in Dept. -

79397-89388 Payment for Watershed Services.Pdf
United Nations Development Programme Country: China PROJECT DOCUMENT Payment for Watershed Services in the Chishui River Basin for the Project Title: Conservation of Globally Significant Biodiversity UNDAF Outcome 1: Government and other stakeholders ensure environmental sustainability, Outcome(s): address climate change, and promote a green, low carbon economy Expected CP Outcome(s): Outcome 4: Low carbon and other environmentally sustainable strategies and technologies are adapted widely to meet China’s commitments and compliance with Multilateral Environmental Agreements; and Outcome 5. The vulnerability of poor communities and ecosystems to climate change is reduced Expected CPAP Output (s): Output 4.1 Policy and capacity barriers for the sustained and widespread adoption of low carbon and other environmentally sustainable strategies and technologies removed, and Output 5.1 A strengthened policy, legal, institutional framework for the sustainable use of land, water, the conservation of biodiversity, and other natural resources in fragile ecosystems is enforced. Executing Entity/Implementing Partner: Ministry of Environmental Protection Implementing Ent ity/Responsible Partners: Environmental Protection Department of Guizhou Brief Description The Chishui River is one of the most important tributaries of the upper Yangtze River, because of its diverse landscapes, richness in biodiversity and abundance in water resources. It is the only major tributary of the Upper Yangtze that remains free-flowing without a mainstream dam. The Chishui River Basin (CRB) is an important storehouse of biodiversity, lying within the Upper Yangtze Freshwater Ecoregion and the Guizhou Plateau Broadleaf and Mixed Forests Terrestrial Ecoregion. The basin also lies on the eastern margin of the Mountains of Southwest China biodiversity hotspot, and contains part of the China Danxia World Heritage Site. -

Internationale Tätigkeit
Roadshow China 2009 bis 2014 Dalian, Changchun, Tongliao Kliniken: The 3 rd Hospital of Dalian (Dalian, Provinz Liaoning) Central Hospital of Pulandian ( Dalian, Provinz Liaoning) 2nd Affiliated Hospital of Changchun , (Changchun, Provinz Jilin) People’s Hospital of Tongliao (Tongliao, Provinz Innere Mongolei) Vorträge: “Gemini SL” “Early and late infection” “Key points of TKA” Operationen: Knie: TKA mit Gemini MK II; beidseitig TKA mit Gemini MKII/PSII Hüfte: beidseitig THA LCU/TOP 2013: Bozhou, Lu’an, Anqing, Luzhou, Guiyang Kliniken: People’s Hospital of Bozhou (Bozhou, Provinz Anhui) Traditional Chinese Medicine Hospital of Lu’an (Lu’an, Provinz Anhui) Petrifaction Hospital of Anqing (Anqing, Provinz Anhui) Affiliated Hospital of Luzhou Medical School ( Luzhou, Provinz Sichuan) Provincial People Hospital of Guizhou (Guiyang, Provinz Guizhou) Vortrag: “Early infection treatment” Operationen: Knie: TKA mit Gemini 2012: Weihai, Harbin, Changchun Kliniken: 404 Hospital of Weihai (Weihai, Provinz Shandong) Fifth Municipal Hospital of Harbin (Harbin, Provinz Heilongjiang) 3rd Affiliated Hospital of Jilin University (Changchun, Provinz Jilin) Vorträge: How to treat early periprosthetic infections?” “Rats Model on the antibiotics application in infected bone” Operationen: Knie: TKA 2011: Hangzhou, Taiyuan, Changchun, Shenyang Kliniken: Xiaoshan Hospital of traditional Chinese medicine (Hangzhou, Provinz Zhejiang) Shanxi Medical Second Hospital (Taiyuan, Provinz Shanxi) Jilin First Hospital (Changchun, Provinz Jilin) -

