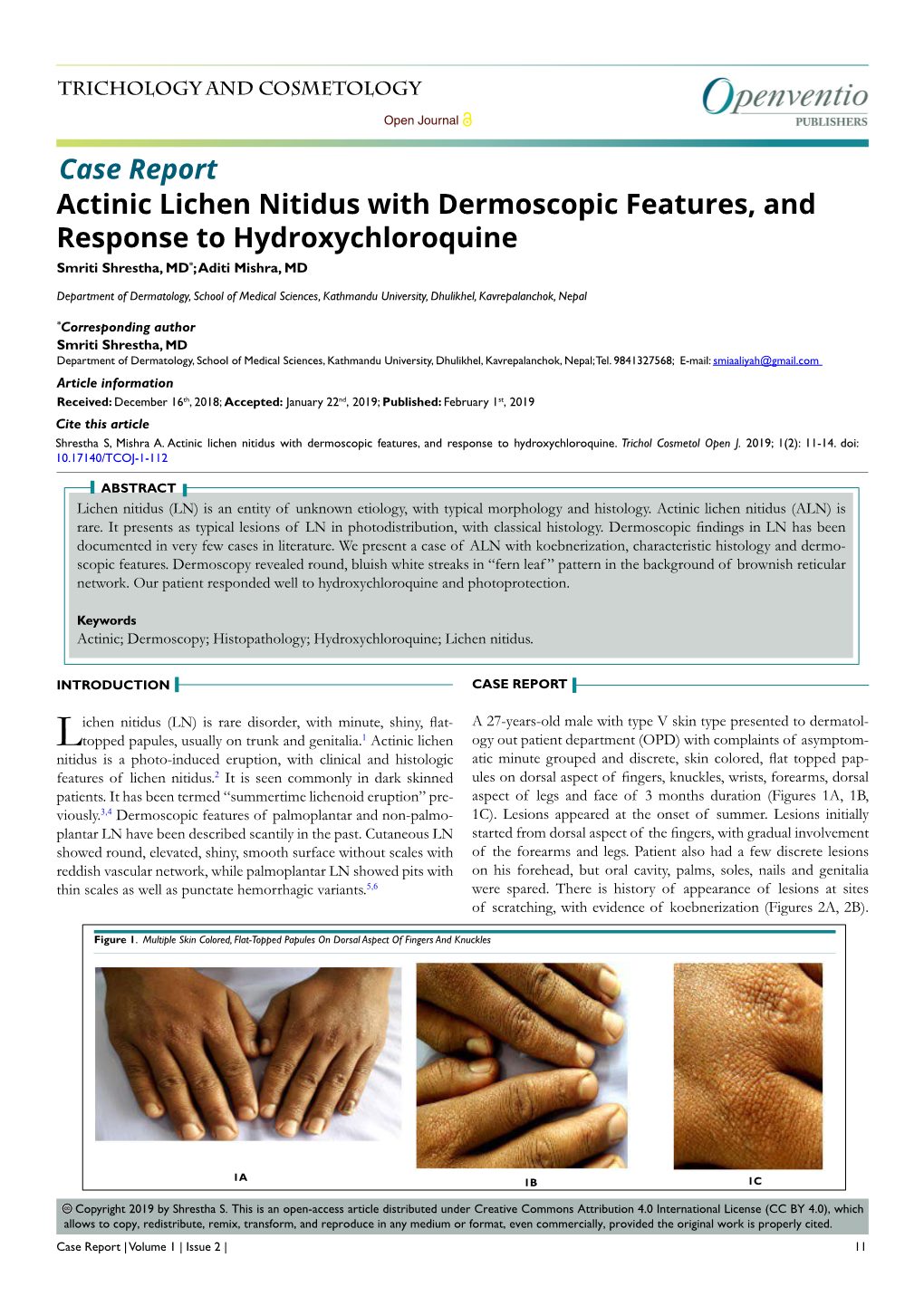
Actinic Lichen Nitidus with Dermoscopic Features, and Response to Hydroxychloroquine Case Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hyperkeratotic and Hypertrophic Lichen Nitidus
Volume 23 Number 10 | October 2017 Dermatology Online Journal || Case Presentation 23 (10): 15 Hyperkeratotic and hypertrophic lichen nitidus Jonathan D Ho1,2 MBBS DSc Dip.Dermpath, Ali Al-Haseni1 MD MSC, Michael T Rosenbaum1 MD, Lynne J Goldberg1,2 MD Affiliations:1 Department of Dermatology, Boston University School of Medicine, Boston, Massachusetts 2Section of Dermatopathology, Boston University School of Medicine, Boston, Massachusetts Corresponding Author: Ali Al-Haseni MD, 609 Albany Street, Boston MA 02118, Email: [email protected] Abstract interphalangeal joints of the fingers on both hands (Figure 1A). Biopsy demonstrated marked Lichen nitidus typically presents as shiny pin- orthokeratosis, hypergranulosis, and lichen simplex head sized papules on the trunk and extremities, chronicus-like irregular epidermal hyperplasia. A often affecting children and young adults. In this multifocal lichenoid lymphohistiocytic infiltrate prototypical form, it rarely presents a diagnostic expanding one or two dermal papillae with overlying challenge being characterized by distinctive clinical parakeratosis, associated focal hypogranulosis, and and histopathologic findings. We describe a rare occasional individually necrotic keratinocytes were variant of lichen nitidus, which we term “hyperkeratotic noted (Figure 2). These findings were diagnostic and hypertrophic lichen nitidus.” of lichen nitidus. Unusually, the histopathologic and clinically correlated epidermal changes were Keywords: lichen nitidus, hyperkeratosis, somewhat exuberant -

