Phytochemical Characterization of Tabernanthe
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Rhazya Stricta S
IENCE SC • VTT VTT S CIENCE • T S E Alkaloids of in vitro cultures of N C O H I N Rhazya stricta S O I V Dis s e r ta tion L • O S 93 G Rhazya stricta Decne. (Apocynaceae) is a traditional medicinal T Y H • R plant in Middle East and South Asia. It contains a large number of G I E L S H 93 E G terpenoid indole alkaloids (TIAs), some of which possess A I R H C interesting pharmacological properties. This study was focused on H biotechnological production tools of R. stricta, namely undifferentiated cell cultures, and an Agrobacterium rhizogenes- mediated transformation method to obtain hairy roots expressing heterologous genes from the early TIA pathway. Rha zya alkaloids comprise a wide range of structures and polarities, therefore, many A analytical methods were developed to investigate the alkaloid l k contents in in vitro cultures. Targeted and non-targeted analyses a l o were carried out using gas chromatography-mass spectrometry i d (GC-MS), high performance liquid chromatography (HPLC), ultra s o performance liquid chromatography-mass spectrometry (UPLC- f i MS) and nuclear magnetic resonance (NMR) spectroscopy. n Calli derived from stems contained elevated levels of v i t r strictosidine lactam compared to other in vitro cultures. It o was revealed that only leaves were susceptible to Agrobacterium c u infection and subsequent root induction. The transformation l t u efficiency varied from 22% to 83% depending on the gene. A total r e of 17 TIAs were identified from hairy root extracts by UPLC-MS. -

A Review on Tabernaemontana Spp.: Multipotential Medicinal Plant
Online - 2455-3891 Vol 11, Issue 5, 2018 Print - 0974-2441 Review Article A REVIEW ON TABERNAEMONTANA SPP.: MULTIPOTENTIAL MEDICINAL PLANT ANAN ATHIPORNCHAI* Department of Chemistry and Center of Excellence for Innovation in Chemistry, Faculty of Science, Burapha University, Bangsaen, Chonburi 20131 Thailand. Email: [email protected] Received: 01 March 2016, Revised and Accepted: 29 January 2018 ABSTRACT Plants in the genus Tabernaemontana have been using in Thai and Chinese traditional medicine for the treatment several diseases. The great majority constituents of Tabernaemontana species have already been subjected to isolation and identification of monoterpene indole alkaloids present in their several parts. Many of monoterpene indole alkaloids exhibited a wide array of several activities. The biogenesis, classification, and biological activities of these alkaloids which found in Tabernaemontana plants were discussed in this review and its brings the research up-to-date on the bioactive compounds produced by Tabernaemontana species, directly or indirectly related to human health. Keywords: Tabernaemontana plants, Phytochemistry, Biogenesis, Terpene indole alkaloids, Biological activities. © 2018 The Authors. Published by Innovare Academic Sciences Pvt Ltd. This is an open access article under the CC BY license (http://creativecommons. org/licenses/by/4. 0/) DOI: http://dx.doi.org/10.22159/ajpcr.2018.v11i5.11478 INTRODUCTION alkaloids are investigated. All monoterpene indole alkaloids are derived from aromatic amino acid tryptophan and the iridoid terpene Several already drugs were discovered from the natural products. secologanin (Scheme 1). Tryptophan converts to tryptamine using Especially, the treatments of infectious diseases and oncology have tryptophan decarboxylase which is a pyridoxal-dependent enzyme. benefited from numerous drugs which were found in natural product The specific iridoid precursor was subsequently identified as sources. -
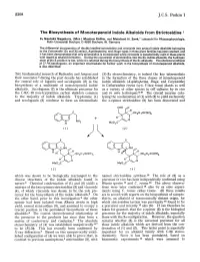
J.C.S. Perkin I
2308 J.C.S. Perkin I The Biosynthesis of Monoterpenoid lndole Alkaloids from Strictosidine By Naotaka Nagakura, (Mrs.) Martin8 Ruffer, and Meinhart H. Zenk," Lehrstuhl fur Pflanzenphysiologie, Ruhr-Universitat Bochum, D 4630 Bochum, W. Germany The differential incorporation of doubly labelled strictosidine and vincoside into several indole alkaloids belonging to the Corynanthe (3a and 3p series), Aspidosperma, and lboga types in three plant families has been studied, and it has been demonstrated that only strictosidine is incorporated while vincoside is metabolically inert in these plants with regard to alkaloid formation. During the conversion of strictosidine into the 3P-indole alkaloids, the hydrogen atom at the 3-position is lost, while it is retained during the biosynthesis of the 32 alkaloids. The chemical synthesis of [7-3H]secologanin, an important intermediate for further work in the biosynthesis of monoterpenoid alkaloids, is also described. THEfundamental research of Battersby and Arigoni and (S)-3a stereochemistry, is indeed the key intermediate their associates during the past decade has established in the formation of the three classes of monoterpenoid the central role of loganin and secologanin (2) in the indole alkaloids (Asfiidosfierma, Iboga, and Corynanthe) biosynthesis of a multitude of monoterpenoid indole in Catharanthus roseus (syn. Vinca rosea) plants as well alkaloids. Secologanin (2) is the ultimate precursor for as a variety of other species in cell cultures by in vivo the C-9/C-10 non-tryptamine carbon skeleton -

