Evaluation of Short-Term Exposure to 2.4 Ghz Radiofrequency Radiation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ECE 5011: Antennas
ECE 5011: Antennas Course Description Electromagnetic radiation; fundamental antenna parameters; dipole, loops, patches, broadband and other antennas; array theory; ground plane effects; horn and reflector antennas; pattern synthesis; antenna measurements. Prior Course Number: ECE 711 Transcript Abbreviation: Antennas Grading Plan: Letter Grade Course Deliveries: Classroom Course Levels: Undergrad, Graduate Student Ranks: Junior, Senior, Masters, Doctoral Course Offerings: Spring Flex Scheduled Course: Never Course Frequency: Every Year Course Length: 14 Week Credits: 3.0 Repeatable: No Time Distribution: 3.0 hr Lec Expected out-of-class hours per week: 6.0 Graded Component: Lecture Credit by Examination: No Admission Condition: No Off Campus: Never Campus Locations: Columbus Prerequisites and Co-requisites: Prereq: 3010 (312), or Grad standing in Engineering, Biological Sciences, or Math and Physical Sciences. Exclusions: Not open to students with credit for 711. Cross-Listings: Course Rationale: Existing course. The course is required for this unit's degrees, majors, and/or minors: No The course is a GEC: No The course is an elective (for this or other units) or is a service course for other units: Yes Subject/CIP Code: 14.1001 Subsidy Level: Doctoral Course Programs Abbreviation Description CpE Computer Engineering EE Electrical Engineering Course Goals Teach students basic antenna parameters, including radiation resistance, input impedance, gain and directivity Expose students to antenna radiation properties, propagation (Friis transmission -

25. Antennas II
25. Antennas II Radiation patterns Beyond the Hertzian dipole - superposition Directivity and antenna gain More complicated antennas Impedance matching Reminder: Hertzian dipole The Hertzian dipole is a linear d << antenna which is much shorter than the free-space wavelength: V(t) Far field: jk0 r j t 00Id e ˆ Er,, t j sin 4 r Radiation resistance: 2 d 2 RZ rad 3 0 2 where Z 000 377 is the impedance of free space. R Radiation efficiency: rad (typically is small because d << ) RRrad Ohmic Radiation patterns Antennas do not radiate power equally in all directions. For a linear dipole, no power is radiated along the antenna’s axis ( = 0). 222 2 I 00Idsin 0 ˆ 330 30 Sr, 22 32 cr 0 300 60 We’ve seen this picture before… 270 90 Such polar plots of far-field power vs. angle 240 120 210 150 are known as ‘radiation patterns’. 180 Note that this picture is only a 2D slice of a 3D pattern. E-plane pattern: the 2D slice displaying the plane which contains the electric field vectors. H-plane pattern: the 2D slice displaying the plane which contains the magnetic field vectors. Radiation patterns – Hertzian dipole z y E-plane radiation pattern y x 3D cutaway view H-plane radiation pattern Beyond the Hertzian dipole: longer antennas All of the results we’ve derived so far apply only in the situation where the antenna is short, i.e., d << . That assumption allowed us to say that the current in the antenna was independent of position along the antenna, depending only on time: I(t) = I0 cos(t) no z dependence! For longer antennas, this is no longer true. -