ORIGINAL ARTICLE a Clinical and Histopathological Study of Lichenoid Eruption of Skin in Two Tertiary Care Hospitals of Dhaka
ORIGINAL ARTICLE A Clinical and Histopathological study of Lichenoid Eruption of Skin in Two Tertiary Care Hospitals of Dhaka. Khaled A1, Banu SG 2, Kamal M 3, Manzoor J 4, Nasir TA 5 Introduction studies from other countries. Skin diseases manifested by lichenoid eruption, With this background, this present study was is common in our country. Patients usually undertaken to know the clinical and attend the skin disease clinic in advanced stage histopathological pattern of lichenoid eruption, of disease because of improper treatment due to age and sex distribution of the diseases and to difficulties in differentiation of myriads of well assess the clinical diagnostic accuracy by established diseases which present as lichenoid histopathology. eruption. When we call a clinical eruption lichenoid, we Materials and Method usually mean it resembles lichen planus1, the A total of 134 cases were included in this study prototype of this group of disease. The term and these cases were collected from lichenoid used clinically to describe a flat Bangabandhu Sheikh Mujib Medical University topped, shiny papular eruption resembling 2 (Jan 2003 to Feb 2005) and Apollo Hospitals lichen planus. Histopathologically these Dhaka (Oct 2006 to May 2008), both of these are diseases show lichenoid tissue reaction. The large tertiary care hospitals in Dhaka. Biopsy lichenoid tissue reaction is characterized by specimen from patients of all age group having epidermal basal cell damage that is intimately lichenoid eruption was included in this study. associated with massive infiltration of T cells in 3 Detailed clinical history including age, sex, upper dermis. distribution of lesions, presence of itching, The spectrum of clinical diseases related to exacerbating factors, drug history, family history lichenoid tissue reaction is wider and usually and any systemic manifestation were noted. -

Down's Syndrome with Lichen Nitidus and Segmental Vitiligo
Letters to the Editor and liver manifestations. Retinoids are useful in the and pitryiasis rubra pilaris. We describe a four-year- treatment of skin and muscle manifestations.[2] old girl with Down’s syndrome, with segmental vitiligo and lichen nitidus. Tzanck smear may provide important information in a patient with suspected DCS. A four-year-old female child with Down’s syndrome [Figure 1] presented to us with white patches on the MMuraturat DDurdu,urdu, FFahrettinahrettin AAkaykay1, TTevevÞ k AAlperlper2, right waist and inguinal area for the last one month. SSerkanerkan YYaaşaarr ÇÇelikelik3 She also had asymptomatic papules on the legs for Başkent University Faculty of Medicine, Department of Dermatology, the same duration. She did not have any systemic Adana Hospital, Adana/Turkey, Department of 1Ophthalmology, complaints. On examination, she had segmental vitiligo 2Internal Medicine, 3Pathology, Diyarbakõr Military Hospital, [Figure 2] on the right waist. The vitiliginous macule Diyarbakõr, Turkey had an irregular border and leucotrichia. She also had AAddressddress fforor ccorrespondenceorrespondence: Dr. Murat Durdu, multiple, discrete, flat, round, smooth, skin-colored- Başkent University Faculty of Medicine, to-slightly pink papules of 1 to 2 mm size, distributed Department of Dermatology, Adana Hospital, 01250, symmetrically over the extensors of both the legs and Adana/Turkey. E-mail: [email protected] thighs [Figure 3]. The rest of the skin, hair, and nails DOI: 10.4103/0378-6323.57737 - PMID: 19915256 were normal. Manifestations of Down’s Syndrome RREFERENCESEFERENCES in our case were hypertelorism, depressed nose, epicanthal folds, high-arched palate, flat occiput, low- 1. Ben Selma Z, Yilmaz S, Schischmanoff PO, Blom A, Ozogul C, set ears, hypotonia, sandle toe, flat feet, clinodactyly, Laroche L, et al. -

