Postgraduate Psychiatry Elective Description
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
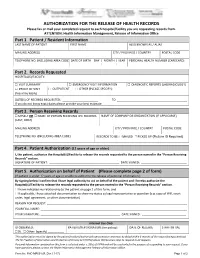
AUTHORIZATION for the RELEASE of HEALTH RECORDS Please Fax Or Mail Your Completed Request to Each Hospital/Facility You Are Requesting Records From
AUTHORIZATION FOR THE RELEASE OF HEALTH RECORDS Please fax or mail your completed request to each hospital/facility you are requesting records from. ATTENTION: Health Information Management, Release of Information Office Part 1. Patient / Resident Information LAST NAME OF PATIENT FIRST NAME ALSO KNOWN AS / ALIAS MAILING ADDRESS CITY / PROVINCE / COUNTRY POSTAL CODE TELEPHONE NO. (INCLUDING AREA CODE) DATE OF BIRTH DAY | MONTH | YEAR PERSONAL HEALTH NUMBER (CARECARD) | | Part 2. Records Requested HOSPITAL(S)/FACILITY: □ VISIT SUMMARY □ EMERGENCY VISIT INFORMATION □ DIAGNOSTIC REPORTS (LAB/RADIOLOGY) □ PROOF OF VISIT □ OUTPATIENT □ OTHER (PLEASE SPECIFY): (fees may apply) DATE(S) OF RECORDS REQUESTED: ______________________ TO ___________________________________________ If you do not know exact dates please provide your best estimate Part 3. Person Receiving Records □ MYSELF OR □ NAME OF PERSON RECEIVING THE RECORDS NAME OF COMPANY OR ORGANIZATION (IF APPLICABLE) (LAST, FIRST) MAILING ADDRESS CITY / PROVINCE / COUNTRY POSTAL CODE TELEPHONE NO. (INCLUDING AREA CODE) RECORDS TO BE: □ MAILED □ PICKED UP (Picture ID Required) Part 4. Patient Authorization (12 years of age or older) I, the patient, authorize the Hospital(s)/Facility to release the records requested to the person named in the “Person Receiving Records” section. SIGNATURE OF PATIENT: ___________________________________________ DATE SIGNED: ____________________________ Part 5. Authorization on behalf of Patient (Please complete page 2 of form) (If patient is under 12 years of age or unable to authorize the release of personal information.) By signing below I confirm that I have legal authority to act on behalf of the patient and I hereby authorize the Hospital(s)/Facility to release the records requested to the person named in the “Person Receiving Records” section. -

UBC Department of Medicine CME Event: Medicine in the 21St Century – June 5, 2008 2
THE UNIVERSITY OF BRITISH COLUMBIA S192- 2211 Wesbrook Mall Vancouver, BC, V6T2B5 Curriculum Vitae for Faculty Members Date completed: June 8, 2013 1. SURNAME: FELDMAN FIRST NAME: HOWARD MIDDLE NAME(S): 2. DEPARTMENT/SCHOOL: Medicine 3. FACULTY: Medicine 4. PRESENT RANK: Full Professor SINCE: July 1, 2001 5. POST-SECONDARY EDUCATION University or Institution Degree Subject Area Dates McGill University DCS Arts 1971-1973 McGill University MDCM Medicine 1974-1978 University of British Columbia FRCP(C) Neurology 1984-1986 PROFESSIONAL QUALIFICATIONS Internship - University of Western Ontario 1978-9 Victoria Hospital - London, Ontario Residency Training Internal Medicine - McGill University 1981-83 Royal Victoria Hospital - Montreal, Quebec Neurology - University of Colorado 1983-84 Neurology - University of British Columbia 1984-86 Fellowship Training Amyotrophic lateral sclerosis and Neuromuscular Diseases -1986 University of British Columbia Supervisor – Dr. A.A. Eisen Fellowships Awarded Fellow of the Royal College of Physicians and Surgeons of Canada FRCP (Neurology) 1986 Fellow of the Canadian Academy of Health Sciences FCAHS (2008 – present) Fellow of the American Academy of Neurology FAAN (2008 – present) 1 6. EMPLOYMENT RECORD (a) At UBC RANK OR TITLE Dates Executive Associate Dean, Research January 2012- present UBC Faculty of Medicine Full Professor 2001-present UBC Division of Neurology Head 2001- 2008 UBC Division of Neurology Ralph Fisher and Alzheimer Society of B.C. 2007 – 2008, 2012- present Endowed Professor in Alzheimer -

