Recent Advances Targeting CCR5 for Cancer and Its Role in Immuno-Oncology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
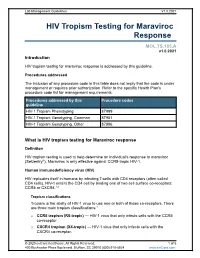
HIV Tropism Testing for Maraviroc Response
Lab Management Guidelines V1.0.2021 HIV Tropism Testing for Maraviroc Response MOL.TS.185.A v1.0.2021 Introduction HIV tropism testing for maraviroc response is addressed by this guideline. Procedures addressed The inclusion of any procedure code in this table does not imply that the code is under management or requires prior authorization. Refer to the specific Health Plan's procedure code list for management requirements. Procedures addressed by this Procedure codes guideline HIV-1 Tropism Phenotyping 87999 HIV-1 Tropism Genotyping, Common 87901 HIV-1 Tropism Genotyping, Other 87906 What is HIV tropism testing for Maraviroc response Definition HIV tropism testing is used to help determine an individual's response to maraviroc (Selzentry®). Maraviroc is only effective against CCR5-tropic HIV-1. Human immunodeficiency virus (HIV) HIV replicates itself in humans by infecting T-cells with CD4 receptors (often called CD4 cells). HIV-1 enters the CD4 cell by binding one of two cell surface co-receptors: CCR5 or CXCR4.1,2 Tropism classifications Tropism is the ability of HIV-1 virus to use one or both of these co-receptors. There are three main tropism classifications:3 o CCR5 tropism (R5-tropic) — HIV-1 virus that only infects cells with the CCR5 co-receptor. o CXCR4 tropism (X4-tropic) — HIV-1 virus that only infects cells with the CXCR4 co-receptor. © 2020 eviCore healthcare. All Rights Reserved. 1 of 5 400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924 www.eviCore.com Lab Management Guidelines V1.0.2021 o Dual or mixed tropism (D/M-tropic) — HIV-1 virus populations that can use either co-receptor to infect cells. -

Download Article PDF/Slides
Kan Lu, PharmD New Antiretrovirals for Based on a presentation at prn by Roy M. Gulick, md, mph the Treatment of HIV: Kan Lu, PharmD | Drug Development Fellow University of North Carolina School of Pharmacy Chapel Hill, North Carolina The View in 2006 Roy M. Gulick, md, mph Reprinted from The prn Notebook® | october 2006 | Dr. James F. Braun, Editor-in-Chief Director, Cornell Clinical Trials Unit | Associate Professor of Medicine, Meri D. Pozo, PhD, Managing Editor. Published in New York City by the Physicians’ Research Network, Inc.® Weill Medical College of Cornell University | New York, New York John Graham Brown, Executive Director. For further information and other articles available online, visit http://www.prn.org | All rights reserved. ©october 2006 substantial progress continues to be made in the arena of cokinetics and a long extracellular half-life of approximately 10 hours antiretroviral drug development. prn is again proud to present its annual (Zhu, 2003). During apricitabine’s development, a serious drug interac- review of the experimental agents to watch for in the coming months and tion with lamivudine (Epivir) was noted. Although the plasma years. This year’s review is based on a lecture by Dr. Roy M. Gulick, a long- concentrations of apricitabine were unaffected by coadministration of time friend of prn, and no stranger to the antiretroviral development lamivudine, the intracellular concentrations of apricitabine were reduced pipeline. by approximately sixfold. Additionally, the 50% inhibitory concentration To date, twenty-two antiretrovirals have been approved by the Food (ic50) of apricitabine against hiv with the M184V mutation was increased and Drug Administration (fda) for the treatment of hiv infection. -