Compact Integrated Antennas Designs and Applications for the Mc1321x, Mc1322x, and Mc1323x
Freescale Semiconductor Document Number: AN2731 Application Note Rev. 2, 12/2012 Compact Integrated Antennas Designs and Applications for the MC1321x, MC1322x, and MC1323x 1 Introduction Contents 1 Introduction . 1 With the introduction of many applications into the 2 Antenna Terms . 2 2.4 GHz band for commercial and consumer use, 3 Basic Antenna Theory . 3 Antenna design has become a stumbling point for many 4 Impedance Matching . 5 customers. Moving energy across a substrate by use of an 5 Antennas . 8 RF signal is very different than moving a low frequency 6 Miniaturization Trade-offs . 11 voltage across the same substrate. Therefore, designers 7 Potential Issues . 12 who lack RF expertise can avoid pitfalls by simply 8 Recommended Antenna Designs . 13 following “good” RF practices when doing a board 9 Design Examples . 14 layout for 802.15.4 applications. The design and layout of antennas is an extension of that practice. This application note will provide some of that basic insight on board layout and antenna design to improve our customers’ first pass success. Antenna design is a function of frequency, application, board area, range, and costs. Whether your application requires the absolute minimum costs or minimization of board area or maximum range, it is important to understand the critical parameters so that the proper trade-offs can be chosen. Some of the parameters necessary in selecting the correct antenna are: antenna © Freescale Semiconductor, Inc., 2005, 2006, 2012. All rights reserved. tuning, matching, gain/loss, and required radiation pattern. This note is not an exhaustive inquiry into antenna design. It is instead, focused toward helping our customers understand enough board layout and antenna basics to aid in selecting the correct antenna type for their application as well as avoiding the typical layout mistakes that cause performance issues that lead to delays. -

Performance Expectations for Reduced-Size Antennas
High Frequency Design From February 2010 High Frequency Electronics Copyright © 2010 Summit Technical Media, LLC SMALL ANTENNAS Performance Expectations for Reduced-Size Antennas By Gary Breed Editorial Director λ very device that L/ = 0.167 and RRad = 5.5 ohms. The feed- This month’s tutorial article transmits and/or point impedance will be 5.5 –jX, where X is a presents a summary of Ereceives radio sig- large capacitance, as high as 1500 ohms in the the advantages and limita- nals needs an antenna. case of thin dipole. This 5.5 –j1500 ohm tions of electrically-small When that device has a impedance must be matched to the system antennas like those used in small size or limited impedance, typically 50 ohms. many wireless devices space for a classic reso- Small loops and monopoles have similarly nant antenna, various low radiation resistance with high reactance. techniques are used to implement reduced- Matching to highly reactive loads is inherent- size antennas. Those techniques may include ly narrow bandwidth, since the magnitude of inductive or capacitive loading, meandered or the reactance changes rapidly with frequency. spiral construction, high dielectric constant Achieving a broader bandwidth match materials to slow down wave propagation, and requires either complex networks or the intro- embedded structures incorporated into the duction of lossy components. packaging. Each of these methods imposes The use of meandered lines, spirals, fractal some type of limitation when compared to patterns effectively distribute the required monopole, dipole, or resonant loop antennas. inductance over the length of the antenna, This tutorial looks at the key limitations of and can result in higher radiation resistance small antennas, with the intention of illus- and lower loss matching networks. -

