Atrial Fibrillation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pacemaker Syndrome Pacemaker Therapy Has Become an Important Therapeutic Option for Patients with Heart Rhythm Conditions Worldwide
360 Cardiology Pacemaker syndrome Pacemaker therapy has become an important therapeutic option for patients with heart rhythm conditions worldwide. Te number of elderly patients needing pacemakers is on the increase due to an ageing population worldwide. Pacemaker syndrome consists of the cardiovascular signs and symptoms of heart failure and hypotension induced by right ventricular (RV) pacing. Dr Satnam Singh Research Registrar, University of Aberdeen, Level 3, Polwarth building, Aberdeen email [email protected] Pacemaker syndrome is a term syndrome occurring in dual trial was a single blinded study proposed in 1979 by Erbel and chamber modes.5,6 It can even enrolling around 2000 patients refers to symptoms and signs in occur with AAI pacing with long with sick sinus syndrome. the pacemaker patient caused by PR intervals. All patients were implanted inadequate timing of atrial and dual chamber pacemakers ventricular contractions.1 It was first programmed to VVIR or DDDR described in 1969 by Mitsui et al2 as Incidence before implantation. Pacemaker an iatrogenic disease characterised syndrome was a secondary by the disappearance of symptoms Te overall incidence of pacemaker endpoint studied. Severe with restoration of atrioventricular syndrome is very difficult to pacemaker syndrome developed synchrony (AV synchrony). estimate but is about 20% in a in nearly 20% of VVIR-paced It means if atria and ventricles landmark trial called the Mode patients and improved with contract at appropriate timings (as Selection Trial (MOST).7 It occurs reprogramming to the dual- close to physiological), pacemaker with equal frequency in both sexes chamber pacing mode. syndrome can be prevented. -

How to Define Valvular Atrial Fibrillation?
Archives of Cardiovascular Disease (2015) 108, 530—539 Available online at ScienceDirect www.sciencedirect.com REVIEW How to define valvular atrial fibrillation? Comment définir la fibrillation atriale valvulaire ? ∗ Laurent Fauchier , Raphael Philippart, Nicolas Clementy, Thierry Bourguignon, Denis Angoulvant, Fabrice Ivanes, Dominique Babuty, Anne Bernard Service de cardiologie, faculté de médecine, université Franc¸ois-Rabelais, CHU Trousseau, Tours, France Received 3 June 2015; accepted 8 June 2015 Available online 14 July 2015 KEYWORDS Summary Atrial fibrillation (AF) confers a substantial risk of stroke. Recent trials compar- Atrial fibrillation; ing vitamin K antagonists (VKAs) with non-vitamin K antagonist oral anticoagulants (NOACs) in Valve disease; AF were performed among patients with so-called ‘‘non-valvular’’ AF. The distinction between Stroke ‘‘valvular’’ and ‘‘non-valvular’’ AF remains a matter of debate. Currently, ‘‘valvular AF’’ refers to patients with mitral stenosis or artificial heart valves (and valve repair in North American guidelines only), and should be treated with VKAs. Valvular heart diseases, such as mitral regur- gitation, aortic stenosis (AS) and aortic insufficiency, do not result in conditions of low flow in the left atrium, and do not apparently increase the risk of thromboembolism brought by AF. Post-hoc analyses suggest that these conditions probably do not make the thromboembolic risk less responsive to NOACs compared with most forms of ‘‘non-valvular’’ AF. The pathogenesis of thrombosis is probably different for blood coming into contact with a mechanical prosthetic valve compared with what occurs in most other forms of AF. This may explain the results of the only trial performed with a NOAC in patients with a mechanical prosthetic valve (only a few of whom had AF), where warfarin was more effective and safer than dabigatran. -