Cartografiando Un Camino Para La Iboga
CARTOGRAFIANDO UN CAMINO PARA LA IBOGA Iboga Community Engagement Initiative CONCLUSIONES Y RECOMENDACIONES Marzo 2021 Un proyecto de International Center for Ethnobotanical Education, Research and Service (ICEERS) Dirección del proyecto Ricard Faura, PhD Andrea Langlois Asesoramiento científico, legal y técnico en ICEERS Benjamin De Loenen, Dr. José Carlos Bouso, Genís Ona Edición Igor Domsac Fotografía Ricard Faura Diseño gráfico Àlex Verdaguer Marzo de 2021 Para más información o consultas, por favor envíe un correo electrónico a: [email protected] www.iceers.org CARTOGRAFIANDO UN CAMINO PARA LA IBOGA Iboga Community Engagement Initiative CONCLUSIONES Y RECOMENDACIONES CONTENIDOS Conclusiones y recomendaciones 5 Introducción 7 Breve contexto: de África al mundo 9 La Iniciativa de Compromiso 10 Cómo abordar este informe 11 Agradecimientos 11 A: Comunidad, reciprocidad y curación global 14 Conclusiones 14 Recomendaciones 16 B: Regeneración biocultural y sostenibilidad 23 Conclusiones 23 Recomendaciones 27 C: Reconocimiento y evolución de los enfoques curativos tradicionales y nuevos 31 Conclusiones 31 Recomendaciones 34 Notas 38 Conclusiones y recomendaciones 5 Conclusiones y recomendaciones A: Comunidad, reciprocidad y curación global Conclusiones » Las comunidades internacionales de la iboga y de la ibogaína se beneficiarían de una mayor interconexión, comunicación y colaboración para aumentar los esfuerzos de sostenibilidad y fomentar mayores oportunidades de curación humana y planetaria. » El actual ecosistema global de la iboga está -

