Spontaneous Abortion
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Supplement of Hydrol
Supplement of Hydrol. Earth Syst. Sci., 25, 957–982, 2021 https://doi.org/10.5194/hess-25-957-2021-supplement © Author(s) 2021. This work is distributed under the Creative Commons Attribution 4.0 License. Supplement of Learning from satellite observations: increased understanding of catchment processes through stepwise model improvement Petra Hulsman et al. Correspondence to: Petra Hulsman ([email protected]) The copyright of individual parts of the supplement might differ from the CC BY 4.0 License. Supplements S1. Model performance with respect to all discharge signatures ............................................... 2 S2. Parameter sets selected based on discharge ......................................................................... 3 S2.1 Time series: Discharge ............................................................................................................................... 3 S2.2. Time series: Evaporation (Basin average) ................................................................................................. 4 S2.3 Time series: Evaporation (Wetland dominated areas) ................................................................................ 5 S2.4 Time series: Total water storage (Basin average) ....................................................................................... 6 S2.5. Spatial pattern: Evaporation (normalised, dry season) .............................................................................. 7 S2.6. Spatial pattern: Total water storage (normalised, dry season) .................................................................. -

Report on 'Er' Viewers Who Saw the Smallpox Episode
Working Papers Project on the Public and Biological Security Harvard School of Public Health 4. REPORT ON ‘ER’ VIEWERS WHO SAW THE SMALLPOX EPISODE Robert J. Blendon, Harvard School of Public Health, Project Director John M. Benson, Harvard School of Public Health Catherine M. DesRoches, Harvard School of Public Health Melissa J. Herrmann, ICR/International Communications Research June 13, 2002 After "ER" Smallpox Episode, Fewer "ER" Viewers Report They Would Go to Emergency Room If They Had Symptoms of the Disease Viewers More Likely to Know About the Importance of Smallpox Vaccination For Immediate Release: Thursday, June 13, 2002 BOSTON, MA – Regular "ER" viewers who saw or knew about that television show's May 16, 2002, smallpox episode were less likely to say that they would go to a hospital emergency room if they had symptoms of what they thought was smallpox than were regular "ER" viewers questioned before the show. In a survey by the Harvard School of Public Health and Robert Wood Johnson Foundation, 71% of the 261 regular "ER" viewers interviewed during the week before the episode said they would go to a hospital emergency room. A separate HSPH/RWJF survey conducted after the episode found that a significantly smaller proportion (59%) of the 146 regular "ER" viewers who had seen the episode, or had heard, read, or talked about it, would go to an emergency in this circumstance. This difference may reflect the pandemonium that broke out in the fictional emergency room when the suspected smallpox cases were first seen. Regular "ER" viewers who saw or knew about the smallpox episode were also less likely (19% to 30%) than regular "ER" viewers interviewed before the show to believe that their local hospital emergency room was very prepared to diagnose and treat smallpox. -

2009 TV Land Awards' on Sunday, April 19Th
Legendary Medical Drama 'ER' to Receive the Icon Award at the '2009 TV Land Awards' on Sunday, April 19th Cast Members Alex Kingston, Anthony Edwards, Linda Cardellini, Ellen Crawford, Laura Innes, Kellie Martin, Mekhi Phifer, Parminder Nagra, Shane West and Yvette Freeman Among the Stars to Accept Award LOS ANGELES, April 8 -- Medical drama "ER" has been added as an honoree at the "2009 TV Land Awards," it was announced today. The two-hour show, hosted by Neil Patrick Harris ("How I Met Your Mother," Harold and Kumar Go To White Castle and Assassins), will tape on Sunday, April 19th at the Gibson Amphitheatre in Universal City and will air on TV Land during a special presentation of TV Land PRIME on Sunday, April 26th at 8PM ET/PT. "ER," one of television's longest running dramas, will be presented with the Icon Award for the way that it changed television with its fast-paced steadi-cam shots as well as for its amazing and gritty storylines. The Icon Award is presented to a television program with immeasurable fame and longevity. The show transcends generations and is recognized by peers and fans around the world. As one poignant quiet moment flowed to a heart-stopping rescue and back, "ER" continued to thrill its audiences through the finale on April 2, which bowed with a record number 16 million viewers. Cast members Alex Kingston, Anthony Edwards, Linda Cardellini, Ellen Crawford, Laura Innes, Kellie Martin, Mekhi Phifer, Parminder Nagra, Shane West and Yvette Freeman will all be in attendance to accept the award. -