Mitral Stenosis and Atrial Fibrillation Funding the Authors Have Not Declared a Specific Heart: First Published As 10.1136/Heartjnl-2019-316282 on 6 February 2020
Editorial Contributors DW and BS wrote the editorial together. Mitral stenosis and atrial fibrillation Funding The authors have not declared a specific Heart: first published as 10.1136/heartjnl-2019-316282 on 6 February 2020. Downloaded from grant for this research from any funding agency in the Dirk Westermann , Benedikt Schrage public, commercial or not- for- profit sectors. Competing interests None declared. Patient consent for publication Not required. Over the past decades, the incidence of Health Insurance Review and Assessment mitral stenosis (MS) due to rheumatic Service database, which covers 98% of the Provenance and peer review Commissioned; internally peer reviewed. fever has markedly decreased. Regardless, overall South Korean population, Kim et rheumatic fever remains associated with al4 describe a cohort of 42 075 patients about 80% of all cases of MS, and so rela- diagnosed with MS between 2007 and tively the most relevant contributor to 2016. In their study, the authors observed MS.1 Aside from rare causes such as a decreasing incidence of MS during the congenital MS, MS due to myxoma or MS study period, from 10.3 to 3.6 cases per following infiltrating diseases, another 100 000 inhabitants. While this data source Open access This is an open access article distributed in accordance with the Creative Commons Attribution important cause of MS is indeed severe does not allow indepth analysis of patient Non Commercial (CC BY- NC 4.0) license, which permits calcification of the mitral annulus and its data, it is important due to the large popu- others to distribute, remix, adapt, build upon this work leaflets. -

Atrial Fibrillation in Hypertrophic Cardiomyopathy: Prevalence, Clinical Impact, and Management
Heart Failure Reviews (2019) 24:189–197 https://doi.org/10.1007/s10741-018-9752-6 Atrial fibrillation in hypertrophic cardiomyopathy: prevalence, clinical impact, and management Lohit Garg 1 & Manasvi Gupta2 & Syed Rafay Ali Sabzwari1 & Sahil Agrawal3 & Manyoo Agarwal4 & Talha Nazir1 & Jeffrey Gordon1 & Babak Bozorgnia1 & Matthew W. Martinez1 Published online: 19 November 2018 # Springer Science+Business Media, LLC, part of Springer Nature 2018 Abstract Hypertrophic cardiomyopathy (HCM) is the most common hereditary cardiomyopathy characterized by left ventricular hyper- trophy and spectrum of clinical manifestation. Atrial fibrillation (AF) is a common sustained arrhythmia in HCM patients and is primarily related to left atrial dilatation and remodeling. There are several clinical, electrocardiographic (ECG), and echocardio- graphic (ECHO) features that have been associated with development of AF in HCM patients; strongest predictors are left atrial size, age, and heart failure class. AF can lead to progressive functional decline, worsening heart failure and increased risk for systemic thromboembolism. The management of AF in HCM patient focuses on symptom alleviation (managed with rate and/or rhythm control methods) and prevention of complications such as thromboembolism (prevented with anticoagulation). Finally, recent evidence suggests that early rhythm control strategy may result in more favorable short- and long-term outcomes. Keywords Atrial fibrillation . Hypertrophic cardiomyopathy . Treatment . Antiarrhythmic agents Introduction amyloidosis) [3–5]. The clinical presentation of HCM is het- erogeneous and includes an asymptomatic state, heart failure Hypertrophic cardiomyopathy (HCM) is the most common syndrome due to diastolic dysfunction or left ventricular out- inherited cardiomyopathy due to mutation in one of the sev- flow (LVOT) obstruction, arrhythmias (atrial fibrillation and eral sarcomere genes and transmitted in autosomal dominant embolism), and sudden cardiac death [1, 6]. -

Treatment of Atrial Fibrillation in Hypertrophic Cardiomyopathy Hipertrofik Kardiyomiyopatide Atriyal Fibrilasyonun Tedavisi
44 Treatment of atrial fibrillation in hypertrophic cardiomyopathy Hipertrofik kardiyomiyopatide atriyal fibrilasyonun tedavisi Khashayar Hematpour, Jonathan S. Steinberg Division of Cardiology, St. Luke's-Roosevelt Hospital Center, New York, NY, USA ABSTRACT Atrial fibrillation (AF) is present in 5 percent of hypertrophic cardiomyopathy (HCM) patients at the time of diagnosis. Ostial pulmonary vein (PV) diameter is increased in patients with AF as well as hypertensive patients. These findings support the theory that the cascade of events leading to diastolic dysfunction might predispose a person to AF by stretching the PVs. This mechanism is likely relevant to AF in HCM as well. The recognition that AF often times arises from the PVs has led to innovation of ablation techniques that target this zone to electrically isolate the PVs from the left atrium (LA). Anticoagulation is the cornerstone of AF treatment. Additional AF treatment in HCM patients de- pends on the initial decision regarding need for surgical intervention, whether or not AF is permanent, and the severity of symptoms in pati- ents with non-permanent AF. If surgery is planned, correction of the arrhythmia with MAZE procedure, which isolates the arrhythmogenic foci, at the time of myectomy is an option to consider. The goal in HCM patients with permanent AF is to control the heart rate whether by chronic medications or through ablate + pace procedure. Based on the severity of symptoms, HCM patients with non-permanent AF will be treated with either the rate control strategy (β-blockers/calcium channel blocker) or the rhythm control strategy (PV ablation, antiarrhyth- mic drugs, or radiofrequency ablation of the LA). -

