Neurologic Urinary and Faecal Incontinence
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Fecal Incontinence/Anal Incontinence
Fecal Incontinence/Anal Incontinence What are Fecal incontinence/ Anal Incontinence? Fecal incontinence is inability to control solid or liquid stool. Anal incontinence is the inability to control gas and mucous in addition to the inability to control stool. The symptoms range from mild release of gas to a complete loss of control. It is a common problem affecting 1 out of 13 women under the age of 60 and 1 out of 7 women over the age of 60. Men can also be have this condition. Anal incontinence is a distressing condition that can interfere with the ability to work, do daily activities and enjoy social events. Even though anal incontinence is a common condition, people are uncomfortable discussing this problem with family, friends, or doctors. They often suffer in silence, not knowing that help is available. Normal anatomy The anal sphincters and puborectalis are the primary muscles responsible for continence. There are two sphincters: the internal anal sphincter, and the external anal sphincter. The internal sphincter is responsible for 85% of the resting muscle tone and is involuntary. This means, that you do not have control over this muscle. The external sphincter is responsible for 15% of your muscle tone and is voluntary, meaning you have control over it. Squeezing the puborectalis muscle and external anal sphincter together closes the anal canal. Squeezing these muscles can help prevent leakage. Puborectalis Muscle Internal Sphincter External Sphincter Michigan Bowel Control Program - 1 - Causes There are many causes of anal incontinence. They include: Injury or weakness of the sphincter muscles. Injury or weakening of one of both of the sphincter muscles is the most common cause of anal incontinence. -

Coating Composition, Coating Film, and Process for the Production of the Film
s\ — Mil II II II II II II I II I II III II Ml OJII Eur°Pean Patent Office <*S Office europeen des brevets (11) EP 0 909 800 A1 (12) EUROPEAN PATENT APPLICATION published in accordance with Art. 158(3) EPC (43) Date of publication: (51) Int. CI.6: C09D 1 27/1 2, C08L 27/12, 21.04.1999 Bulletin 1999/16 C08K 3/22 (21) Application number: 97926258.1 v ' ^ (86)/0~x International application number:u PCT/JP97/02070 (22) Date of filing: 16.06.1997 (87) International publication number: WO 97/48774 (24.12.1997 Gazette 1997/55) (84) Designated Contracting States: • KUMEGAWA, Masahiro, DE FR GB IT Yodogawa-seisakusho Settsu-shi, Osaka 566 (JP) (30) Priority: 19.06.1996 JP 157978/96 • OKA, Noritoshi, Yodogawa-seisakusho (71) Applicant: Settsu-shi, Osaka 566 (JP) DAI KIN INDUSTRIES, LIMITED . SHIMIZU, TetSUO, Osaka-shi, Osaka-fu 530 (JP) Yodogawa-seisakusho Settsu-shi, Osaka 566 (JP) (72) Inventors: • ARAKI, Takayuki, (74) Representative: HOFFMANN - EITLE Yodogawa-seisakusho Patent- und Rechtsanwalte Settsu-shi, Osaka6566 (JP) Arabellastrasse 4 • TANAKA, Yoshito, 81925 Munchen (DE) Yodogawa-seisakusho Settsu-shi, Osaka 566 (JP) (54) COATING COMPOSITION, COATING FILM, AND PROCESS FOR THE PRODUCTION OF THE FILM (57) To provide the water-repellent coating film hav- ing excellent transparency, abrasion resistance, weather resistance and water repellency, the method for producing the coating film, the multi-functional compos- ite material provided with the coating film and the coat- ing composition used therefor which has excellent dispersion stability. The coating composition comprises (A) the fluorine-containing ethylenic polymer prepared by copolymerizing a fluorine-containing ethylenic mono- mer having at least one functional group selected from hydroxyl, carboxyl, a carboxylic salt group, a carboxylic ester group and epoxy, (B-1) the metal oxide sol, and (C) the solvent. -