The Criminal Justice and Community Response to Rape
If you have issues viewing or accessing this file contact us at NCJRS.gov. .-; .( '\ U.S. Department of Justice Office of Justice Programs National Institute of Justice The Criminal Justice and Community Response to Rape • About the National Institute of Justice The National Institute of Justice (NiJ), a component of the The research and development program that resulted in Office of Justice Programs, is the research and development the creation of police body armor that has meant the agency of the U.S. Department of Justice. NIJ was estab difference between life and death to hundreds of police lished to prevent and reduce crime and to improve the officers. criminal justice system. Specific mandates established by Congress in the Omnibus Crime Control and Safe Streets Act Pioneering scientific advances such as the research and of 1968, as amended, and the Anti-Drug Abuse Act of 1988 development of DNA analysis to positively identify direct the National Institute of Justice to: suspects and eliminate the innocent from suspicion. Sponsor special projects, and research and develop The evaluation of innovative justice programs to deter ment programs that will improve and strengthen the mine what works, including drug enforcement, commu criminal justice system and reduce or prevent crime. nity policing, community anti-drug initiatives, prosecu tion of complex drug cases, drug testing throughout the Conduct national demonstration projects that employ criminal justice system, and user accountability pro f I innovative or promising approaches for improving crimi grams. nal justice. Creation of a corrections information-sharing system Develop new technologies to fight crime and improve that enables State and local officials to exchange more criminal justice. -

Upcoming Promotions Upcoming Games Record
GWINNETT STRIPERS (23-26, 4th in SE, 9.0 GB) at DURHAM BULLS (32-17, 1st in SE, 0.5 GA) Thursday, July 1, 2021 • 6:35 PM • Durham Bulls Athletic Park, Durham, NC • Game #50 of 120 • Road Game #27 GWN: RHP Kyle Wright (1-2, 3.76 ERA) vs. DUR: LHP Dietrich Enns (2-1, 3.27 ERA) STRIPERS MEDIA RELATIONS: Dave Lezotte ([email protected]), Collin Perry ([email protected]) TWITTER: @GoStripers MEDIA CENTER: GoStripers.com/Media TONIGHT: The Stripers continue a 12-game, 13-day road KAZ CLIMBING CAREER LISTS: Over eight seasons with LAST GAME (6/30) trip with game three of a six-game series vs. the Durham Gwinnett dating back to 2013, Sean Kazmar Jr. is batting STREAKS F/9 (2:34) R H E Bulls (Tampa Bay Rays) at Durham Bulls Athletic Park. It is .266 (638-for-2,402, 131 2B, 12 3B, 41 HR, 290 R, 284 RBI, Current Streak: W1 Gwinnett 2 5 0 the third of 12 meetings between the two longtime division 24 SB) in 700 games. He holds Gwinnett career records for Last 10 Games: 3-7 Durham 1 5 0 rivals this season (6 home, 6 road). With a win, Gwinnett games, at-bats, hits, total bases (916), doubles, runs, and Long Winning Streak: W: D. Lee (2-0) would have back-to-back victories for the first time since RBI. “Kaz” is also just 19 hits shy of tying the Atlanta Braves 4G (2x, last: 5/25-5/28) 1.0 IP, 1 H, 1 ER, 0 BB, 1 SO 6/15-6/16 vs. -
The Script, Vol. 01 No. 25, January 04, 1947
University of Central Florida STARS The Script Newspapers and Weeklies of Central Florida 1-4-1947 The Script, Vol. 01 No. 25, January 04, 1947 The Script Find similar works at: https://stars.library.ucf.edu/cfm-thescript University of Central Florida Libraries http://library.ucf.edu This Newspaper is brought to you for free and open access by the Newspapers and Weeklies of Central Florida at STARS. It has been accepted for inclusion in The Script by an authorized administrator of STARS. For more information, please contact [email protected]. STARS Citation The Script, "The Script, Vol. 01 No. 25, January 04, 1947" (1947). The Script. 24. https://stars.library.ucf.edu/cfm-thescript/24 Saturday 10c Per Copy JAN. 4, 1947 THE SCRIPT Brevard County's Only Colored Newspaper Elmer Silas, Publisher VOL. 1, NO. 25 COCOA, FLORIDA Dorothy Sweetwine, Editor Local Girl Will Emancipation Program Is Mrs. Lucy Knight Speak For Elks Held At Mt. Moriah Church Visitor In Cocoa Miss Annie Laura Jones, daugh Emancipation Program MRS LUCK KNIGHT ter of Mr. and Mrs. Osborne To Conduct Revival Here Mrs. Lucy Knight, who has re Jones, was chosen in a recent Held at Mt. Moriah sided in New York City for the meeting of the local lodge of Elks The Brevard County Branch of past ten years, arrived here on to represent Indian River Lodge the NAACP was the sponsors of Christmas day, practically sur No. 692 LB.P.O.E. of W., in the the Emancipation day program, prising her parents, Mr. and Mrs. annual oratorical contest. -