Pacemaker Syndrome: an Iatrogenic Condition
Br Heart J 1992;68:163-6 163 VIEWPOINT Pacemaker syndrome: an iatrogenic condition Christopher M Travill, Richard Sutton Pacemaker syndrome was first described in inhibited (VVI) pacing was used. In the re- 1969 by Mitsui when it was referred to as the maining 20 patients with no history of pacemaking syndrome.' The name pacemaker pacemaker syndrome or ventriculoatrial con- syndrome was first coined by Erbel (using the duction Doppler derived cardiac output German Schrittmacher syndrom) in 1979.2 It improved by 14% when pacing was changed can present with symptoms as severe as to DDD from VVI.8 syncope, presyncope, oedema, dyspnoea, and chest pain, or more moderately and subtly as lethargy, palpitation, or an awareness of Haemodynamics of pacemaker venous pulsation all of which may occur when syndrome there is atrial systole during ventricular sys- Contraction of the atria against closed atrio- tole. This is most frequent when there is ventricular valves during ventricular systole ventriculoatrial conduction from the paced leads to raised atrial pressures, loss of atrial ventricle to the atrium usually via the contribution to ventricular filling, and a con- atrioventricular node.34 The symptoms can be sequent fall in cardiac output which causes a identical to those prompting implant.5 fall in arterial pressure if the baroreceptor Occasionally pacemaker syndrome can occur mediated rise in systemic vascular resistance is in the absence of ventriculoatrial conduction insufficient.9 In a study on 20 open-chest dogs when ventricular pacing is in competition with experimental complete heart block left with sinus rhythm.6 atrial angiography showed retrograde blood flow into the pulmonary venous system at Incidence of pacemaker syndrome atrioventricular intervals of -50 and The incidence of pacemaker syndrome varies - 100 ms. -

Answer: E) Atrial Fibrillation with Complete Heart Block Teaching Point
Answer: e) Atrial fibrillation with complete heart block Teaching Point: A slow regular ventricular rate in a patient with concurrent atrial fibrillation, as seen in this ECG, is diagnostic of complete heart block. Atrial fibrillation creates a diagnostic dilemma for identifying AV nodal disease or block. Close scrutiny should be placed on R-R intervals to identify patterns or regularity (1). Clinicians should be wary of a regular heart rate in a patient with persistent atrial fibrillation, especially in those using digitalis. If an AV nodal block is identified, it may be transient, and a search for reversible causes is indicated as in all cases of complete heart block prior to pacemaker placement. Electrolyte abnormalities, ischemia, and medications remain the leading reversible causes (2,3). The patient in this case was transferred to the Emergency Department and admitted for further observation. Ischemia was ruled out. Carvedilol was held, and he was diuresed. He continued to demonstrate adequate chronotropic response with exertion. The complete heart block soon resolved, and he was diuresed to euvolemia. Pacemaker placement was deferred given the transient nature of the AV block in the context of recent beta-blocker usage. He was discharged home with continuous heart rhythm monitoring without any further evidence of complete heart block. References: 1. Urbach JR, Grauman JJ, Straus SH. Quantitative Methods for the Recognition of Atrioventricular Junctional Rhythms in Atrial Fibrillation. Circulation. 1969; 39: 803- 817. 2. Kojic EM, Hardarson T, Sigfusson N, Sigvaldason H. The prevalence and prognosis of third-degree atrioventricular conduction block: the Reykjavik study. J Intern Med. -