Utility of the Digital Rectal Examination in the Emergency Department: a Review
The Journal of Emergency Medicine, Vol. 43, No. 6, pp. 1196–1204, 2012 Published by Elsevier Inc. Printed in the USA 0736-4679/$ - see front matter http://dx.doi.org/10.1016/j.jemermed.2012.06.015 Clinical Reviews UTILITY OF THE DIGITAL RECTAL EXAMINATION IN THE EMERGENCY DEPARTMENT: A REVIEW Chad Kessler, MD, MHPE*† and Stephen J. Bauer, MD† *Department of Emergency Medicine, Jesse Brown VA Medical Center and †University of Illinois-Chicago College of Medicine, Chicago, Illinois Reprint Address: Chad Kessler, MD, MHPE, Department of Emergency Medicine, Jesse Brown Veterans Hospital, 820 S Damen Ave., M/C 111, Chicago, IL 60612 , Abstract—Background: The digital rectal examination abdominal pain and acute appendicitis. Stool obtained by (DRE) has been reflexively performed to evaluate common DRE doesn’t seem to increase the false-positive rate of chief complaints in the Emergency Department without FOBTs, and the DRE correlated moderately well with anal knowing its true utility in diagnosis. Objective: Medical lit- manometric measurements in determining anal sphincter erature databases were searched for the most relevant arti- tone. Published by Elsevier Inc. cles pertaining to: the utility of the DRE in evaluating abdominal pain and acute appendicitis, the false-positive , Keywords—digital rectal; utility; review; Emergency rate of fecal occult blood tests (FOBT) from stool obtained Department; evidence-based medicine by DRE or spontaneous passage, and the correlation be- tween DRE and anal manometry in determining anal tone. Discussion: Sixteen articles met our inclusion criteria; there INTRODUCTION were two for abdominal pain, five for appendicitis, six for anal tone, and three for fecal occult blood. -
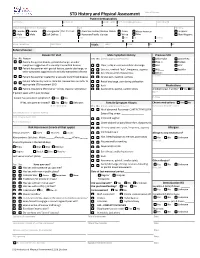
STD History and Physical Assessment Date of Service: Patient Demographics Last Name First Name Middle Initial Pref
STD History and Physical Assessment Date of Service: Patient Demographics Last Name First Name Middle Initial Pref. name/AKA/pronoun Date of Birth Sex (at birth) Gender (all that apply Race Ethnicity Female Female Transgender Pref. Pronoun: American Indian/Alaskan Native Asian African American Hispanic Male Male Self Define: Hawaiian/Pacific Islander White Other Non-Hispanic Street Address City State Zip County Home Telephone Cell Phone Vitals: Temp: Pulse: RR: BP: Referral Source: Reason for Visit Male Symptom History Previous STD Yes No Reason Yes No (check appropriate boxes) Chlamydia Gonorrhea Patient has genital lesions, genital discharge, or other Hep. C Herpes symptoms suggestive of a sexually transmitted disease Clear, milky or mucoid urethral discharge HIV HPV Patient has partner with genital lesions, genital discharge, or Dysuria , urethral “itch”, frequency, urgency PID Syphilis other symptoms suggestive of a sexually transmitted disease Sore throat and/or hoarseness Other: Patient has partner treated for a sexually transmitted disease Scrotal pain, swelling, redness Comments: Patient referred by local or state DIS. Review labs and refer to Rectal discharge, pain during defecation appropriate STD treatment SDO Rash Medications Patient requesting STD testing – denies reasons listed above Asymmetric, painful, swollen joints Antibiotics last 4 weeks? Yes No If patient seen within past 30 days: Name Purpose Patient has persistent symptoms? Yes No If Yes, was partner treated? Yes No Unknown Female Symptom History Chronic medications -

Autonomic Nervous System Dysfunction Involving the Gastrointestinal and the Urinary Tracts in Primary Sjögren’S Syndrome
Autonomic nervous system dysfunction involving the gastrointestinal and the urinary tracts in primary Sjögren’s syndrome L. Kovács1, M. Papós2, R. Takács3, R. Róka2, Z. Csenke4, A. Kovács1, T. Várkonyi3, L. Pajor5, L. Pávics2, G. Pokorny1 Department of Rheumatology1, Department of Nuclear Medicine2, 1st Department of Internal Medicine3 and Department of Urology5, University of Szeged, Faculty of Medicine, Szeged; Division of Urology, Municipial Clinic, Szeged, Hungary4 Abstract Objective Antibodies reacting with the m3 subtype muscarinic acetylcholine receptor appear to be an important patho- genic factor in primary Sjögren’s syndrome (pSS). As this receptor subtype is functionally important in the gastrointestinal and urinary tracts, and very little is known about the autonomic nervous system function in these organs in pSS patients, the occurrence and clinical significance of an autonomic nervous system dysfunction involving the gastrointestinal and urinary tracts were investigated. Methods Data on clinical symptoms attributable to an autonomic dysfunction were collected from 51 pSS patients. Gastric emptying scintigraphy and urodynamic studies were performed on 30 and 16 patients, respectively, and the results were correlated with patient characteristics and with the presence of autonomic nervous system symptoms. Results Gastric emptying was abnormally slow in 21 of the 30 examined patients (70%). Urodynamic findings compatible with a decreased detrusor muscle tone or contractility were found in 9 of the 16 patients tested (56%). Various symptoms of an autonomic nervous system dysfunction were reported by 2-16% of the patients. Conclusion Signs of an autonomic nervous system dysfunction involving the gastrointestinal and the urinary systems can be observed in the majority of pSS patients. -