TCMI) Combined with Oxaliplatin-Containing Chemotherapy in the Treatment of Colorectal Cancer
Int J Clin Exp Med 2018;11(10):10255-10268 www.ijcem.com /ISSN:1940-5901/IJCEM0067770 Review Article Systematic evaluation of therapeutic efficacy and safety of traditional Chinese medicine injection (TCMI) combined with oxaliplatin-containing chemotherapy in the treatment of colorectal cancer Wenqi Huang1, Zhu Yang2, Fengxi Long3, Li Luo4,6, Jinghui Wang4, Bing Yang1, Dongxin Tang5 Departments of 1Clinical, 2Principal Office, 3Graduate School, Guiyang College of TCM, Guiyang 550002, Guizhou, China; Departments of 4Oncology, 5Science and Education Section, The First Affiliated Hospital of Guiyang College of TCM, Guiyang 550001, Guizhou, China; 6Department of Oncology, Guihang Guiyang Hospital, Affiliated Guihang 300 Hospital of Zunyi Medical College, Guiyang 553009, Guizhou, China Received October 23, 2017; Accepted March 5, 2018; Epub October 15, 2018; Published October 30, 2018 Abstract: Objective: This analysis was to evaluate the therapeutic efficacy and safety of traditional Chinese medicine injection (TCMI) combined with oxaliplatin-containing chemotherapy in the treatment of colorectal cancer. Methods: PubMed, Embase, Medline, Cochrane Library, Chinese Biomedical Literature Database, China National Knowledge Infrastructure (CNKI), China Knowledge Network, Weipu Chinese Journal Database, and Wanfang Database were searched, and randomized controlled trials (RCTs) concerning the combination treatment of TCMI and oxaliplatin chemotherapy were collected. Literature screening, data extraction, and methodology quality evaluation were per- formed. Meta-analysis was conducted with RevMan 5.3 software. Results: In total, 77 RCTs were included in this study, including 9 TCMI (i.e., ADI, BJOEI, CKSI, DLSI, KAI, KLTI, SQFZI, XAPI and XGDTI) and 6014 patients. Meta- analysis showed that, compared with the chemotherapy alone, the combination with the following 7 TCMI signifi- cantly elevated the efficacy rates: CKSI, ADI, SQFZI, BJOEI, DLSI, KAI and KLTI. -

Ginsenoside-Rd Induces Cholesterol Efflux from Macrophage-Derived Foam Cells Conjunction with Cardiovascular, Pharmacological and Biochemical Evaluations
npg Section 6: Cardiovascular Pharmacology 56 10.1038/aps.2013.113 model of brain stem death that employed microinjection of the organophosphate S6.1 insecticide mevinphos bilaterally into RVLM of Sprague-Dawley rats was used, in Ginsenoside-Rd induces cholesterol efflux from macrophage-derived foam cells conjunction with cardiovascular, pharmacological and biochemical evaluations. Da-yan CAO, Ya LIU*, Xiao-hui LI*. Institute of Materia Medica and Department of Results: A significant increase in TrkB protein, phosphorylation of TrkB at Tyr516 Pharmaceutics, College of Pharmacy, Third Military Medical University, Chongqing (pTrkBY516), Shc at Tyr317 (pShcY317) or extracellular signal-regulated kinase (ERK) 400038, China at Thr202/Tyr204, or Ras activity in RVLM occurred preferentially during the pro- Aim: Ginsenoside-Rd, a purified component from panax notoginseng saponins, life phase of experimental brain stem death. Microinjection bilaterally into RVLM has been described to reduce atherosclerotic lesion formation, yet the mechanism of a specific TrkB inhibitor, K252a, antagonized those increases. Pretreatment with is not fully understood. This study is designed to investigate the potential role of anti-pShcY317 antiserum, Src homology 3 binding peptide (Grb2/SOS inhibitor), Ginsenoside-Rd in modulating cholesterol deposition and to explore its underlying farnesylthioacetic acid (Ras inhibitor), manumycin A (Ras inhibitor) or GW5074 mechanisms in macrophages. Methods: The murine macrophage-derived foam (Raf-1 inhibitor) blunted the preferential augmentation of Ras activity or ERK cells induced by 25 μg/mL oxidized low-density lipoprotein (oxLDL) in RAW264.7 phosphorylation in RVLM and blocked the upregulated nitric oxide synthase I cells for 48 h. Ginsenoside-Rd 10, 20 μmol/L was added during oxLDL incubation (NOS I)/protein kinase G (PKG) signaling, the pro-life cascade that sustains central respectively. -