Fall TNP Herbals.Pptx
8/18/14 Introduc?on to Objecves Herbal Medicine ● Discuss history and role of psychedelic herbs Part II: Psychedelics, in medicine and illness. Legal Highs, and ● List herbs used as emerging legal and illicit Herbal Poisons drugs of abuse. ● Associate main plant and fungal families with Jason Schoneman RN, MS, AGCNS-BC representave poisonous compounds. The University of Texas at Aus?n ● Discuss clinical management of main toxic Schultes et al., 1992 compounds. Psychedelics Sacraments: spiritual tools or sacred medicine by non-Western cultures vs. Dangerous drugs of abuse vs. Research and clinical tools for mental and physical http://waynesword.palomar.edu/ww0703.htm disorders History History ● Shamanic divinaon ○ S;mulus for spirituality/religion http://orderofthesacredspiral.blogspot.com/2012/06/t- mckenna-on-psilocybin.html http://www.cosmicelk.net/Chukchidirections.htm 1 8/18/14 History History http://www.10zenmonkeys.com/2007/01/10/hallucinogenic- weapons-the-other-chemical-warfare/ http://rebloggy.com/post/love-music-hippie-psychedelic- woodstock http://fineartamerica.com/featured/misterio-profundo-pablo- amaringo.html History ● Psychotherapy ○ 20th century: un;l 1971 ● Recreaonal ○ S;mulus of U.S. cultural revolu;on http://qsciences.digi-info-broker.com http://www.uspharmacist.com/content/d/feature/c/38031/ http://en.wikipedia.org/nervous_system 2 8/18/14 Main Groups Main Groups Tryptamines LSD, Psilocybin, DMT, Ibogaine Other Ayahuasca, Fly agaric Phenethylamines MDMA, Mescaline, Myristicin Pseudo-hallucinogen Cannabis Dissociative -
Biosynthesis by in Situ Hybridization (ISH)
Localization of monoterpenoid indole alkaloid (MIA) biosynthesis by in situ hybridization (ISH) By Elizabeth Edmunds, Hons. B.Sc. A Thesis Submitted to the Department of Biotechnology In partial fulfillment of the requirements For the degree of Masters of Science August, 2012 Brock University St. Catha rines, Ontario ©Elizabeth Edmunds, 2012 ii Acknowledgments First and foremost I would like to thank Dr. Vincenzo Deluca for the opportunity to work in his laboratory under his mentorship. I have appreciated the helpful insight that has guided me through the course of this project. I have gained a valuable experience being able to learn from such an established and knowledgeable researcher. Secondly, I would like to thank my committee members Dr. Jeffrey Atkinson and Dr. Heather Gordon for their support and advice and their time to serve on my advisory committee. Thirdly, I would like to thank my colleagues and co-workers for their patience and helpful advice throughout my project. Particular mention must be given to Dr. Carlone's lab for their assistance and insight into in situ hybridization techniques. Finally, I would like to express my sincerest gratitude and appreciation towards my family and friends for their support. I would not be where I am today without the support and love from my mother and father, as well as Craig Easton. iii Abstract Monoterpenoid indole alkaloids (MIA) are among the largest and most complex group of nitrogen containing secondary metabolites that are characteristic of the Apocynaceae plant family including the most notable Catharanthus roseus. These compounds have demonstrated activity as successful drugs for treating various cancers, neurological disorders and cardiovascular conditions. -

BOARD MEETING AGENDA Meeting Location: Portland State Office Building 800 NE Oregon Street, Portland, OR 97232 June 6-7, 2018 Updated 6.4.18
Oregon Board of Pharmacy BOARD MEETING AGENDA Meeting Location: Portland State Office Building 800 NE Oregon Street, Portland, OR 97232 June 6-7, 2018 Updated 6.4.18 The mission of the Oregon State Board of Pharmacy is to promote, preserve and protect the public health, safety and welfare by ensuring high standards in the practice of pharmacy and by regulating the quality, manufacture, sale and distribution of drugs. Wednesday, June 6, 2018 @ 8:30AM – Conference Rm A Thursday, June 7, 2018 @ 8:30AM – Conference Room A ≈ If special accommodations are needed for you to attend or participate in this Board Meeting, please contact Loretta Glenn at: (971) 673-0001. ≈ WEDNESDAY, JUNE 6, 2018 I. 8:30AM OPEN SESSION, Penny Reher, R.Ph, Presiding A. Roll Call B. Agenda Review and Approval Action Necessary II. Contested Case Deliberation pursuant to ORS 192.690(1) - Not Open to the Public III. EXECUTIVE SESSION – NOT OPEN TO THE PUBLIC, pursuant to ORS 676.175, ORS 192.660 (1) (2) (f) (k). A. Items for Consideration and Discussion: 1. Deliberation on Disciplinary Cases and Investigations 2. Personal Appearances 3. Deficiency Notifications 4. Case Review B. Employee Performance Review pursuant to ORS 192.660(2)(i). IV. OPEN SESSION - PUBLIC MAY ATTEND - At the conclusion of Executive Session, the Board may convene Open Session to begin some of the following scheduled agenda items - time permitting at approximately 3:30PM. V. Approve Consent Agenda* Action Necessary *Items listed under the consent agenda are considered to be routine agency matters and will be approved by a single motion of the Board without separate discussion. -