Di Scovery Channel Jul Y Schedul E ( 2021)
Di scover y Channel Jul y Schedul e ( 2021) MONDAY TUESDAY WEDNESDAY THURSDAY FRI DAY SATURDAY SUNDAY 6/28 6/29 6/30 7/1 7/2 7/3 7/4 4: 00 Through The Wor mhol e Wit h Wheeler Deal er s ( Season 14) : br oadcast cancel ed ★Steel Buddi es ( Season 7) : Naked And Afraid (Season 6): How The Uni ver se Wor ks World's Top 5 (Season 2): 4: 00 Mor gan Fr eeman ( Season 7) : 1969 Opel Gt 1900 Epi sode 11 Dont Cave I n (Season 9): War Of The Gi ant Ai r cr af t What Makes A Terr or i st ? Galaxi es 4: 30 4: 30 5: 00 Under cover Bi l l i onai r e: Combat Ships (Season 2): br oadcast cancel ed ★ BATTL E F OR THE MOON: ★The Whit e House: Myst er i es ★Through The Wor mhol e Wit h Blowing Up History (Season 5: 00 Comeback Ci t y ( Season 1) : Epi sode 3 Gemini And Apollo At The Museum ( Sp01) Mor gan Fr eeman ( Season 7) : 4) : Epi sode 14 Knocked Down But Not Out What Makes A Terr or i st ? 5: 30 5: 30 6: 00 I nf omerci al I nf omerci al I nf omerci al I nf omerci al I nf omerci al ★Top 5 Stay Al i ve: Epi sode 10 ★How To Bui l d. Ever yt hi ng: 6: 00 I nsi de a Jet Car 6: 30 How It's Made Dream Cars S3: How It's Made Dream Cars S3: How It's Made Dream Cars S3: ★How It's Made Dream Cars S3: BMW ★How It's Made Dream Cars S3: I nf omerci al I nf omerci al 6: 30 Ultima Evolution Ferrari Cali fornia T Jaguar Xf M6 Rol l s-Royce Dawn 7: 00 Wheeler Deal er s ( Season 12) : Wheeler Deal er s ( Season 12) : Wheeler Deal er s ( Season 12) : ★Wheeler Deal er s ( Season ★Wheeler Deal er s ( Season Naked And Afraid (Season 6): How I t ' s Made ( Season 16) : -