Simultaneous Occurrence of Lichen Nitidus and Morphea
Yonago Acta Medica 2021;**(*):***–*** doi: 10.33160/yam.2021.05.006 Patient Report Simultaneous Occurrence of Lichen Nitidus and Morphea Yuko Ehara,* Yuichi Yoshida,* Kazunari Sugita* and Osamu Yamamoto* *Division of Dermatology, Department of Medicine of Sensory and Motor Organs, School of Medicine, Faculty of Medicine, Tottori University, Yonago 683-8503, Japan ABSTRACT plaques (Fig. 1b). Dermoscopically, the papules were Lichen nitidus and morphea are common diseases, but shown to be well-defined circular hypopigmented an associated localization of both lesions is rare. Here, structures (Fig. 1c). Clinical differential diagnosis we describe the first case of lesions distributed along included atrophoderma, morphea and ashy dermatosis. Blaschko’s lines. A 24-year-old Japanese woman was Histopathologically, there was sclerosis in the lower referred to our clinic for evaluation of band-like plaques half of the dermis (Fig. 1d) and perivascular lympho- of 18-months history on the right lateral side of her ab- plasmacytic infiltration near the eccrine glands (Fig. domen. In addition, multiple milky-white papules were 1e). In addition, we observed well-circumscribed, seen within the plaques. Histopathological examination dense, papillary dermal lymphohistiocytic aggregations showed there was sclerosis in the lower half of the showing a so-called”claw clutching a ball”pattern (Fig. dermis and well-circumscribed, dense, papillary dermal 1f). Immunohistochemically, these aggregations were lymphohistiocytic aggregations showing a so-called mainly composed of CD4+ and CD8+ lymphocytes and “claw clutching a ball.” Immunohistochemical analysis some CD68+ cells (Figs. 1g, h, and i). In addition, the revealed that the morphea and lichen nitidus had similar aggregations also contained S-100 protein+ and CD1a+ characteristics. -

Linear Lichen Planus: Two Case Reports
ANATOL J FAMILY MED Case Report The Anatolian Journal of Family Medicine DOI: 10.5505/anatoljfm.2018.25633 Anatol J Family Med 2019;2(1):41–4 Linear Lichen Planus: Two Case Reports Gülhan Gürel,1 Sevinç Şahin,2 Emine Çölgeçen1 1Department of Dermatology, Bozok University School of Medicine, Yozgat, Turkey 2Department of Pathology, Bozok University School of Medicine, Yozgat, Turkey ABSTRACT Lichen planus (LP) is an idiopathic inflammatory skin disease which affects the skin, mucosa, nails, and hairs of middle-aged individuals. Linear lichen planus (LLP) is a rare variant of LP characterized by pruritic, lichenoid appearance, violaceous-color papules in a linear pattern. About 0.24 to 0.62% of patients with LP have been reported to have LLP. In cases with LP, linear lesions can be post-traumatically seen as widespread generalized eruptions (Koebner phenomenon) and as zosteriforms on herpes infection as the Wolf’s isotopic response. However, LLP indicates the presence of spontaneous LLP lesions which follow Blaschko’s lines without any previous association with trauma or herpes infection. Herein, we present two cases with LLP and emphasize the rarity of these cases and the importance of linear lesions in the differential diagnosis. Keywords: Dermatosis, lichen planus, skin diseases INTRODUCTION Lichen planus (LP) was first described in 1869 by Erasmus Wilson.[1] It is mostly seen in adults aged 30 to 60 years and affects 0.14 to 0.8% of the population. LP is classified according to the location, distribution, and morphology of the lesion and nearly 20 clinical forms have been described as eruptive, localized, annular, linear, hypertrophic, nodular, atrophic, bullous, ero- Please cite this article as: [2] Gürel G, Şahin S, Çölgeçen E. -