Cenicriviroc CSF Abstract Page 1 of 3 Title: Cerebrospinal Fluid Exposure
Cenicriviroc CSF Abstract Title: Cerebrospinal fluid exposure of cenicriviroc in HIV-positive individuals with cognitive impairment Authors: Jasmini Alagaratnam1, Laura Else2, Sujan Dilly Penchala2, Elizabeth Challenger2, Ken Legg1, Claire Petersen1, Brynmor Jones3, Ranjababu Kulasegaram4, Star Seyedkazemi5, Eric Lefebvre5, Saye Khoo2 and Alan Winston1 1. Division of Infectious Diseases, Department of Medicine, Imperial College London, London W2 1PG 2. Department of Pharmacology, University of Liverpool, Liverpool L69 7SX, UK 3. Department of Radiology, Imperial College Healthcare NHS Trust, London W2 1NY 4. St. Thomas’ Hospital, London W6 8RP, UK 5. Clinical Development, Allergan plc, South San Francisco, USA Page 1 of 3 Cenicriviroc CSF Abstract Abstract Background: Cenicriviroc, a dual C-C chemokine receptor type 2 (CCR2) and type 5 (CCR5) antagonist, is a potential adjunctive therapy, along with antiretroviral therapy (ART), for the management of HIV-associated cognitive disorders. Materials and Methods: Virologically suppressed persons living with HIV (PLWH) with a clinical diagnosis of HIV-related cognitive impairment intensified ART with cenicriviroc once daily, dose dependent on current ART, for eight weeks. Subjects with current or previous use of CCR5 inhibitors were not eligible. We assessed cerebrospinal fluid (CSF) exposure of cenicriviroc and CSF albumin at week 8, and changes in cognitive function over 8 weeks. Cenicriviroc concentration was determined using reverse phase high-performance liquid chromatography (HPLC) with geometric mean (GM) and 95% confidence intervals (CI) calculated. The proposed cenicriviroc target concentration was above the 90% effective concentration (EC90) for cenicriviroc (0.17 ng/mL), with the lower limit of quantification (LLQ) 0.24 ng/mL taken as target concentration. -

Review CCR5 Antagonists: Host-Targeted Antivirals for the Treatment of HIV Infection
Antiviral Chemistry & Chemotherapy 16:339–354 Review CCR5 antagonists: host-targeted antivirals for the treatment of HIV infection Mike Westby* and Elna van der Ryst Pfizer Global R&D, Kent, UK *Corresponding author: Tel: +44 1304 649876; Fax: +44 1304 651819; E-mail: [email protected] The human chemokine receptors, CCR5 and suggest that these compounds have a long plasma CXCR4, are potential host targets for exogenous, half-life and/or prolonged CCR5 occupancy, which small-molecule antagonists for the inhibition of may explain the delay in viral rebound observed HIV-1 infection. HIV-1 strains can be categorised by following compound withdrawal in short-term co-receptor tropism – their ability to utilise CCR5 monotherapy studies. A switch from CCR5 to (CCR5-tropic), CXCR4 (CXCR4-tropic) or both (dual- CXCR4 tropism occurs spontaneously in approxi- tropic) as a co-receptor for entry into susceptible mately 50% of HIV-infected patients and has been cells. CCR5 may be the more suitable co-receptor associated with, but is not required for, disease target for small-molecule antagonists because a progression. The possibility of a co-receptor natural deletion in the CCR5 gene preventing its tropism switch occurring under selection pressure expression on the cell surface is not associated by CCR5 antagonists is discussed. The completion with any obvious phenotype, but can confer of ongoing Phase IIb/III studies of maraviroc, resistance to infection by CCR5-tropic strains – the aplaviroc and vicriviroc will provide further insight most frequently sexually-transmitted strains. into co-receptor tropism, HIV pathogenesis and The current leading CCR5 antagonists in clinical the suitability of CCR5 antagonists as a potent development include maraviroc (UK-427,857, new class of antivirals for the treatment of HIV Pfizer), aplaviroc (873140, GlaxoSmithKline) and infection. -