Update on the Diagnosis and Management of Familial Long QT Syndrome
Heart, Lung and Circulation (2016) 25, 769–776 POSITION STATEMENT 1443-9506/04/$36.00 http://dx.doi.org/10.1016/j.hlc.2016.01.020 Update on the Diagnosis and Management of Familial Long QT Syndrome Kathryn E Waddell-Smith, FRACP a,b, Jonathan R Skinner, FRACP, FCSANZ, FHRS, MD a,b*, members of the CSANZ Genetics Council Writing Group aGreen Lane Paediatric and Congenital Cardiac Services, Starship Children’s Hospital, Auckland New Zealand bDepartment[5_TD$IF] of Paediatrics,[6_TD$IF] Child[7_TD$IF] and[8_TD$IF] Youth[9_TD$IF] Health,[10_TD$IF] University of Auckland, Auckland, New Zealand Received 17 December 2015; accepted 20 January 2016; online published-ahead-of-print 5 March 2016 This update was reviewed by the CSANZ Continuing Education and Recertification Committee and ratified by the CSANZ board in August 2015. Since the CSANZ 2011 guidelines, adjunctive clinical tests have proven useful in the diagnosis of LQTS and are discussed in this update. Understanding of the diagnostic and risk stratifying role of LQTS genetics is also discussed. At least 14 LQTS genes are now thought to be responsible for the disease. High-risk individuals may have multiple mutations, large gene rearrangements, C-loop mutations in KCNQ1, transmembrane mutations in KCNH2, or have certain gene modifiers present, particularly NOS1AP polymorphisms. In regards to treatment, nadolol is preferred, particularly for long QT type 2, and short acting metoprolol should not be used. Thoracoscopic left cardiac sympathectomy is valuable in those who cannot adhere to beta blocker therapy, particularly in long QT type 1. Indications for ICD therapies have been refined; and a primary indication for ICD in post-pubertal females with long QT type 2 and a very long QT interval is emerging. -

Heart and Circulatory System?Arrhythmia (Irregular
Heart and Circulatory System?Arrhythmia (Irregular Heartbeat) Cardiac arrhythmias have a wide range of clinical significance, depending upon the type, location of origin, symptoms present, and the likelihood for sudden or subtle incapacitation. Arrhythmias that originate in the upper chambers of the heart, the atria, are referred to as "supraventricular" arrhythmias. The atria are the heart's pacemakers and also act as primers for the pump chambers, the ventricles. The most common atrial arrhythmia is atrial fibrillation, which is a rapid, irregular rhythm that can result in dizziness, shortness of breath, or loss of consciousness if the heart rate is too slow or fast. Ventricular arrhythmias affect the lower pump chambers, the ventricles. Common ventricular arrhythmias include premature ventricular contractions (PVCs). These are fairly common in healthy people and can be brought on by a number of stimuli, including excessive caffeine consumption or stress. Ventricular tachycardia is a rapid heart rate with sudden onset. Symptoms of ventricular tachycardia include lightheadedness, fainting, weakness, or mental confusion. This type of arrhythmia is often associated with underlying heart disease and requires good medical management. The FAA issues medical certificates for many types of arrhythmias. Atrial fibrillation, atrial flutter, or ventricular/supraventricular arrhythmias that are not associated with underlying ischemic heart disease, cardiomyopathy (a disease of the heart muscle), or significant heart valve defect or outflow tract obstructions may be favorably considered for issuance of any class of medical certificate. Premature Ventricular Contractions (PVCs) If there is a history of PVCs occurring at a rate of more than six per minute on a resting electrocardiogram, or that have caused symptoms, the FAA will require a cardiovascular evaluation, including a 24hour Holter monitor and graded exercise treadmill test. -