Carms 2021 Information Package TABLE of CONTENTS
THE UNIVERSITY OF BRITISH COLUMBIA DEPARTMENT OF PSYCHIATRY CaRMS 2021 Information Package TABLE OF CONTENTS 03 Welcome Messages 05 Program Overview 06 Clinical Curriculum 13 Psychotherapy Curriculum 14 Academic Curriculum 15 Opportunities Unique to UBC 16 Outreach and Rural Practice Opportunities 17 Fellowship & Subspecialty Training 18 CaRMS Interview Day QUESTIONS ABOUT INTERVIEW SCHEDULE? CONTACT: Linda Chang Education Coordinator, PGE [email protected] Welcome Message from Dr. Khanbhai Irfan Khanbhai Interim Program Director [email protected] Dear CaRMS Applicant, I am excited that you have chosen UBC Psychiatry for an interview. I look forward to meeting you during the interview period as I meet with all applicants individually. UBC Psychiatry offers a dynamic and comprehensive program. Depending on what track you have applied to, I encourage you to read the information outlined in the document. I am from North Vancouver, received my BSc from McGill, completed medical school at UBC, and thereafter, began my training in Psychiatry at UBC. Given that I have trained here, I can say first hand that we offer an incredible program with respect to clinical experience and resident education. I have been involved in resident education since my residency training and feel privileged to be able to lead this program. Please feel free to email me at [email protected]. Sincerely, Irfan Khanbhai Interim Program Director University of British Columbia Postgraduate Education Psychiatry 3 Message from our CaRMS Committee Dear CaRMS Applicant, We would like to welcome you (virtually!) to the University of British Columbia! Our program offers a diverse array of exceptional training in all core competencies outlined by the Royal College of Physicians and Surgeons of Canada. -

Bc Simulation Current State Report
Provincial Simulation Coordination Committee Current State Report BC SIMULATION CURRENT STATE REPORT Prepared by: BC Provincial Simulation Coordination Committee Delivered to: BC Ministry of Advanced Education, Innovation, and Technology BC Ministry of Health November 29, 2013 November 19, 2013 Page 0 of 35 Provincial Simulation Coordination Committee Current State Report 1 Executive Summary The Provincial Simulation Coordination Committee (PSCC) was established in June 2012 and functions as a central coordinating and advisory organization. The PSCC’s goal is to support health authorities and health professional education institutions province wide to advance the efficient development of simulation education through an integrated approach that improves access to simulation facilities, technologies, and resources. In early 2013, the PSCC received funding to develop a Simulation Roadmap for BC. The first deliverable in this roadmap is a Current State Report that aims to enable the BC Government to make effective, contextual decisions on where to allocate taxpayer funds based on an improved understanding of the current simulation environment. A PSCC Sub-Committee was established to lead the development of the Current State Report and included representatives from UBC, BCIT, and Northern Health Authority. The Sub-Committee developed a list of online survey questions for stakeholders identified by the PSCC across the Province according to regional, professional, and institutional affiliation. Approximately 80 individuals were invited to complete the survey on May 27, 2013 and 56 completed responses were received by the survey close on July 5, 2013 for a 70% completion rate. Key findings from the survey were grouped into three categories: 1. Equipment and Technology 2. -

Annual Report 2015 | 2016 TABLE of CONTENTS OVERVIEW of the DEPARTMENT of MEDICINE Heads and Directors
UNIVERSITY OF BRITISH COLUMBIA DEPARTMENT OF MEDICINE Annual Report 2015 | 2016 TABLE OF CONTENTS OVERVIEW OF THE DEPARTMENT OF MEDICINE Heads and Directors.................................................................... 2 Committees................................................................................... 3 Administration.............................................................................. 11 RESEARCH Activities....................................................................................... 12 Research Metrics and Highlights............................................ 12 EDUCATION UNIVERSITY OF BRITISH COLUMBIA Accomplishments and Highlights........................................... 13 DEPARTMENT OF MEDICINE Undergraduate Medical Education Program (UGME)....... 13 Annual Report 2015 | 2016 Postgraduate Medical Education Program (PGME)........... 13 Experimental Medicine.............................................................. 16 Dr. Graydon S. Meneilly, MD, FRCPC, MACP DIVISION REPORTS Professor and Eric W. Hamber Chair AIDS................................................................................................ 17 Head, UBC Department of Medicine Allergy and Immunology.......................................................... 20 Physician-in-Chief & Head, Cardiology.................................................................................... 22 Community Internal Medicine................................................ 25 Department of Medicine Critical Care Medicine.............................................................. -