Lesions' Pattern Helps Line up Diagnosis
DERMADIAGNOSIS Lesions’ Pattern Helps Line Up Diagnosis ix months ago, a 6-year-old records provided by his primary boy developed asymptom- care provider’s office. Satic lesions on his elbows, The lesions are particularly then his knees. They slowly spread numerous over the extensor sur- to other areas, including his fore- faces of the legs—especially the arms. One primary care provider knees—but are also seen on the diagnosed probable warts; an- extensor forearms and elbows. other, molluscum. The prescribed The lesions are exquisitely dis- treatments—liquid nitrogen and crete, identical, tiny white pin- tretinoin, respectively—had no point papules, all with flat tops. effect. None are umbilicated. In several The boy’s mother became areas of the arms, linear collec- alarmed when the lesions started tions of lesions, some extending to form in long lines on his arms. as long as 6 cm, are noted. The At that point, she decided to bring rest of his exposed type V skin is him to dermatology for evalua- unremarkable. tion. Aside from his skin condi- The most likely diagnostic ex- tion, the child is healthy, accord- planation for these lesions is ing to both his mother and the a) Molluscum contagiosum b) Lichen nitidus Joe R. Monroe, c) Warts MPAS, PA, practices d) Lichen planus at Dawkins Dermatology Clinic in Oklahoma City. ANSWER He is also the The correct answer is lichen niti- founder of the dus (choice “b”), a harmless, self- Society of Dermatology limited condition of unknown Physician Assistants. origin. The lesions’ flat-topped 10 Clinician Reviews • FEBRUARY 2015 clinicianreviews.com (planar) surfaces and tendency best way to highlight it is with ent in this manner are psoriasis, to form in linear configurations a short blast of liquid nitrogen. -

Histopathological and Clinical Correlation of Hyperpigmented Skin Lesions Dr
Scholars Journal of Applied Medical Sciences Abbreviated Key Title: Sch J App Med Sci ISSN 2347-954X (Print) | ISSN 2320-6691 (Online) Journal homepage: https://saspublishers.com/sjams/ Pathology Histopathological and Clinical Correlation of Hyperpigmented Skin Lesions Dr. Sneha Ravindran1, Dr. Kalla Ravi Teja2*, Dr. Arun Kumar SP3, Dr. Jonathan Arnold4, Dr. Balaji S4 1Post Graduate, Department of Pathology, SVMCH, Puducherry, India 2Assistant Professor, Department of Pathology, SVMCH, Puducherry, India 3Professor and HOD, Department of Pathology, SVMCH, Puducherry, India 4Associate Professor, Department of Pathology, SVMCH, Puducherry, India 5Post Graduate, Department of Pathology, SVMCH, Puducherry, India DOI: 10.36347/sjams.2020.v08i11.007 | Received: 16.10.2020 | Accepted: 30.10.2020 | Published: 12.11.2020 *Corresponding author: Dr. Sneha Ravindran Abstract Original Research Article Introduction: The spectrum of clinical disease related to hyperpigmented lesion is wider. The most common hyperpigmented skin lesion is lichen planus and its variants. Histopathological examination helps to derive an accurate tissue reaction. Pathologic examination often serves as a confirmative diagnosis for skin lesions. The histology-based treatment will be helpful for establishing a standardized management for hyperpigmentary skin lesions. Materials and Methods: A total of 100 patients with hyperpigmented punch skin biopsy lesions in all age groups following inclusion and exclusion criteria is taken and examined for histopathological correlation from the Department of Pathology. Result: In this study of hyperpigmented skin lesions the maximum number of cases 45 (45%) were those of classical Lichen planus and its variants, followed by 12% of eczematoid dermatitis, 8% of PMLE, 7%of DLE, 6% of lichen simplex chronicus, 7% of post inflammatory hyperpigmentation, 3% of prurigo nodularis, 4% of prurigo simplex, morphea 4%, acne 3%, and 1% of erythema dyschromium perstans. -