The Rape of Emergency Medicine
The Rape of Emergency Medicine James Keaney, M.D. © 2004 by the American Academy of Emergency Medicine Table of Contents Prologue..............................................................................1 Chapter One: Steinerman................................................. 8 Chapter Two: The Contracts and Their Holders ....... 13 Chapter Three: Suits and Scrubs....................................25 Chapter Four: Origin of a Species..................................45 Chapter Five: Crips and Bloods......................................54 Chapter Six: The Anderson Syndrome .......................... 62 Chapter Seven: Caveat Emptor .......................................82 Chapter Eight: Cro-Magnon ......................................... 99 Chapter Nine: The Quiet Room.................................... 108 Chapter Ten: The Other Side of Midnight ................ 126 Chapter Eleven: A One Way Ticket to Palookaville . 142 Chapter Twelve: Utah ................................................... 154 Chapter Thirteen: Pinnacle, Inc. .................................167 Chapter Fourteen: The Missing Chapter .................... 187 Chapter Fifteen: Chart Wars ....................................... 188 Chapter Sixteen: Physicians of a Lesser God ............. 200 Chapter Seventeen: Mea Culpa..................................... 214 Chapter Eighteen: California Dreamin’......................220 Chapter Nineteen: The Empire Strikes Back...............237 Chapter Twenty: The One Hundred and Eighty Thousand Dollar Pair of Sunglasses ...........................246 -
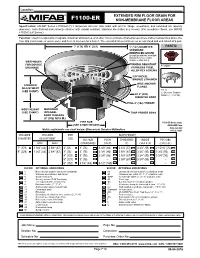
F1100-Er Non-Membrane Floor Areas
Location: ® EXTENDED RIM FLOOR DRAIN FOR F1100-ER NON-MEMBRANE FLOOR AREAS Specification: MIFAB® Series F1100-ER-(*)-1 lacquered cast iron floor drain with anchor flange, weepholes, and extended rim (specify diameter), satin finished nickel bronze strainer with vandal resistant, stainless steel allen key screws. (For membrane floors, use MIFAB F1100-C-ER Series.) Function: Used in restaurants, hospitals, industrial laboratories, and other non-membrane finished areas where indirect waste lines above the floor drip condensate or waste water and there is no room for a funnel. The extended rim permits use as an anti-flood and anti splash drip pan. 7" (178) OR 9" (229) 5" (127) DIAMETER PARTS: STANDARD REINFOCED GRATE (Compliant with the 2010 ADA Standards for accessible design, section 302.3) WEEPHOLES FOR DOUBLE VANDAL RESISTANT A1 BODY DRAINAGE STAINLESS STEEL ALLEN KEY SCREWS "ER" NICKEL BRONZE STRAINER WIDE ANCHOR STRAINER FLANGE ADJUSTMENT ER-(*) (SEE CHART) (*) Denotes Strainer A1 8" (203) Finish (-1, -3 or 50) DIAMETER BODY FULL 4" (102) THROAT BODY HEIGHT MACHINED (SEE CHART) INTEGRAL TRAP PRIMER BOSS BODY THREADS (4" (102) N.P.S.M.) PIPE SIZE F1100-ER Series meets (SEE CHART BELOW) Metric equivalents see chart below. (Dimension) Denotes Millimetres drain standard A112.6.3-2001 STRAINER STRAINER PIPE BODY HEIGHT DIAMETER ADJUSTMENT SIZE NO HUB PUSH THREADED INSIDE PVC/ABS MIN MAX (STANDARD) ON (P) (T) CAULK (X) (-30)/(-31) 7" (178) 1 3/4" (44) 2 5/8" (67) 2" (51) 3” (76) 3 3/8” (86) 2 1/4” (57) 3 3/4” (95) 2 15/16” (75) 9" (229) 1 -