CHINA Entidades Académicas Sedes, UNAM
Foro Educativo UNAM - CHINA Entidades Académicas Sedes, UNAM- IES/ Organismos Chinos Organismos Chinos Entidad Académica UNAM Principales fortalezas de la Oferta Educativa/Servicios de Organismos chinos lES/ Organismo Representante Cargo Liao Xiangzhong Vice President Communication University of China Liu Chang Associate Dean Ciencias de la Comunicación Wang Lei Teacher Facultad de Ciencias Políticas China Education Daily Li Yaoming Office Director Institución Periódica y Sociales FES Acatlan en Ji Yuan Vice Director Relaciones Internacionales CCTV News Center Televisón Caidan Yangji Journalist Ao Yuwen Professor Hulunbeier College Ciencias Políticas, Relaciones Internacionales, Ciencias de la Comunicación Guo Weizhong Deputy Dean Facultad de Química y FES Jilin Institute of Chemical Technology Sun Xiuyun Deputy President Ingeniería Química Zaragoza Cheng Jiwei Assistant President Hu Lingyun Chairman Beihang University Lu Ying Deputy Director Ingeniería Ma Qishuang Director Zhou Hong Dean Chang Yuezhu Manager Beijing University of Posts and Telecommunicaitons Tecnologías de Información Zhang Xiaoyan Vice Dean Huang Jing Vice Director Tsinghua University Lu Zhiqiang Assistant Dean Ingeniería Hao Juandi Assistant Wu Yan Project Chief Beijing University of Technology Tecnologías de Información Zhang Ailin Vice President Yang Zhixin Deputy Director Oficina de Asuntos Internacionales Hainan University Hu Xinwen Vice President Tecnologías de la Información e Ingeniería Facultad de Ingeniería e Liu Wen Director Instituto de Ingenierí, IIMAS, -

1 Please Read These Instructions Carefully
PLEASE READ THESE INSTRUCTIONS CAREFULLY. MISTAKES IN YOUR CSC APPLICATION COULD LEAD TO YOUR APPLICATION BEING REJECTED. Visit http://studyinchina.csc.edu.cn/#/login to CREATE AN ACCOUNT. • The online application works best with Firefox or Internet Explorer (11.0). Menu selection functions may not work with other browsers. • The online application is only available in Chinese and English. 1 • Please read this page carefully before clicking on the “Application online” tab to start your application. 2 • CLIC on the Edit Personal Details button. 3 • Fill out your personal information accurately. o Make sure to have a valid passport at the time of your application. o Use the name and date of birth that are on your passport. Use the name on your passport for all correspondences with the CLIC office or Chinese institutions. o List Canadian as your Nationality, even if you have dual citizenship. Only Canadian citizens are eligible for CLIC support. o Enter the mailing address for where you want your admission documents to be sent under Permanent Address. Leave Current Address blank. o Once you have completed this section click Verify and Save. 4 • Fill out your Education and Employment History accurately. o For Highest Education enter your current degree studies. o Once you have completed this section, click Verify and Save. 5 • Provide the contact information of the host Chinese university. o The contact information for summer programs is available on the CLIC website in the Program Finder. o For exchange programs, please contact your home university international office to get your host university contact information (http://clicstudyinchina.com/contact-us/). -

CONICYT Ranking Por Disciplina > Sub-Área OECD (Académicas) Comisión Nacional De Investigación 1
CONICYT Ranking por Disciplina > Sub-área OECD (Académicas) Comisión Nacional de Investigación 1. Ciencias Naturales > 1.4 Ciencias Químicas Científica y Tecnológica PAÍS INSTITUCIÓN RANKING PUNTAJE Nanyang Technological University & National Institute of Education SINGAPORE 1 5,000 (NIE) Singapore CHINA Tsinghua University 2 5,000 INDIA Indian Institute of Technology System (IIT System) 3 5,000 CHINA University of Science & Technology of China 4 5,000 CHINA Zhejiang University 5 5,000 CHINA Peking University 6 5,000 USA University of California Berkeley 7 5,000 CHINA Jilin University 8 5,000 USA Massachusetts Institute of Technology (MIT) 9 5,000 CHINA South China University of Technology 10 5,000 CHINA Suzhou University 11 5,000 USA Stanford University 12 5,000 SINGAPORE National University of Singapore 13 5,000 CHINA Nanjing University 14 5,000 CHINA Fudan University 15 5,000 SAUDI ARABIA King Abdulaziz University 16 5,000 USA University of Chicago 17 5,000 CHINA Nankai University 18 5,000 JAPAN Kyoto University 19 5,000 CHINA Shanghai Jiao Tong University 20 5,000 SWITZERLAND Ecole Polytechnique Federale de Lausanne 21 5,000 CHINA Tianjin University 22 5,000 USA Georgia Institute of Technology 23 5,000 CHINA Sichuan University 24 5,000 UNITED KINGDOM University of Cambridge 25 5,000 USA Northwestern University 26 5,000 SOUTH KOREA University of Science & Technology (UST) 27 5,000 JAPAN University of Tokyo 28 5,000 UNITED KINGDOM University of Oxford 29 5,000 CHINA Huazhong University of Science & Technology 30 5,000 CHINA Wuhan University -