Generalized Lichen Nitidus Successfully Treated with Narrow-Band UVB Phototherapy : Two Cases Report
J Korean Med Sci 2007; 22: 163-6 Copyright � The Korean Academy ISSN 1011-8934 of Medical Sciences Generalized Lichen Nitidus Successfully Treated with Narrow-band UVB Phototherapy : Two Cases Report Lichen nitidus (LN) is an uncommon chronic inflammatory skin disease composed Mi-Ok Do, Myoung-Ju Kim, of numerous, tiny, shiny, flesh-colored papules that are predominantly observed on Seong-Hyun Kim, Ki-Bum Myung, the chest, abdomen, glans penis and upper extremities. The distribution of LN is You-Won Choi most often localized, but in some cases it can become generalized. Because LN Department of Dermatology, College of Medicine, tends to be asymptomatic and presents spontaneous resolution within several years, Ewha Womans University, Seoul, Korea it usually does not require treatment except in symptomatic, persistent and gener- alized cases. We describe a 28-yr-old man and a 7-yr-old boy with generalized LN Received : 27 July 2005 where both cases improved with narrow-band ultraviolet B (NB-UVB) phototherapy Accepted : 27 October 2005 plus topical steroid ointment. Both patients noted improvement within the first three treatments and showed almost complete resolution after 18 and 20 treatments, res- Address for correspondence You-Won Choi, M.D. pectively. NB-UVB phototherapy may be an effective alternative therapy for the treat- Department of Dermatology, Ewha Womans University ment of generalized LN, even for those patients in their childhood. Mokdong Hospital, 911-1 Mok-dong, Yangcheon-gu, Seoul 158-710, Korea Key Words : Skin Diseases; Lichenoid Eruptions; Lichen Nitidus; Narrow-band UVB; Phototherapy; Ultravio- Tel : +82.2-2650-5159, Fax : +82.2-2652-6925 let Therapy E-mail : [email protected] INTRODUCTION head-sized papules that involved the trunk, upper extremi- ties and palms including the fingers. -

Lichen Planus and Lichenoid Dermatoses: Clinical Overview and Molecular Basis
King’s Research Portal DOI: 10.1016/j.jaad.2018.02.010 Document Version Peer reviewed version Link to publication record in King's Research Portal Citation for published version (APA): Tziotzios, C., Lee, J. Y. W., Brier, T., Saito, R., Hsu, C-K., Bhargava, K., Stefanato, C., Fenton, D. A., & McGrath, J. A. (2018). Lichen planus and lichenoid dermatoses: clinical overview and molecular basis. Journal of the American Academy of Dermatology, 789. https://doi.org/10.1016/j.jaad.2018.02.010 Citing this paper Please note that where the full-text provided on King's Research Portal is the Author Accepted Manuscript or Post-Print version this may differ from the final Published version. If citing, it is advised that you check and use the publisher's definitive version for pagination, volume/issue, and date of publication details. And where the final published version is provided on the Research Portal, if citing you are again advised to check the publisher's website for any subsequent corrections. General rights Copyright and moral rights for the publications made accessible in the Research Portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognize and abide by the legal requirements associated with these rights. •Users may download and print one copy of any publication from the Research Portal for the purpose of private study or research. •You may not further distribute the material or use it for any profit-making activity or commercial gain •You may freely distribute the URL identifying the publication in the Research Portal Take down policy If you believe that this document breaches copyright please contact [email protected] providing details, and we will remove access to the work immediately and investigate your claim. -

Clinical Pattern of Papulosquamous Dermatoses: an Observational Study Conducted at Tertiary Care Center, Ujjain, Madhya Pradesh, India
International Journal of Research in Dermatology Varma K et al. Int J Res Dermatol. 2020 Mar;6(2):230-236 http://www.ijord.com DOI: http://dx.doi.org/10.18203/issn.2455-4529.IntJResDermatol20200602 Original Research Article Clinical pattern of papulosquamous dermatoses: an observational study conducted at tertiary care center, Ujjain, Madhya Pradesh, India Krishnendra Varma, Ujjwal Kumar, Varun Kumar* Department of Dermatology, Venereology and Leprology, R.D Gardi Medical College, Ujjain, Madhya Pradesh, India Received: 11 November 2019 Accepted: 10 January 2020 *Correspondence: Dr. Varun Kumar, E-mail: [email protected] Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT Background: Papulosquamous dermatoses is a complex group of disorder characterized by scaly papules and plaques. There is a need to study the exact, pattern and prevalence of this disorder in different age groups and their line of treatment. Objective of the study was to observe the clinical pattern of various papulosquamous dermatoses and their prevalence at tertiary care center, Ujjain. Methods: This was an observational study done in R.D. Gardi Medical college, Ujjain over a period of one year. A total of 229 cases including male and female of papulosquamous dermatoses were enrolled from the outpatient department. All patients were studied clinically and relevant data was recorded. Microsoft excel was used for data entry and analysis was done using SPSS version 23. -