Cast Bios NANCY GRACE
‘HAILEY DEAN MYSTERY: DATING IS MURDER’ Cast Bios NANCY GRACE – An outspoken, tireless advocate for victims’ rights and one of television's most respected legal analysts, Nancy Grace is the powerful force behind CNN Headline News’ (HLN) top-rated “Nancy Grace.” A former prosecutor with an unparalleled record of success, she has appeared on “The Oprah Winfrey Show,” “The View,” “The Today Show,” “Good Morning America,” “Dr. Phil” and “Larry King Live,” among others, dispensing her firebrand take on the modern justice system. In addition, she was a highlight and fan favorite of “Dancing with the Stars,” finishing Season 13 in the competition’s coveted Top 5. All of her earnings from the show went to support the National Center for Missing and Exploited Children. In 2011, Grace was named one of the most impactful and powerful women in entertainment by both leading industry trade magazines, Variety and The Hollywood Reporter. Beginning earlier this year, she has hosted a daily podcast called “Crime Stories with Nancy Grace.” Grace’s first book, Objection! was published in 2005, and became an instant New York Times bestseller. Her two subsequent novels, The Eleventh Victim (2009) and Death on the D-List (2010), were also New York Times bestsellers. She is the recipient of several American Women in Radio & Television Gracie Awards for her “Nancy Grace Investigates” primetime report on Court TV and has been awarded the Individual Achievement/Best Program Host honor. Grace has also been widely recognized by many notable organizations (including the Carole Sund/Carrington Foundation, Crime Victims United of California and The Retreat) for her advocacy work on behalf of victims’ rights. -

TV Doctors Fieldwork Dates: 12Th - 13Th March 2019
TV Doctors Fieldwork Dates: 12th - 13th March 2019 Conducted by YouGov On behalf of YouGov Omnibus © YouGov plc 2019 BACKGROUND This spreadsheet contains survey data collected and analysed by YouGov plc. No information contained within this spreadsheet may be published without the consent of YouGov Plc and the client named on the front cover. Methodology: This survey has been conducted using an online interview administered to members of the YouGov Plc panel of 1.2 million individuals who have agreed to take part in surveys. Emails are sent to panellists selected at random from the base sample. The e-mail invites them to take part in a survey and provides a generic survey link. Once a panel member clicks on the link they are sent to the survey that they are most required for, according to the sample definition and quotas. (The sample definition could be "US adult population" or a subset such as "US adult females"). Invitations to surveys don’t expire and respondents can be sent to any available survey. The responding sample is weighted to the profile of the sample definition to provide a representative reporting sample. The profile is normally derived from census data or, if not available from the census, from industry accepted data. YouGov plc make every effort to provide representative information. All results are based on a sample and are therefore subject to statistical errors normally associated with sample-based information. For further information about the results in this spreadsheet, please contact YouGov Plc +1 888.729.0773 or email [email protected] quoting the survey details EDITOR'S NOTES - all press releases should contain the followinG information All figures, unless otherwise stated, are from YouGov Plc. -

I Am a Canadian Doctor
Humour and Humanity combat. I had him, and he had me. My speech and ataxia that I intended. I grinned weakly, confidence in my left index finger was deep in his chest, This stunning assault on his pleural “balls” somewhat shaken. and his right fist clutched my ability to space caused him to release my Later, back in the trauma room, one sire future generations. It was Capulet nightlife. I disengaged and sewed him of the nurses approached, jabbed the and Montague, St. George and the up in a flash, all the while resisting the trauma flow-sheet at me and said, “Dr. Dragon, Ralph Klein and the Canada desperate urge to drop everything and Huber, would you mind putting your Health Act. All this flashed by in the rush to the loo to inspect the damage. John Henry on this?” instant that it took my own pain im- When I finally slunk out, I bumped She probably never understood why pulses to traverse the pudendal nerves into the SSR (grinning like an idiot) I panicked and ran. You see, in New and reach my brain. and one of the attendings, who’d seen Zealand, “John Henry” refers not to a I screamed. “You trucker!” (or words the whole thing — or thought he had. man’s signature, but to his . to that effect). Then I rammed the tube “Well, Huber,” he chuckled, “you Since then, I’ve done many chest toward his cerebellum, by way of the finally did it. That was the fastest tubes, but none as slick as that first one.