Regions Hospital Delineation of Privileges Surgery
Regions Hospital Delineation of Privileges Surgery Applicant’s Name: ____________________________________________________________________________ Last First M. Instructions: Place a check-mark where indicated for each core group you are requesting. Review education and basic formal training requirements to make sure you meet them. Review documentation and experience requirements and be prepared to prove them. Note all renewing applicants are required to provide evidence of their current ability to perform the privileges being requested\ When documentation of cases or procedures is required, attach said case/procedure logs to this privileges-request form. Provide complete and accurate names and addresses where requested -- it will greatly assist how quickly our credentialing-specialist can process your requests. Overview: (Applicant should check all core privileges you are requesting) Core I – General Staff Privileges in Surgery Core II – General Staff Privileges in Trauma (Adult and Pediatric) Core III – Pediatric Trauma Rounding Privileges Core IV – General Staff Privileges in Burn Core V – General Staff Privileges in Colon and Rectal Surgery Core VI – General Staff Privileges in Vascular Surgery Core VII – General Staff Privileges in Surgical Critical Care Special Privileges Also included are: Core Procedure Lists Signature Page Page 1 of 24 06.2015 CORE I -- General Staff Privileges in Surgery (Appointments are based on the needs of the Department of Surgery as determined by the Division Head of Surgery and Hospital Board) Privileges Privileges include the performance of surgical procedures (including related admission, consultation, work-up, pre- and post-operative care) to correct or treat various conditions, illnesses and injuries of the: alimentary tract, including colon and rectum, abdomen and its contents, breasts, skin, and soft tissue, head and neck, endocrine system and vascular system, excluding the intercranial vessels, the heart and those vessels intrinsic and immediately adjacent thereto. -

The Practice of Gastrointestinal Motility Laboratory During COVID-19 Pandemic
J Neurogastroenterol Motil, Vol. 26 No. 3 July, 2020 pISSN: 2093-0879 eISSN: 2093-0887 https://doi.org/10.5056/jnm20107 JNM Journal of Neurogastroenterology and Motility Review The Practice of Gastrointestinal Motility Laboratory During COVID-19 Pandemic: Position Statements of the Asian Neurogastroenterology and Motility Association (ANMA-GML-COVID-19 Position Statements) Kewin T H Siah,1,2* M Masudur Rahman,3 Andrew M L Ong,4,5 Alex Y S Soh,1,2 Yeong Yeh Lee,6,7 Yinglian Xiao,8 Sanjeev Sachdeva,9 Kee Wook Jung,10 Yen-Po Wang,11 Tadayuki Oshima,12 Tanisa Patcharatrakul,13,14 Ping-Huei Tseng,15 Omesh Goyal,16 Junxiong Pang,17 Christopher K C Lai,18 Jung Ho Park,19 Sanjiv Mahadeva,20 Yu Kyung Cho,21 Justin C Y Wu,22 Uday C Ghoshal,23 and Hiroto Miwa12 1Department of Medicine, Yong Loo Lin School of Medicine, The National University of Singapore, Singapore; 2Division of Gastroenterology and Hepatology, Department of Medicine, National University Hospital, Singapore; 3Department of Gastroenterology, Sheikh Russel National Gastroliver Institute and Hospital, Dhaka, Bangladesh; 4Department of Gastroenterology and Hepatology, Singapore General Hospital, Singapore; 5Duke-NUS Medical School, Singapore; 6School of Medical Sciences, Universiti Sains Malaysia, Malaysia; 7St George and Sutherland Clinical School, University of New South Wales, Kogarah, NSW, Australia; 8Department of Gastroenterology and Hepatology, First Affiliated Hospital, Sun Yat-sen University, Guangzhou, China; 9Department of Gastroenterology, GB Pant Hospital, New Delhi, India; -