Product Monograph for CELSENTRI
PRODUCT MONOGRAPH PrCELSENTRI maraviroc Tablets 150 and 300 mg CCR5 antagonist ViiV Healthcare ULC 245, boulevard Armand-Frappier Laval, Quebec H7V 4A7 Date of Revision: July 05, 2019 Submission Control No: 226222 © 2019 ViiV Healthcare group of companies or its licensor. Trademarks are owned by or licensed to the ViiV Healthcare group of companies. Page 1 of 60 Table of Contents PART I: HEALTH PROFESSIONAL INFORMATION.........................................................3 SUMMARY PRODUCT INFORMATION ........................................................................3 INDICATIONS AND CLINICAL USE..............................................................................3 CONTRAINDICATIONS ...................................................................................................3 WARNINGS AND PRECAUTIONS..................................................................................4 ADVERSE REACTIONS....................................................................................................9 DRUG INTERACTIONS ..................................................................................................19 DOSAGE AND ADMINISTRATION..............................................................................28 OVERDOSAGE ................................................................................................................31 ACTION AND CLINICAL PHARMACOLOGY ............................................................31 STORAGE AND STABILITY..........................................................................................36 -

Emerging Therapies in NASH
Emerging Therapies in NASH Stephen A Harrison, MD, FACP, FAASLD COL (ret.), USA, MC Visiting Professor of Hepatology Radcliffe Department of Medicine, University of Oxford Medical Director, Pinnacle Clinical Research President, Summit Clinical Research San Antonio, TX Disclosures • Scientific advisor or consultant for Akero, Alentis, Altimmune, Arrowhead, Axcella, Canfite, Cirius, CiVi Biopharma, Cymabay, Echosens, Fibronostics, Forest Labs, Galectin, Genfit, Gilead, Hepion, HistoIndex, Intercept, Madrigal, Medpace, Metacrine, NGM Bio, Northsea, Novartis, Novo Nordisk, PathAI, Poxel, Liminal, Ridgeline, Sagimet, Terns, Viking, 89 Bio. • Stock options: Akero, Cirius, Galectin, Genfit, Hepion, HistoIndex, PathAI, Metacrine, NGM Bio, Northsea. • Grant/Research support: Akero, Axcella, BMS, Cirius, CiVi Biopharma, Conatus, Cymabay, Enyo, Galectin, Genentech, Genfit, Gilead, Hepion, Hightide, Intercept, Madrigal, Metacrine, NGM Bio, Novartis, Novo Nordisk, Northsea, Pfizer,Sagimet, Viking. Goals of NASH Treatment • Improve metabolic abnormalities • Decrease inflammation • Prevent/arrest/reverse liver fibrosis – AASLD recommends pharmacological treatments aimed primarily at improving liver disease should generally be limited to those with biopsy-proven NASH and fibrosis • Prevent advanced liver disease, liver failure, liver cancer and related outcomes • Systemic outcomes (eventually) Chalasani N et al. Hepatology. 2018;67:328-35. Lifestyle Recommendations for Treating NASH Caloric intake Weight loss Exercise No heavy alcohol reduction of 3% -

Microbicides 2008