Paracentesis Jim Pattison Outpatient Care 604-533-3308 You Can Ask Questions About the Risks and Surgery Centre Ext 63926 Before You Sign the Consent Form
Are there any risks or complications? Locations Abbotsford-Regional Hospital 604-851-4866 Any time the skin is pierced or cut, there Medical Imaging 2nd Floor, Fraser Wing, 32900 Marshall Road, Abbotsford is a chance of infection. Other possible BC Cancer Agency 604-877-6000 complications include: Medical Imaging, 3rd Floor, 600 West 10th Ave, Vancouver - bleeding Burnaby Hospital 604-434-4211 Medical Imaging, 3rd Floor, 3935 Kincaid St., Burnaby - infection of the lining of the abdominal Chilliwack General Hospital 604-795-4122 wall (called peritonitis) Medical Imaging, Main Floor, 45600 Menholm Rd, Chilliwack Paracentesis Jim Pattison Outpatient Care 604-533-3308 You can ask questions about the risks and Surgery Centre Ext 63926 before you sign the consent form. Medical Imaging, 2nd Floor, 9750 140th Street, Surrey Langley Memorial Hospital 604-533-6405 Medical Imaging, Main Floor, 22051 Fraser Highway, Langley When will I get the results? Lions Gate Hospital 604-984-5775 Medical Imaging, Lower Level, 231 East 15th Street, North Vancouver If we collect samples of the fluid, the Peace Arch Hospital 604-531-5512 results are sent to your doctor’s office Medical Imaging, Main Floor, 15521 Russell Ave, White Rock within 2 weeks. Make an appointment Powell River General Hospital 604-485-3282 Medical Imaging, 5000 Joyce Avenue, Powell River with your doctor to review the results. Richmond Hospital 604-278-9711 Medical Imaging, Main Floor, 7000 Westminster Hwy, Richmond When to get help Ridge Meadows Hospital 604-463-1800 Medical Imaging, Main Floor, 11666 Laity Street, Maple Ridge Call your doctor if you have any of the Royal Columbian Hospital 604-520-4640 following: Medical Imaging, Columbia Tower 330 E. -

Ultrasound Guided Thyroid Biopsy Over…
When to get help Locations Abbotsford-Regional Hospital 604-851-4866 Call your doctor if you have any of the Medical Imaging 2nd Floor, Fraser Wing following: 32900 Marshall Road, Abbotsford BC Cancer Agency 604-877-6000 rd Fever above 38.5°C (101°F), aches, and Medical Imaging, 3 Floor chills 600 West 10th Ave, Vancouver Burnaby Hospital 604-434-4211 Increased pain or any redness at or Medical Imaging, 3rd Floor around the biopsy site 3935 Kincaid St., Burnaby Ultrasound Chilliwack General Hospital 604-795-4122 Medical Imaging, Main Floor Go to the nearest Emergency 45600 Menholm Rd, Chilliwack Guided Thyroid Department if you have any of the Delta Hospital 604-946-1121 following: Medical Imaging, 5800 Mountain View Boulevard, Delta Biopsy Jim Pattison Outpatient Care 604-533-3308 Swelling of the neck and Surgery Centre ext. 63926 Medical Imaging, 2nd Floor Severe weakness 9750 140th Street, Surrey Lions Gate Hospital 604-984-5775 Trouble breathing Medical Imaging, Lower Level th Trouble swallowing 231 East 15 Street, North Vancouver Peace Arch Hospital 604-531-5512 Medical Imaging, Main Floor 15521 Russell Ave, White Rock Richmond Hospital 604-278-9711 Medical Imaging, Main Floor 7000 Westminster Hwy, Richmond Ridge Meadows Hospital 604-463-1800 Medical Imaging, Main Floor 11666 Laity Street, Maple Ridge St. Paul’s Hospital 604-806-8006 Medical Imaging, 2nd Floor, Providence Building 1081 Burrard Street, Vancouver Surrey Memorial Hospital 604-588-3308 st Medical Imaging, 1 Floor, Lower Level th 13750 96 Avenue, Surrey HealthLinkBC 8-1-1 UBC Hospital 604-822-7076 Medical Imaging, Main Floor Call any time you have any questions or concerns. -