Range Calculation for 300Mhz to 1000Mhz Communication Systems
APPLICATION NOTE Range Calculation for 300MHz to 1000MHz Communication Systems RANGE CALCULATION Description For restricted-power UHF* communication systems, as defined in FCC Rules and Regula- tions Title 47 Part 15 Subpart C “intentional radiators*”, communication range capability is a topic which generates much interest. Although determined by several factors, communica- tion range is quantified by a surprisingly simple equation developed in 1946 by H.T. Friis of Denmark. This paper begins by introducing the Friis Transmission Equation and examining the terms comprising it. Then, real-world-environment factors which influence RF commu- nication range and how they affect a “Link Budget*” are investigated. Following that, some methods for optimizing RF-link range are given. Range-calculation spreadsheets, including the special case of RKE, are presented. Finally, information concerning FCC rules govern- ing “intentional radiators”, FCC-established radiation limits, and similar reference material is provided. Section 7. “Appendix” on page 13 includes definitions (words are marked with an asterisk *) and formulas. Note: “For additional information, two excel spreadsheets, RKE Range Calculation (MF).xls and Generic Range Calculation.xls, have been attached to this PDF. To open the attachments, in the Attachments panel, select the attachment, and then click Open or choose Open Attachment from the Options menu. For addi- tional information on attachments, please refer to Adobe Acrobat Help menu“ 9144C-RKE-07/15 1. The Friis Transmission Equation For anyone using a radio to communicate across some distance, whatever the type of communication, range capability is inevitably a primary concern. Whether it is a cell-phone user concerned about dropped calls, kids playing with their walkie- talkies, a HAM radio operator with VHF/UHF equipment providing emergency communications during a natural disaster, or a driver opening a garage door from their car in the pouring rain, an expectation for reliable communication always exists. -
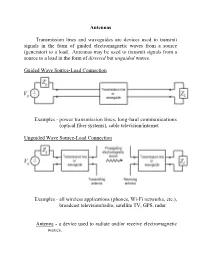
Antennas Transmission Lines and Waveguides Are Devices Used To
Antennas Transmission lines and waveguides are devices used to transmit signals in the form of guided electromagnetic waves from a source (generator) to a load. Antennas may be used to transmit signals from a source to a load in the form of directed but unguided waves. Guided Wave Source-Load Connection Examples - power transmission lines, long-haul communications (optical fiber systems), cable television/internet Unguided Wave Source-Load Connection Examples - all wireless applications (phones, Wi-Fi networks, etc.), broadcast television/radio, satellite TV, GPS, radar Antenna - a device used to radiate and/or receive electromagnetic waves. Major Classes of Antennas Wire Antennas - monopole, dipole, loop, helical Aperture Antennas - horn, slot, microstrip patch Reflector Antennas - parabolic dish, corner reflector Antenna Characteristics Antenna impedance - an antenna must be matched to the connecting transmission line or waveguide for efficient radiation or reception. Radiated power - the amount of power radiated by a transmit antenna will limit the separation distance between the transmit and receive antennas. Directivity - the direction in which an antenna radiates or receives power will dictate how the transmit and receive antennas should be positioned (the radiation pattern of the antenna defines the antenna radiated power as a function of direction). Efficiency (losses) - the amount of power dissipated by the antenna should be small in comparison to the amount of power radiated in order to minimize the source power requirements. Reciprocity - most antennas are reciprocal (radiation characteristics are equivalent to the reception characteristics). Examples of non-reciprocal antennas are those containing nonlinear materials. Polarization - the orientation of the fields radiated by the antenna define the antenna polarization. -

Principles of Radiation and Antennas
RaoCh10v3.qxd 12/18/03 5:39 PM Page 675 CHAPTER 10 Principles of Radiation and Antennas In Chapters 3, 4, 6, 7, 8, and 9, we studied the principles and applications of prop- agation and transmission of electromagnetic waves. The remaining important topic pertinent to electromagnetic wave phenomena is radiation of electromag- netic waves. We have, in fact, touched on the principle of radiation of electro- magnetic waves in Chapter 3 when we derived the electromagnetic field due to the infinite plane sheet of time-varying, spatially uniform current density. We learned that the current sheet gives rise to uniform plane waves radiating away from the sheet to either side of it. We pointed out at that time that the infinite plane current sheet is, however, an idealized, hypothetical source. With the ex- perience gained thus far in our study of the elements of engineering electro- magnetics, we are now in a position to learn the principles of radiation from physical antennas, which is our goal in this chapter. We begin the chapter with the derivation of the electromagnetic field due to an elemental wire antenna, known as the Hertzian dipole. After studying the radiation characteristics of the Hertzian dipole, we consider the example of a half-wave dipole to illustrate the use of superposition to represent an arbitrary wire antenna as a series of Hertzian dipoles to determine its radiation fields.We also discuss the principles of arrays of physical antennas and the concept of image antennas to take into account ground effects. Next we study radiation from aperture antennas. -