What Is Atrial Fibrillation?
ANSWERS Cardiovascular Conditions by heart What Is Atrial Fibrillation? Normally, your heart contracts and relaxes to a regular beat. Certain cells in your heart, called the sinus node, make electrical The illustrations above show normal conduction and contraction. signals that cause the heart to contract and pump blood. These electrical signals can be recorded using an electrocardiogram, or Sinus node ECG. Your doctor can read your ECG to find out if the electrical signals are normal. Left atrium In atrial fibrillation, or AFib, the heart’s Right atrium two small upper chambers (atria) beat irregularly and too fast, quivering instead of contracting properly. With atrial fibrillation, random electrical activity During AFib, some blood may not be interrupts the normal pumped efficiently from the atria into the conduction rhythm. ventricles. Blood that’s left behind can pool This prevents the atria from in the atria and form blood clots. properly contracting. How do I know I have atrial fibrillation? The risk of stroke is about five times higher in people with AFib. This is because blood can pool in the atria and blood Some people with AFib don’t have symptoms. Some of the clots can form. symptoms are: • Fast, irregular heartbeat What can be done to correct AFib? • Heart palpitations (rapid “flopping” or “fluttering” feeling in the chest) Treatment options may include one or more of the following: • Feeling lightheaded or faint • Medication to help slow your heart rate, such as beta • Chest pain or pressure blockers, certain calcium channel blockers or digoxin • Shortness of breath, especially when lying down • Medication to restore normal heart rhythm, such as • Tiring more easily (fatigue) beta blockers or antiarrhythmics • Procedures to stop or control the electrical impulses Can AFib lead to other problems? causing the AFib, such as electrical cardioversion or catheter ablation You can live with and manage AFib. -
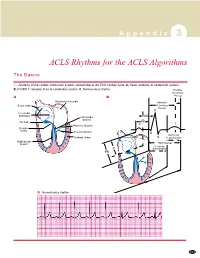
ACLS Rhythms for the ACLS Algorithms
A p p e n d i x 3 ACLS Rhythms for the ACLS Algorithms The Basics 1. Anatomy of the cardiac conduction system: relationship to the ECG cardiac cycle. A, Heart: anatomy of conduction system. B, P-QRS-T complex: lines to conduction system. C, Normal sinus rhythm. Relative Refractory A B Period Bachmann’s bundle Absolute Sinus node Refractory Period R Internodal pathways Left bundle AVN branch AV node PR T Posterior division P Bundle of His Anterior division Q Ventricular Purkinje fibers S Repolarization Right bundle branch QT Interval Ventricular P Depolarization PR C Normal sinus rhythm 253 A p p e n d i x 3 The Cardiac Arrest Rhythms 2. Ventricular Fibrillation/Pulseless Ventricular Tachycardia Pathophysiology ■ Ventricles consist of areas of normal myocardium alternating with areas of ischemic, injured, or infarcted myocardium, leading to chaotic pattern of ventricular depolarization Defining Criteria per ECG ■ Rate/QRS complex: unable to determine; no recognizable P, QRS, or T waves ■ Rhythm: indeterminate; pattern of sharp up (peak) and down (trough) deflections ■ Amplitude: measured from peak-to-trough; often used subjectively to describe VF as fine (peak-to- trough 2 to <5 mm), medium-moderate (5 to <10 mm), coarse (10 to <15 mm), very coarse (>15 mm) Clinical Manifestations ■ Pulse disappears with onset of VF ■ Collapse, unconsciousness ■ Agonal breaths ➔ apnea in <5 min ■ Onset of reversible death Common Etiologies ■ Acute coronary syndromes leading to ischemic areas of myocardium ■ Stable-to-unstable VT, untreated ■ PVCs with -

Atrial Fibrillation: Diagnosis and Treatment CECILIA GUTIERREZ, MD, and DANIEL G
Atrial Fibrillation: Diagnosis and Treatment CECILIA GUTIERREZ, MD, and DANIEL G. BLANCHARD, MD, University of California, San Diego, La Jolla, California Atrial fibrillation is the most common cardiac arrhythmia. It impairs cardiac function and increases the risk of stroke. The incidence of atrial fibrillation increases with age. Key treatment issues include deciding when to restore normal sinus rhythm, when to control rate only, and how to prevent thromboembolism. Rate control is the preferred manage- ment option in most patients. Rhythm control is an option for patients in whom rate control cannot be achieved or who have persistent symptoms despite rate control. The current recommendation for strict rate control is a resting heart rate of less than 80 beats per minute. However, one study has shown that more lenient rate control of less than 110 beats per minute while at rest was not inferior to strict rate control in preventing cardiac death, heart failure, stroke, and life- threatening arrhythmias. Anticoagulation therapy is needed with rate control and rhythm control to prevent stroke. Warfarin is superior to aspirin and clopidogrel in preventing stroke despite its narrow therapeutic range and increased risk of bleeding. Tools that predict the risk of stroke (e.g., CHADS2) and the risk of bleeding (e.g., Outpatient Bleed- ing Risk Index) are helpful in making decisions about anticoagulation therapy. Surgical options for atrial fibrillation include disruption of abnormal conduction pathways in the atria, and obliteration of the left atrial appendage. Catheter ablation is an option for restoring normal sinus rhythm in patients with paroxysmal atrial fibrillation and normal left atrial size.