Diagnostic Approach to Chronic Constipation in Adults NAMIRAH JAMSHED, MD; ZONE-EN LEE, MD; and KEVIN W
Diagnostic Approach to Chronic Constipation in Adults NAMIRAH JAMSHED, MD; ZONE-EN LEE, MD; and KEVIN W. OLDEN, MD Washington Hospital Center, Washington, District of Columbia Constipation is traditionally defined as three or fewer bowel movements per week. Risk factors for constipation include female sex, older age, inactivity, low caloric intake, low-fiber diet, low income, low educational level, and taking a large number of medications. Chronic constipa- tion is classified as functional (primary) or secondary. Functional constipation can be divided into normal transit, slow transit, or outlet constipation. Possible causes of secondary chronic constipation include medication use, as well as medical conditions, such as hypothyroidism or irritable bowel syndrome. Frail older patients may present with nonspecific symptoms of constipation, such as delirium, anorexia, and functional decline. The evaluation of constipa- tion includes a history and physical examination to rule out alarm signs and symptoms. These include evidence of bleeding, unintended weight loss, iron deficiency anemia, acute onset constipation in older patients, and rectal prolapse. Patients with one or more alarm signs or symptoms require prompt evaluation. Referral to a subspecialist for additional evaluation and diagnostic testing may be warranted. (Am Fam Physician. 2011;84(3):299-306. Copyright © 2011 American Academy of Family Physicians.) ▲ Patient information: onstipation is one of the most of 1,028 young adults, 52 percent defined A patient education common chronic gastrointes- constipation as straining, 44 percent as hard handout on constipation is 1,2 available at http://family tinal disorders in adults. In a stools, 32 percent as infrequent stools, and doctor.org/037.xml. -

Chapter Four – TRPA1 Channels: Chemical and Temperature Sensitivity
CHAPTER FOUR TRPA1 Channels: Chemical and Temperature Sensitivity Willem J. Laursen1,2, Sviatoslav N. Bagriantsev1,* and Elena O. Gracheva1,2,* 1Department of Cellular and Molecular Physiology, Yale University School of Medicine, New Haven, CT, USA 2Program in Cellular Neuroscience, Neurodegeneration and Repair, Yale University School of Medicine, New Haven, CT, USA *Corresponding author: E-mail: [email protected], [email protected] Contents 1. Introduction 90 2. Activation and Regulation of TRPA1 by Chemical Compounds 91 2.1 Chemical activation of TRPA1 by covalent modification 91 2.2 Noncovalent activation of TRPA1 97 2.3 Receptor-operated activation of TRPA1 99 3. Temperature Sensitivity of TRPA1 101 3.1 TRPA1 in mammals 101 3.2 TRPA1 in insects and worms 103 3.3 TRPA1 in fish, birds, reptiles, and amphibians 103 3.4 TRPA1: Molecular mechanism of temperature sensitivity 104 Acknowledgments 107 References 107 Abstract Transient receptor potential ankyrin 1 (TRPA1) is a polymodal excitatory ion channel found in sensory neurons of different organisms, ranging from worms to humans. Since its discovery as an uncharacterized transmembrane protein in human fibroblasts, TRPA1 has become one of the most intensively studied ion channels. Its function has been linked to regulation of heat and cold perception, mechanosensitivity, hearing, inflam- mation, pain, circadian rhythms, chemoreception, and other processes. Some of these proposed functions remain controversial, while others have gathered considerable experimental support. A truly polymodal ion channel, TRPA1 is activated by various stimuli, including electrophilic chemicals, oxygen, temperature, and mechanical force, yet the molecular mechanism of TRPA1 gating remains obscure. In this review, we discuss recent advances in the understanding of TRPA1 physiology, pharmacology, and molecular function. -