The Hertzian Dipole Antenna
24. Antennas What is an antenna Types of antennas Reciprocity Hertzian dipole near field far field: radiation zone radiation resistance radiation efficiency Antennas convert currents to waves An antenna is a device that converts a time-varying electrical current into a propagating electromagnetic wave. Since current has to flow in the antenna, it has to be made of a conductive material: a metal. And, since EM waves have to propagate away from the antenna, it needs to be embedded in a transparent medium (e.g., air). Antennas can also work in reverse: converting incoming EM waves into an AC current. That is, they can work in either transmit mode or receive mode. Antennas need electrical circuits • In order to drive an AC current in the antenna so that it can produce an outgoing EM wave, • Or, in order to detect the AC current created in the antenna by an incoming wave, …the antenna must be connected to an electrical circuit. Often, people draw illustrations of antennas that are simply floating in space, unattached to anything. Always remember that there needs to be a wire connecting the antenna to a circuit. Bugs also have antennas. But not the kind we care about. not made of metal The word “antenna” comes from the Italian word for “pole”. Marconi used a long wire hanging from a tall pole to transmit and receive radio signals. His use of the term popularized it. The antenna used by Marconi for the first trans-Atlantic radio broadcast (1902) Guglielmo Marconi 1874-1937 There are many different types of antennas • Omnidirectional antennas – designed to receive or broadcast power more or less in all directions (although, no antenna broadcasts equally in every direction) • Directional antennas – designed to broadcast mostly in one direction (or receive mostly from one direction) Examples of omnidirectional antennas, typically used for receiving radio or TV broadcasts. -
Chapter 31: Antenna Parameters
Chapter 31: Antenna Parameters Chapter Learning Objectives: After completing this chapter the student will be able to: Calculate the input impedance, half-power beam width, directivity, gain, and effective area of an antenna. Use the Friis equation to find power available at the output terminals of a receiving antenna. You can watch the video associated with this chapter at the following link: Historical Perspective: Edwin Hubble (1889-1953) was an American astronomer who used radio telescopes to discover galaxies outside the Milky Way and to prove that the universe is expanding by observing the red shift of distant galaxies. The Hubble Space Telescope is named after him. Photo credit: https://commons.wikimedia.org/wiki/File:Edwin-hubble.jpg, [Public domain], via Wikimedia Commons. 1 31.1 Input Impedance We spent quite a lot of time earlier discussing how to match the impedance of a transmission line to its load. During those discussions, we tended to think of the load as unchangeable, provided to us by a customer, and we had to find a way to match it to the line. But now our focus is shifting, and we see that the load is often an antenna. This, of course, raises the question, “What is the input impedance of an antenna? Figure 31.1 shows an AC source Vs connected to an antenna with input impedance ZL through a transmission line of length L with characteristic impedance ZC. i(z,t)=I0cost(wt-kz) Vs ZC ZL L Figure 31.1. An Antenna Serving as a Load If we draw a sphere around the antenna and integrate the power radiating through the sphere, this will give the total power radiated away from the antenna. -

Antenna with Semicircular Radiation Diagram for 2.4 Ghz Introduction N
AMOS Antenna with Semicircular Radiation Diagram for 2.4 GHz Dragoslav Dobričić, YU1AW Introduction n WiFi communications, antennas with semicircular radiation diagram in the horizontal plane are often needed. Antennas with circular radiation diagrams may have gain values as I high, as it is possible to narrow its vertical radiation diagram. That's where antennas with radiating dipoles aligned vertically are used. When a circular diagram is needed, and vertical polarization is used, the alignment of half-wave dipoles can be carried out according to the principle of the famous Franklin's antenna. An open half-wave dipole fed in the middle is extended on both sides with one continuous conductor, which is, every half wavelength, folded into a quarter-wave short-circuited part of symmetrical two wire line. In this way, proper phasing of the half wave dipoles is performed. This kind of wire antenna has been used, mainly in horizontal polarization, from the very beginnings of radio on medium and short waves and is known as Franklin’s antenna, after its author. Horizontal Franklin antenna The problem with impedance and parasitic radiation of phasing lines This antenna is often used on VHF and UHF bands in vertical polarization, which yields a circular radiation diagram. However, with the increase of frequency, problems arise with phasing lines among dipoles, because they physically enlarge in relation to wavelength, which consequently leads to greater impact of the radiation from this part of the antenna on the overall diagram of the antenna. This unwanted, parasitic radiation of the phasing lines has been resolved in many ways (by wrapping the two-wire line around the antenna axis, by the replacement of the two-wire line with a coil or capacitor, etc.) with more or less success. -