Please Fax Or Mail Your Request to Each Hospital/Facility You Are Requesting Records from Attention: Health Information Management, Release of Information Office
PLEASE FAX OR MAIL YOUR REQUEST TO EACH HOSPITAL/FACILITY YOU ARE REQUESTING RECORDS FROM ATTENTION: HEALTH INFORMATION MANAGEMENT, RELEASE OF INFORMATION OFFICE Abbotsford Regional Hospital Forensic Psychiatric Hospital 32900 Marshall Rd, Abbotsford, BC V2S 0C2 70 Colony Farm Rd, Coquitlam, BC V3C 5X9 Fax: (604) 851‐4902 Tel: (604) 851‐4700, Ext 646790 Fax: (604) 523‐7897 Tel: (604) 524‐7732 BC Children’s Hospital and BC Women’s Hospital Fraser Canyon Hospital 4500 Oak St, Vancouver, BC V6H 3V5 1275 7 Ave, Hope, BC V0X 1L4 Fax: (604) 875‐2662 Tel: (604) 875‐3450 Fax: (604) 860‐7710 Tel: (604) 860‐7729 BCCA – Abbotsford GF Strong Rehab Centre 32900 Marshall Rd, Abbotsford, BC V2S 0C2 4255 Laurel St, Vancouver, BC V5Z 2G9 Fax: (604) 851‐4738 Tel: (604) 851‐4710, Ext 645176 Fax: (604) 731‐5091 Tel: (604) 714‐4158 BCCA – Fraser Valley Holy Family Hospital (c/o St. Paul’s Hospital) 13750 96 Ave, Surrey, BC V3V 1Z2 1081 Burrard St, Vancouver, BC V6Z 1Y6 Fax: (604) 930‐4096 Tel: (604) 930‐4073 Fax: (604) 806‐9015 Tel: (604) 806‐8099 BCCA – Kelowna Langley Memorial Hospital 399 Royal Ave, Kelowna, BC V1Y 5L3 22051 Fraser Hwy, Langley, BC V3A 4H4 Fax: (250) 712‐3977 Tel: (250) 712‐3900 Fax: (604) 533‐6458 Tel: (604) 534‐4121, Ext 745272 If your last name starts with A‐L, Ext 686822 If your last name starts with M‐Z, Ext 686814 Lion’s Gate Hospital 231 E. 15th St, North Vancouver, BC V7L 2L7 BCCA – Prince George Fax: (604)984‐5718 Tel: (604) 984‐5719 1215 Lethbridge St, Prince George, BC V2M 7E9 Fax: (250) 645‐7366 Tel: (250) 645‐7316 Mission Memorial Hospital 7324 Hurd St, Mission, BC V2V 3H5 BCCA – Vancouver Fax: (604) 826‐4043 Tel: (604) 814‐5166 600 W. -

Guidebook-For-Patients-Surrey.Pdf
GUIDEBOOK FOR PATIENTS BC Cancer – Surrey BC Cancer – Surrey 13750 96 Avenue Surrey, BC www.bccancer.bc.ca Contents Introduction to BC Cancer __________________________________ 3 Partners in Care: our mutual commitments _____________________ 4 STOP for the protection of our patients ________________________ 5 BC Cancer – Surrey floor-by-floor services/facilities _______________ 6 Where can I park? _________________________________________7 How can I arrange for transportation? _________________________ 8 What do I need to bring to my first visit? _______________________10 What happens at my first visit? _______________________________10 Who may be on my healthcare team? _________________________12 What kinds of questions can I ask my doctor? ___________________13 What resources are available to me at BC Cancer – Surrey? _________14 Resources within BC Cancer ________________________________19 What other resources are available to me in the community? _______22 Frequently asked questions _________________________________24 Where can I get information on Fair Pharmacare? _______________ 26 How is my personal data collected, used and shared? _____________27 Advance care planning ____________________________________ 29 Glossary of terms ________________________________________ 30 BC Cancer – Surrey contact list _______________________________32 BC Cancer call navigation __________________________________33 Hospitals & other centres __________________________________ 34 Where is the BC Cancer centre where I will receive treatment? ______35 -