State of the Network Ian McGowan & Sharon Hillier Annual Meeting March 14th, 2016 HIV Infection in the US HIV Infection in US MSM HIV Infection in US Women Global HIV Infection HIV Incidence Rates in ASPIRE & RING Studies ASPIRE Study RING Study 10 8 6 4 2 HIV Incidence Rates (%) Rates Incidence HIV 0 <21 years > 25 years 18-21 years22-26 years27-45 years 21-25 years The PrEP Landscape in 2016 (1) • Oral PrEP – Optimization of Truvada delivery – Increasing availability – US, Canada, France, South Africa, Kenya, Israel – 2nd generation regimens being evaluated • Maraviroc combinations • Tenofovir alafenamide – New molecules • EFdA (Merck) The PrEP Landscape in 2016 (2) • Injectable PrEP – Rilpivirine & Cabotegravir • Intravaginal rings – Phase 3 • Dapivirine – Phase 1/2 • Tenofovir • Tenofovir disoproxil fumarate • Vicriviroc + MK 2048 • Dapivirine + Levonorgestrol The PrEP Landscape in 2016 (3) • Rectal microbicides – Phase 2 • Reduced glycerin tenofovir gel – Phase 1 • Maraviroc • Dapivirine • Griffithsin • MIV-150 / Carageenan / Zinc • Implantable PrEP MTN Highlights from the Past Year The MTN Portfolio 2015 / 2016 Studies in Ongoing development: Completed studies MTN-026 studies MTN-030 MTN-015 MTN-031 MTN-017 MTN-016 MTN-032 MTN-020 MTN-023 MTN-033 MTN-024 MTN-027 MTN-028 MTN-034 MTN-029 MTN-035 MTN-036 MTN-037 Intravaginal Ring Studies • Dapivirine • Vicriviroc / MK-2048 – MTN-020 – MTN-027 & MTN-028 – MTN-023 • Dapivirine 200 mg – MTN-025 (HOPE) IVR – MTN-029 – MTN-036 / IPM 047 – MTN-031 – MTN-034 • Dapivirine / Levonorgestrel – MTN-030 / IPM 041 Rectal Microbicide Studies • Tenofovir gel – MTN-017 • Dapivirine gel – MTN-026 – MTN-033 – MTN-035 CHARM-02 Study (Hiruy H et al. -
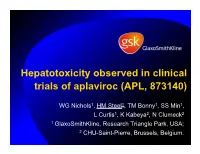
Aplaviroc (APL, 873140)
Hepatotoxicity observed in clinical trials of aplaviroc (APL, 873140) WG Nichols1, HM Steel1, TM Bonny1, SS Min1, L Curtis1, K Kabeya2, N Clumeck2 1 GlaxoSmithKline, Research Triangle Park, USA; 2 CHU-Saint-Pierre, Brussels, Belgium. Aplaviroc (APL, 873140, Ono 4128) O CH3 O HO • Specific CCR5 antagonist O N OH N NH • Potent HIV entry inhibitor O – mean 1.66 log10 decline at nadir in HIV-RNA after 10d monotherapy1 • Safety profile supported further study in humans 1 Lalezari J et al. AIDS 2005;19:1443–1448. Aplaviroc Phase 2b Program CCR100136 CCR102881 • 195 treatment-naïve • 147 treatment-naïve subjects randomized to subjects randomized to – APL 200mg BID / LPV/r – APL 600mg BID / Combivir – APL 400mg BID / LPV/r – APL 800mg BID / Combivir – APL 800mg QD / LPV/r – Combivir / efavirenz – LPV/r / Combivir – 2:2:1 randomisation – 2:2:2:1 randomization Sentinel case: Severe hepatitis • 39 year old HIV+ male – CD4 283 cells/mm3 – HBV/HCV negative – Normal AST/ALT/bilirubin • APL 800mg BID + COM • Day 59: developed severe hepatic cytolysis • Liver biopsy: – Chronic inflammatory infiltrate, mod intensity Liver biopsy (portal area) – Consistent with drug-induced hepatotoxicity CCR102881 Individual Patient LFT Plots ALP ALT AST BILT CK 70 60 50 40 30 APL RX 20 LFT Values (x ULN) 10 0 -50 -40 -30 -20 -10 0 10 20 30 40 50 60 70 80 90 100 Study Day Review of Liver Enzyme Elevations in APL Phase IIb trials • 336 subjects received treatment – 282 subjects on APL – median duration of therapy: 13 wks • Central Lab database query to identify – any Grade -

Ana Rita Ramos Diniz De Quadros E Costa