EE302 Lesson 13: Antenna Fundamentals
EE302 Lesson 13: Antenna Fundamentals Antennas An antenna is a device that provides a transition between guided electromagnetic waves in wires and electromagnetic waves in free space. 1 Reciprocity Antennas can usually handle this transition in both directions (transmitting and receiving EM waves). This property is called reciprocity. Antenna physical characteristics The antenna’s size and shape largely determines the frequencies it can handle and how it radiates electromagnetic waves. 2 Antenna polarization The polarization of an antenna refers to the orientation of the electric field it produces. Polarization is important because the receiving antenna should have the same polarization as the transmitting antenna to maximize received power. Antenna polarization Horizontal Polarization Vertical Polarization Circular Polarization Electric and magnetic field rotate at the frequency of the transmitter Used when the orientation of the receiving antenna is unknown Will work for both vertical and horizontal antennas Right Hand Circular Polarization (RHCP) Left Hand Circular Polarization (LHCP) Both antennas must be the same orientation (RHCP or LHCP) 3 Wavelength () You may recall from physics that wavelength () and frequency (f ) of an electromagnetic wave in free space are related by the speed of light (c) c cf or f Therefore, if a radio station is broadcasting at a frequency of 100 MHz, the wavelength of its signal is given c 3.0 108 m/s 3 m f 100 106 cycle/s Wavelength and antennas The dimensions of an antenna are usually expressed in terms of wavelength (). Low frequencies imply long wavelengths, hence low frequency antennas are very large. High frequencies imply short wavelengths, hence high frequency antennas are usually small. -

Antennas in Practice
Antennas in Practice EM fundamentals and antenna selection Alan Robert Clark Andr´eP C Fourie Version 1.4, December 23, 2002 ii Titles in this series: Antennas in Practice: EM fundamentals and antenna selection (ISBN 0-620-27619-3) Wireless Technology Overview: Modulation, access methods, standards and systems (ISBN 0-620-27620-7) Wireless Installation Engineering: Link planning, EMC, site planning, lightning and grounding (ISBN 0-620-27621-5) Copyright °c 2001 by Alan Robert Clark and Poynting Innovations (Pty) Ltd. 33 Thora Crescent Wynberg Johannesburg South Africa. www.poynting.co.za Typesetting, graphics and design by Alan Robert Clark. Published by Poynting Innovations (Pty) Ltd. This book is set in 10pt Computer Modern Roman with a 12 pt leading by LATEX 2". All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording, or otherwise, without the prior written permission of Poynting Innovations (Pty) Ltd. Printed in South Africa. ISBN 0-620-27619-3 Contents 1 Electromagnetics 1 1.1 Transmission line theory . 1 1.1.1 Impedance . 3 1.1.2 Characteristic impedance & Velocity of propagation . 3 Two-wire line . 4 One conductor over ground plane . 5 Twisted Pair . 5 Coaxial line . 5 Microstrip Line . 6 Slotline . 6 1.1.3 Impedance transformation . 6 1.1.4 Standing Waves, Impedance Matching and Power Transfer 8 1.2 The Smith Chart . 9 1.3 Field Theory . 10 1.3.1 Frequency and wavelength . 10 1.3.2 Characteristic impedance & Velocity of propagation .