Phylogeny and Systematics of the Rauvolfioideae
PHYLOGENY AND SYSTEMATICS Andre´ O. Simo˜es,2 Tatyana Livshultz,3 Elena OF THE RAUVOLFIOIDEAE Conti,2 and Mary E. Endress2 (APOCYNACEAE) BASED ON MOLECULAR AND MORPHOLOGICAL EVIDENCE1 ABSTRACT To elucidate deeper relationships within Rauvolfioideae (Apocynaceae), a phylogenetic analysis was conducted using sequences from five DNA regions of the chloroplast genome (matK, rbcL, rpl16 intron, rps16 intron, and 39 trnK intron), as well as morphology. Bayesian and parsimony analyses were performed on sequences from 50 taxa of Rauvolfioideae and 16 taxa from Apocynoideae. Neither subfamily is monophyletic, Rauvolfioideae because it is a grade and Apocynoideae because the subfamilies Periplocoideae, Secamonoideae, and Asclepiadoideae nest within it. In addition, three of the nine currently recognized tribes of Rauvolfioideae (Alstonieae, Melodineae, and Vinceae) are polyphyletic. We discuss morphological characters and identify pervasive homoplasy, particularly among fruit and seed characters previously used to delimit tribes in Rauvolfioideae, as the major source of incongruence between traditional classifications and our phylogenetic results. Based on our phylogeny, simple style-heads, syncarpous ovaries, indehiscent fruits, and winged seeds have evolved in parallel numerous times. A revised classification is offered for the subfamily, its tribes, and inclusive genera. Key words: Apocynaceae, classification, homoplasy, molecular phylogenetics, morphology, Rauvolfioideae, system- atics. During the past decade, phylogenetic studies, (Civeyrel et al., 1998; Civeyrel & Rowe, 2001; Liede especially those employing molecular data, have et al., 2002a, b; Rapini et al., 2003; Meve & Liede, significantly improved our understanding of higher- 2002, 2004; Verhoeven et al., 2003; Liede & Meve, level relationships within Apocynaceae s.l., leading to 2004; Liede-Schumann et al., 2005). the recognition of this family as a strongly supported Despite significant insights gained from studies clade composed of the traditional Apocynaceae s. -

Antrocom Journal of Anthropology ANTROCOM Journal Homepage
Antrocom Online Journal of Anthropology vol. 17. n. 1 (2021) 5-20 – ISSN 1973 – 2880 Antrocom Journal of Anthropology ANTROCOM journal homepage: http://www.antrocom.net Leshoma, the visionary plant of southern Africa Luca Pasquali 1Independent researcher e-mail <[email protected]>. keywords abstract Boophone disticha, The bulbaceous plant Boophone disticha – known mainly by the term leshoma given hallucinogens, lebollô, kia, by the Sotho ethnic group – is characterized by powerful hallucinogenic properties and is used Basotho, San, South Africa as initiatory and divinatory plant among many southern African ethnicities. Once known as the main compound of San arrow poisons, its psychoactive properties have been recognized by Western scholars only in the last 50 years, since its ritual use was strictly kept secret by its initiates. Through the analysis of the few ancient and modern ethnographic observations that have been able to bypass the wall of secrecy that envelop the use of this plant, the Sotho male initiation rite (lebollô la banna) and the use of the plant as divinatory “bioscope ” among the South African sangoma (healers) are described. As evidenced by archaeological findings, man’s relationship with this plant has lasted for at least 2000 years. The plant The plant of leshoma is botanically classified as Boophone disticha (L. f.) Herb., belonging to the Amaryllidaceae family 1. It is a bulbaceous plant, with the bulb partially protruding from the ground. Each year the leafless bulb produces a beautiful fan of leaves which often are wavy in their margins at maturity. Once the vegetative stage is over, the plant loses its leaves, and the flowering stage begin. -

Plant Powers, Poisons, and Herb Craft
PLANT POWERS, POISONS, AND HERB CRAFT BY DALE PENDELL Foreword by Gary Snyde, $21.95 US In 'Pharmako/Poeia, Dale Pendell offers a mesmerizing guide to psychoactive Alternative plants, from their pharmacological roots to the literary offshoots. "This is a Health/ book," writes Gary Snyder, "about danger: dangerous knowledge, even more Literature dangerous ignorance." Against the greater danger, ignorance, Pendell strikes a formidable blow, as he proves himself a wise and witty guide to our plant teach- ers, their powers and their poisons. "Dale Pendell reactivates the ancient connection between the bardic poet and the shaman. His Pharmako/Poeia is a litany to the secret plant allies that have always accompanied us along the alchemical trajectory that leads to a new and yet authentically archaic future." — Terence McKenna, author of True Hallucinations "Much of our life-force calls upon the plant world for support, in medicines and in foods, as both allies and teachers. Pendell provides a beautifully crafted bridge between these two worlds. The magic he shares is that the voices are spoken and heard both ways; we communicate with plants and they with us. This book is a moving and poetic presentation of this dialogue." — Dr. Alexander T. Shulgin, University of California at Berkeley, Department of Public Health "Pharmako/Poeia is an epic poem on plant humours, an abstruse alchemic treatise, an experiential narrative jigsaw puzzle, a hip and learned wild-nature reference text, a comic paean to cosmic consciousness, an ecological handbook, a dried-herb pastiche, a countercultural encyclopedia of ancient fact and lore that cuts through the present 'conservative' war-on-drugs psychobabble." - Allen Ginsberg, poet Cover design "Dale PendelFs remarkable book will make it impossible to and color work ever again underestimate the most unprepossessing plant. -