UNIVERSIDADE DE LISBOA FACULDADE DE FARMÁCIA ! NEW PREVENTION AND TREATMENT STRATEGIES FOR HIV INFECTION Ana Rita Ramos Diniz de Quadros e Costa Orientadores: Prof. Doutor Nuno Eduardo Moura dos Santos Taveira Prof. Doutor José António Frazão Moniz Pereira Tese especialmente elaborada para a obtenção do grau de Doutor em Farmácia, especialidade Microbiologia 2018 UNIVERSIDADE DE LISBOA FACULDADE DE FARMÁCIA ! NEW PREVENTION AND TREATMENT STRATEGIES FOR HIV INFECTION Ana Rita Ramos Diniz de Quadros e Costa Orientadores: Prof. Doutor Nuno Eduardo Moura dos Santos Taveira Prof. Doutor José António Frazão Moniz Pereira Tese especialmente elaborada para a obtenção do grau de Doutor em Farmácia, especialidade Microbiologia Júri Presidente: Doutora Matilde da Luz dos Santos Duque da Fonseca e Castro, Professora Catedrática e Diretora da Faculdade de Farmácia da Universidade de Lisboa, Presidente do júri por delegação de competências; Vogais: Doutor Bruno Filipe Carmelino Cardoso Sarmento, Investigador Auxiliar do Instituto de Investigação e Inovação em Saúde da Universidade do Porto; Doutor Nuno Eduardo Moura dos Santos Costa Taveira, Professor Catedrático do Instituto Universitário Egas Moniz, Orientador; Doutora Maria Helena de Sousa Barroso, Professora Associada do Instituto Universitário Egas Moniz; Doutora Emília de Jesus da Encarnação Valadas, Professora Associada da Faculdade de Medicina da Universidade de Lisboa; Doutor João Manuel Braz Gonçalves. Professor Associado com Agregação da Faculdade de Farmácia da Universidade de Lisboa. 2018 Todas as afirmações efetuadas no presente documento são da exclusiva responsabilidade da sua autora, não cabendo qualquer responsabilidade à Faculdade de Farmácia, Universidade de Lisboa pelos conteúdos nele apresentados. Ana Rita Ramos Diniz de Quadros e Costa teve o apoio financeiro da Fundação para a Ciência e Tecnologia através de uma bolsa de doutoramento (SFRH/BD/89140/2012). -

Semen-Mediated Enhancement of HIV-1 Infection Markedly Impairs the Antiviral Efficacy of Microbicides
Institute of Molecular Virology Ulm University Medical Center Prof. Dr. Frank Kirchhoff Semen-mediated enhancement of HIV-1 infection markedly impairs the antiviral efficacy of microbicides Dissertation to obtain the Doctoral Degree of Human Biology (Dr. biol. hum.) at the Faculty of Medicine, University of Ulm presented by Onofrio Zirafi Heidenheim an der Brenz 2014 Present Dean: Prof. Dr. Thomas Wirth 1st reviewer: Prof. Dr. Jan Münch 2nd reviewer: Prof. Dr. Barbara Spellerberg Date of graduation: 5th December 2014 TABLE OF CONTENTS III TABLE OF CONTENTS ABBREVIATIONS ............................................................................................................. V 1 INTRODUCTION ....................................................................................................... 1 1.1 HIV LIFE CYCLE AND ANTIRETROVIRAL DRUGS .......................................................... 2 1.2 HIV TRANSMISSION ................................................................................................... 4 1.3 FACTORS IN SEMEN MODULATING HIV-1 INFECTION .................................................. 5 1.4 MECHANISM OF INFECTION ENHANCEMENT BY SEMINAL AMYLOIDS ........................... 6 1.5 COUNTERACTING AMYLOID-MEDIATED ENHANCEMENT OF HIV-1 INFECTION ............ 6 1.6 STRUCTURE-BASED PEPTIDE INHIBITORS OF AMYLOID FORMATION ............................. 7 1.7 MICROBICIDES ............................................................................................................ 8 1.8 SCIENTIFIC AIM ........................................................................................................ -

Investor Presentation