University of British Columbia Curriculum Vitae for Faculty Members
University of British Columbia Curriculum Vitae for Faculty Members Date: Sept 13 2018 Verification Initial: 1. SURNAME: Beattie FIRST NAME: Beverley MIDDLE NAME(S): Lynn 2. DEPARTMENT/SCHOOL: Medicine 3. FACULTY: Medicine JOINT APPOINTMENTS: ASSOCIATE Neuroethics Canada APPOINTMENTS: 4. PRESENT RANK: Professor Emerita SINCE: Jul 1, 2005 5. POST-SECONDARY EDUCATION (a) University or Institution Degree Subject Area Dates University of British Columbia MD Medicine 1961/07 - 1965/06 (b) Title of Dissertation and Name of Supervisor (c) Continuing Education or Training (d) Continuing Medical Education (e) Professional Qualifications 1 1982 Certificate of Special Competence in Geriatric Medicine, Royal College of Physicians and Surgeons of Canada 2 1970 Fellow, Royal College of Physicians and Surgeons of Canada (FRCPC) 6. EMPLOYMENT RECORD (a) Prior University, Company or OrganiZation Rank or Title Dates UBC Professor Emerita 2005/07/01 – to date Printed: 15/Jan/2013 Beattie , B. Lynn 1 Providence Health Care Interim Head, Division of 2004/07/01 - 2005/06/30 Geriatric Medicine and Director Centre for Healthy 2004 - 2010 Aging (CHAP) UBC Associate Member, School of 1994/07/01 - 2005/06/30 Rehabilitation Medicine UBC Professor, Division of Geriatric 1994/07/01 - 2005/06/30 Medicine UBC Head, Division of Geriatric 1980/07/01 - 1998/06/30 Medicine UBC Clinic for AlZheimer Disease and Director and Clinician 1983/07/01 – 2005/06/30 Related Disorders and 2007 - 2013/04/30 UBC Associate Professor, Division of 1983/07/01 - 1994/06/30 Geriatric Medicine -

Carms Manual Copy
UNIVERSITY OF BRITISH COLUMBIA DEPARTMENT OF PSYCHIATRY CaRMS Information Package DEPARTMENT OF PSYCHIATRY FACULTY OF MEDICINE QUESTIONS ABOUT INTERVIEW SCHEDULE? CONTACT DETWILLER PAVILION 2255 WESBROOK MALL LUIZA SHAMKULOVA VANCOUVER, BC CANADA V6T 2A1 POSTGRADUATE COORDINATOR TEL 604-822-7314 604-875-4111 x 68092 FAX 604-822-7756 WEBSITE PSYCHIATRY.UBC.CA Page 1 of 35 | Table of Contents Letter from the CaRMS Committee Dear CaRMS Applicant, The University of British Columbia Psychiatry program offers a diverse array of exceptional training in all core competencies outlined by the Royal College of Physicians and Surgeons of Canada. The philosophy of our program is to train psychiatrists in the broad aspects of the bio-psycho-social model of medicine and psychiatry and to prepare interested residents for further subspecialty training or fellowships. Our psychotherapy and pharmacologic training is excellent, and research is actively encouraged. One day per week is dedicated to academic seminars (academic day). For those residents with expertise and interest in research, a specially tailored training track has been developed that maximizes available research time within the Royal College’s training guidelines. Many research opportunities also exist for all trainees outside of the research track, with projects being developed by the third year of training and completed during elective time in the last year of training. As with all tracks, one day per week is dedicated to academic seminars (academic day). Through an integrated program of clinical placements and academic seminars, our program is designed to achieve the training goals of the Royal College of Physicians and Surgeons of Canada and the University of British Columbia. -

UBC-Medicine-Fall-2104 Low-Res.Pdf
10 Repairing the damage An instructor exposes students to the country 2 he fled Nº 2014 18 Brain change 10 Can a curriculum alter kids’ neurons? VOL FALL 20 Chuck Fipke’s passion for exploration First for diamonds, now MEDICINE for an Alzheimer’s cure THE MAGAZINE OF THE UNIVERSITY OF BRITISH COLUMBIA FACULTY OF MEDICINE THE MEDICINE MAN HOW UBC PUT JAMES CARD ON THE ROAD NORTH, TO A TOWN THAT DESPERATELY NEEDED HIM A centesimal 14 celebration “IF YOU KEEP HATING, IT EATS AWAY AT YOU” 10 CONTENTS 01 Message from the Vice 16 Investigations + Breakthroughs Provost Health and Dean 18 Brain change: Can a curriculum Chuck Fipke’s 02 The Medicine Man: A distributed alter kids’ neurons? passion for education success story 20 Chuck Fipke’s passion for 20 exploration 06 “You Can’t Do That”: How exploration – first for diamonds, UBC’s innovation was emulated now for an Alzheimer’s cure across Canada, and overseas 22 A vision for the Downtown 08 Problem. Response. Outcomes. Eastside: Better eyesight 10 years of distributed medical 23 A donor finds inspiration across A donor finds education a crowded room inspiration, 10 Repairing the damage: An 24 Chew Wei and Tak Mak: Two 23 across a instructor exposes students to immigrants linked by their the country he fled crowded room contributions to Canadian health 13 Speech-language pathology 25 Medical Alumni News prepares for a big jump 14 A centesimal celebration: Midwifery and Genetic Counselling graduate their 100th students UBC MEDICINE VOL. 10 | NO. 2 Fall 2014 A publication of the University of British Columbia’s Faculty of Medicine, providing news and information for and about faculty members, students, staff, alumni and friends.