2017-2018 Urap World Ranking
2017-2018 URAP WORLD RANKING World Total University Name Country Category Article Citation AIT CIT Collaboration Total Ranking Document 1 Harvard University A++ 126.00 126.00 60.00 108.00 90.00 90.00 600.00 2 University of Toronto A++ 125.00 123.97 59.00 104.53 68.03 89.00 569.53 3 University of Oxford A++ 114.82 121.50 52.38 104.21 71.96 86.38 551.26 Pierre & Marie Curie 4 A++ 121.28 115.25 52.24 98.43 64.68 87.90 539.78 University - Paris VI 5 Stanford University A++ 112.66 125.00 50.24 103.39 74.64 71.29 537.21 University College 6 A++ 117.78 114.51 54.55 98.63 65.33 85.50 536.30 London Massachusetts Institute 7 A++ 101.97 121.62 44.17 107.00 89.00 69.28 533.05 of Technology (MIT) Johns Hopkins 8 A++ 115.55 120.44 52.85 98.98 69.18 71.76 528.76 University University of 9 A++ 110.20 115.02 49.34 99.39 69.47 82.63 526.05 Cambridge University of California 10 A++ 101.95 117.30 45.71 102.33 74.47 70.85 512.61 Berkeley 11 University of Michigan A++ 115.90 113.34 52.43 97.53 64.53 68.67 512.41 University of 12 A++ 110.55 116.39 49.15 97.76 68.71 67.57 510.13 Washington Seattle University of California 13 A++ 105.86 112.10 49.26 95.49 66.72 67.88 497.30 Los Angeles University of 14 A++ 105.89 112.03 49.88 93.52 66.23 63.27 490.81 Pennsylvania 15 Columbia University A++ 104.42 108.51 47.83 92.95 65.52 67.33 486.56 Imperial College 16 A++ 104.06 105.01 47.42 88.99 62.27 78.18 485.92 London University of 17 A++ 104.78 102.49 45.40 86.53 60.84 76.86 476.90 Copenhagen University of California 18 A++ 99.23 104.39 45.37 90.07 63.94 65.52 468.52 -

E0039 Effects of Lisinopril on the Activities and Mrna Expression of Ion Pumps in Aortic Smooth Muscle Cells from Spontaneously Hypertensive Rats
GWICC Abstracts 2010 Heart: first published as 10.1136/hrt.2010.208967.39 on 17 November 2010. Downloaded from e0038 EFFECTS OF ANGIOTENSIN II ON ATPASES IN AORTIC Results The activities of Na+,K+-ATPase, Ca2+-ATPase and the + + VASCULAR SMOOTH MUSCLE CELLS FROM WISTAR-KYOTO mRNA expression levels of Na ,K -ATPase a1-subunit and PMCA1 RATS AND SPONTANEOUSLY HYPERTENSIVE RATS in ASMCs from SHR were significantly lower than those from WKY control (p<0.01). Lisinopril significantly increased the activities of doi:10.1136/hrt.2010.208967.38 Na+,K+-ATPase and Ca2+-ATPase and mRNA expression levels of + + 1Qian-Hui Shang, 1Gui-Hai Zhang, 1Qian-Feng Jiang, 2Wei-Hong Wan. 1Institute of Na ,K-ATPase a1-subunit and PMCA1 in ASMCs from SHR < Clinical Medicine, Zunyi Medical College, Department of Cardiology, Affiliated hospital (p 0.01). Ang II content of culture medium in ASMCs from SHR fi < of Zunyi Medical College; 2Key laboratory of cell engineering of Guizhou Province, was signi cantly more than those from WKY control (p 0.05), Zunyi, Guizhou, China Lisinopril attenuated Ang II content of ASMCs culture medium from SHR (p<0.05). Aim To explore the effects of Angiotensin II on the activities of Ca2 Conclusions The decreased activities of Na+,K+-ATPase and +-ATPase, Na+,K+-ATPase and mRNA expression levels of the Ca2+-ATPase may be related to their lower expression of the mRNA plasma membrane Ca2+-ATPase isoform 1 (PMCA1) and Na+,K+- in ASMCs from SHR. The Lisinopril may increase the activities of + + ATPase a1-subunit in cultured thoracic aortic vascular smooth two ion pumps and upregrulae the mRNA expression of Na ,K - muscle cells (AMSCs) from Wistar-Kyoto (WKY) rats and sponta- ATPase a1-subunit and PMCA1 in ASMCs from SHR through neously hypertensive rats (SHR).