The Emerging Role of Transient Receptor Potential Channels in Chronic Lung Disease
BACK TO BASICS | TRANSIENT RECEPTOR POTENTIAL CHANNELS IN CHRONIC LUNG DISEASE The emerging role of transient receptor potential channels in chronic lung disease Maria G. Belvisi and Mark A. Birrell Affiliation: Respiratory Pharmacology Group, Airway Disease Section, National Heart and Lung Institute, Imperial College, London, UK. Correspondence: Maria G. Belvisi, Respiratory Pharmacology Group, Airway Disease Section, National Heart and Lung Institute, Imperial College, Exhibition Road, London SW7 2AZ, UK. E-mail: [email protected] @ERSpublications Transient receptor potential channels are emerging as novel targets for chronic lung diseases with a high unmet need http://ow.ly/GHeR30b3hIy Cite this article as: Belvisi MG, Birrell MA. The emerging role of transient receptor potential channels in chronic lung disease. Eur Respir J 2017; 50: 1601357 [https://doi.org/10.1183/13993003.01357-2016]. ABSTRACT Chronic lung diseases such as asthma, chronic obstructive pulmonary disease and idiopathic pulmonary fibrosis are a major and increasing global health burden with a high unmet need. Drug discovery efforts in this area have been largely disappointing and so new therapeutic targets are needed. Transient receptor potential ion channels are emerging as possible therapeutic targets, given their widespread expression in the lung, their role in the modulation of inflammatory and structural changes and in the production of respiratory symptoms, such as bronchospasm and cough, seen in chronic lung disease. Received: Jan 08 2017 | Accepted after revision: April 14 2017 Conflict of interest: Disclosures can be found alongside this article at erj.ersjournals.com Copyright ©ERS 2017 https://doi.org/10.1183/13993003.01357-2016 Eur Respir J 2017; 50: 1601357 TRANSIENT RECEPTOR POTENTIAL CHANNELS IN CHRONIC LUNG DISEASE | M.G. -

Peripheral Neuropathy Diagnostic Services
Peripheral Neuropathy Diagnostic Services Approximately 1 out of every 15 people (20 million) suffer from Neuropathy and more than 30% of all Neuropathies stem from Diabetes. Digirad provides Peripheral Neuropathy diagnostic services to healthcare providers that treat patients who are at risk from autonomic dysfunction or autonomic neuropathy. Adding these services is convenient for your patients and provides a new revenue stream for your practice. Program Overview The Peripheral Neuropathy Diagnostics service is performed by our technologist in a standard patient exam room. The patient’s peripheral nervous system is monitored and evaluated for its response to stimulation. The test is relatively quick, pain free and patient satisfaction is very high. After the test is performed, a detailed set of results and analysis are delivered back to you. The results provide a clear understanding of the presence, and extent of, peripheral autonomic dysfunction or disease. Additional studies may be performed to identify the cause of symptoms such as numbness, tingling, continuous pain and the early detection of diabetes complications. How it Works • The program is overseen by highly qualified Neurologists • One of our highly trained technologists will arrive on your scheduled date to perform testing • We provide the state-of-the-art equipment and tests are done in one of your exam rooms • Reports are delivered within 24-48 hours using Digirad’s digital delivery system • This system permanently stores patients’ test results allowing you unlimited access Contact us to learn more: 855-644-3443 | www.digirad.com Digirad delivers diagnostic imaging expertise. As Needed. When Needed. Where Needed. Autonomic Neuropathy Autonomic neuropathy is a disorder that affects involuntary body functions, including heart rate, blood pressure, perspiration and digestion. -

Complications of Urinary Diversion
Complications of Urinary Diversion Jennifer L. Dodson, M.D. Department of Urology Johns Hopkins University Types of Diversion Conduit Diversions Ileal conduit Colon conduit Continent Diversions Continent catheterizable reservoir Continent rectal pouch 1 Overview of Complications Mechanical Stoma problems Bowel obstruction Ureteral obstruction Reservoir perforation Metabolic Altered absorption Altered bone metabolism Growth delay Stones Cancer Conduit Diversions Ileal Conduit: Technically simplest Segment of choice Colon Conduit: Transverse or sigmoid Used when ileum not appropriate (eg: concomitant colon resection, abdominal radiation, short bowel syndrome, IBD) Early complications (< 30 days): 20-56% Late complications : 28-81% Risks: abdominal radiation abdominal surgery poor nutrition chronic steroids Farnham & Cookson, World J Urol, 2004 2 Complications of Ileal Conduit Campbell’s Urology, 8th Edition, 2002 Conduit: Bowel Complications Paralytic ileus 18-20% Conservative management vs NGT Consider TPN Bowel obstruction 5-10% Causes: Adhesions, internal hernia Evaluation: CT scan, Upper GI series Anastomotic leak 1-5 % Risk factors: bowel ischemia, radiation, steroids, IBD, technical error Prevention: Pre-operative bowel prep Attention to technical detail Stapled small-bowel Anastomosis (Campbell’s Blood supply, tension-free anastomosis, Urology, 8th Ed, 2004) realignment of mesentery Farnham & Cookson, World J Urol, 2004 3 Conduit Complications Conduit necrosis: Acute ischemia to bowel