Study of Noninfectious Papulosquamous Lesions- an Experience at a Teritiary Hospital
Indian Journal of Pathology and Oncology 2020;7(1):43–48 Content available at: iponlinejournal.com Indian Journal of Pathology and Oncology Journal homepage: www.innovativepublication.com Original Research Article Study of noninfectious papulosquamous lesions- An experience at a teritiary hospital Vidya Kedarisetti1, V Krishna Kumar1, C Shalini1,* 1Dept. of Pathology, Mediciti Institute of Medical Sciences, Ghanpur, Telangana, India ARTICLEINFO ABSTRACT Article history: Objectives: To study the spectrum and have a clinicopathological correlation of papulosquamous skin Received 13-06-2019 lesions. Accepted 05-08-2019 Material and Methods: A series of noninfectious papulosquamous skin lesions coming to Department Available online 22-02-2020 of Dermatology were studied over a period of one year, i.e. from June 2017 to July 2018. These were correlated and analysed with the histopathological findings. Results: The present study comprised of 70 cases of skin diseases presenting as papulosquamous lesions. Keywords: Majority of cases were in the age group of 31 to 40 years (16 cases, 22.8%) followed by 11 to 20 years Papulosquamous skin lesions (15 cases, 21.4%). Females were more commonly affected with 37 cases(52.8%) compared to males with Psoriasis 33cases (47.1%) and female to male ratio of incidence being 1:0.89. Lichen planus In the present study, out of 70 cases, 34 cases (48.5%) were diagnosed as psoriasis, Lichen planus- Clinicopathological correlation 15 cases(21.4%), Chronic Dermatitis- 4 cases (5.71%), Lichen striatus- 3 cases (4.28%), Pityriasis Psoriasiform reaction Lichenoides- 2 cases(2.85%), Pityriasis Rosea- 2 cases (2.85%), Prurigo Simplex- 2 cases(2.8%), Prurigo Lichenoid reaction. -

A Clinical Study on Papulosquamous Disorders in Children Less Than 12 Years
A CLINICAL STUDY ON PAPULOSQUAMOUS DISORDERS IN CHILDREN LESS THAN 12 YEARS Dissertation submitted to THE TAMILNADU DR. M.G.R. MEDICAL UNIVERSITY CHENNAI – 600 032 APRIL 2015 in partial fulfillment of the regulations required for the award of M.D. DEGREE IN DERMATOLOGY, VENEREOLOGYAND LEPROLOGY (BRANCH XII ) DEPARTMENT OF DERMATOLOGY, VENEREOLOGY AND LEPROLOGY COIMBATORE MEDICAL COLLEGE HOSPITAL DECLARATION I Dr. PREETHA PRASAD solemnly declare that the dissertation entitled “A CLINICAL STUDY ON PAPULOSQUAMOUS DISORDERS IN CHILDREN LESS THAN 12 YEARS” was done by me in the Department of Dermatology and Venereology at Coimbatore Medical College Hospital during the period from August 2013 to July 2014 under the guidance & supervision of Dr. P. P. RAMASAMY M.D., D.D., Professor & Head of Department, Department of Dermatology and Venereology, Coimbatore Medical College Hospital, Coimbatore. The dissertation is submitted to Tamil Nadu Dr. MGR Medical University, Chennai towards the partial fulfillment of the requirement for the award of M.D., degree in Dermatology, Venereology and Leprology.I have not submitted this dissertion on any previous occasion to any university for the award of any degree. PLACE: Dr. PREETHA PRASAD DATE: CERTIFICATE This is to certify that the dissertation entitled “A CLINICAL STUDY ON PAPULOSQUAMOUSDISORDERS IN CHILDREN LESS THAN 12 YEARS” is a record of bonafide work done by Dr. PREETHA PRASAD, Post graduate student in the Department of Dermatology, Venereology and Leprology,Coimbatore Medical College Hospital, Coimbatore under the guidance of Dr.P.P.Ramasamy M.D.,D.D., Professor & Head of Department, Department of Dermatology, Coimbatore Medical College Hospital, Coimbatore in partial fulfillment of the regulations of the Tamilnadu Dr.M.G.R Medical University, Chennai towards the award of M.D., degree(Branch XII) in Dermatology, Venereology and Leprology.