Participants Company overview Pharmaceuticals Oncology Financial review Conclusion Appendix References Q1 2021 Results Investor presentation 1 Investor Relations │ Q1 2021 Results Participants Company overview Pharmaceuticals Oncology Financial review Conclusion Appendix References Disclaimer This presentation contains forward-looking statements within the meaning of the United States Private Securities Litigation Reform Act of 1995, that can generally be identified by words such as “potential,” “expected,” “will,” “planned,” “pipeline,” “outlook,” or similar expressions, or by express or implied discussions regarding potential new products, potential new indications for existing products, potential product launches, or regarding potential future revenues from any such products; or regarding the impact of the COVID-19 pandemic on certain therapeutic areas including dermatology, ophthalmology, our breast cancer portfolio, some newly launched brands and the Sandoz retail and anti-infectives business, and on drug development operations; or regarding potential future, pending or announced transactions; regarding potential future sales or earnings of the Group or any of its divisions; or by discussions of strategy, plans, expectations or intentions; or regarding the Group’s liquidity or cash flow positions and its ability to meet its ongoing financial obligations and operational needs; or regarding our collaboration with Molecular Partners to develop, manufacture and commercialize potential medicines for the prevention and treatment of COVID- 19 and our joining of the industry-wide efforts to meet global demand for COVID-19 vaccines and therapeutics by leveraging our manufacturing capacity and capabilities to support the production of the Pfizer-BioNTech vaccine and to manufacture the mRNA and bulk drug product for the vaccine candidate CVnCoV from CureVac. -

The CCR5-Delta32 Variant Might Explain Part of the Association Between COVID-19 and the Chemokine-Receptor Gene Cluster
medRxiv preprint doi: https://doi.org/10.1101/2020.11.02.20224659; this version posted November 4, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. All rights reserved. No reuse allowed without permission. The CCR5-delta32 variant might explain part of the association between COVID-19 and the chemokine-receptor gene cluster 1,8,12* 1,8* 2,8,9,10,11 Juan Gómez, Elías Cuesta-Llavona, Guillermo M. Albaiceta, Marta 3 4,8,9,12 2,8,10,11 García-Clemente, Carlos López-Larrea, Laura Amado-Rodríguez, Inés 8,10 3 3 1,8 1,8 López-Alonso, Tamara Hermida, Ana I. EnrÍquez, Helena Gil , Belén Alonso, 1,8 1 1,8,9,12 Sara Iglesias, Beatriz Suarez-Alvarez,4,8,12 Victoria Alvarez, Eliecer Coto *These authors contributed equally to this work. 1 Genética Molecular, Hospital Universitario Central Asturias, Oviedo, Spain. 2 Unidad de Cuidados Intensivos Cardiológicos, Hospital Universitario Central Asturias, Oviedo, Spain. 3 Neumología, Hospital Universitario Central Asturias, Oviedo, Spain. 4 Inmunología, Hospital Universitario Central Asturias, Oviedo, Spain. 5 Urgencias, Hospital Universitario Central Asturias, Oviedo, Spain. 8 Instituto de Investigación Sanitaria del Principado deAsturias, ISPA, Oviedo, Spain. 9 Universidad de Oviedo, Oviedo, Spain. 10 CIBER-Enfermedades Respiratorias. Instituto de Salud Carlos III. Madrid, Spain. 11 Instituto Universitario de Oncología del Principado de Asturias. Oviedo, Spain. 12 Red de Investigación Renal (REDINREN), Madrid, Spain. Correspondenceto: Dr.EliecerCoto Hospital Univ. Central Asturias 33011 – Oviedo – Spain Tel. 34.985.10.55.00 Email: [email protected] 1 NOTE: This preprint reports new research that has not been certified by peer review and should not be used to guide clinical practice.