Deploying Microbial Synthesis for Halogenating and Diversifying Medicinal Alkaloid Scaffolds
Downloaded from orbit.dtu.dk on: Sep 28, 2021 Deploying Microbial Synthesis for Halogenating and Diversifying Medicinal Alkaloid Scaffolds Bradley, Samuel Alan; Zhang, Jie; Jensen, Michael Krogh Published in: Frontiers in Bioengineering and Biotechnology Link to article, DOI: 10.3389/fbioe.2020.594126 Publication date: 2020 Document Version Publisher's PDF, also known as Version of record Link back to DTU Orbit Citation (APA): Bradley, S. A., Zhang, J., & Jensen, M. K. (2020). Deploying Microbial Synthesis for Halogenating and Diversifying Medicinal Alkaloid Scaffolds. Frontiers in Bioengineering and Biotechnology, 8, [594126]. https://doi.org/10.3389/fbioe.2020.594126 General rights Copyright and moral rights for the publications made accessible in the public portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognise and abide by the legal requirements associated with these rights. Users may download and print one copy of any publication from the public portal for the purpose of private study or research. You may not further distribute the material or use it for any profit-making activity or commercial gain You may freely distribute the URL identifying the publication in the public portal If you believe that this document breaches copyright please contact us providing details, and we will remove access to the work immediately and investigate your claim. fbioe-08-594126 October 19, 2020 Time: 19:15 # 1 REVIEW published: 23 October 2020 doi: 10.3389/fbioe.2020.594126 Deploying Microbial Synthesis for Halogenating and Diversifying Medicinal Alkaloid Scaffolds Samuel A. Bradley, Jie Zhang and Michael K. -

Hallucinogenic Plants – a Golden Guide
Downloaded from https://www.holybooks.com: https://www.holybooks.com/hallucinogenic-plants-golden-guide/ Complete your collection of Golden Guides and Golden Field Guides! Some titles may be temporarily unavailable at local retailers. To order, send check or money order to: Dept. M, Western Publishing Company, Inc., 1220 Mound Avenue, Racine, Wisconsin 53404. Be sure to include 35¢ per book !o cover postage and handling. GOLDEN GUIDES: $1.95 GOLDEN FIELD GUIDES: softcover, $4.95; hardcover, $7.95 GOLDEN GUIDES NATURE BIRDS • BUTTERFLIES AND MOTHS • CACTI • CATS EXOTIC PLANTS FOR HOUSE AND GARDEN • FISHES FLOWERS • FOSSILS • GAMEBIRDS • HALLUCINOGENIC PLANTS HERBS AND SPICES • INSECT PESTS • INSECTS NON-FLOWERING PLANTS • ORCHIDS • POND LIFE REPTILES AND AMPHIBIANS • ROCKS AND MINERALS THE ROCKY MOUNTAINS • SEASHELLS OF THE WORLD • SEASHORES SKY OBSERVER'S GUIDE • SPIDERS AND THEIR KIN • STARS TREES • TROPICAL FISH • WEEDS • YOSEMITE • ZOO ANIMALS SCIENCE BOTANY • ECOLOGY • EVOLUTION • FAMILIES OF BIRDS GEOLOGY • HEART • LANDFORMS • LIGHT AND COLOR OCEANOGRAPHY • WEATHER • ZOOLOGY HOBBIES AMERICAN ANTIQUE GLASS • ANTIQUES CASINO GAMES • FISHING INDIAN ARTS • KITES • WINES GOLDEN FIELD GUIDES BIRDS OF NORTH AMERICA • MINERALS OF THE WORLD SEASHELLS OF NORTH AMERICA • TREES OF NORTH AMERICA Golden, A Golden Guide®, and Golden Press® Downloadedare trademarks fromof Western https://www.holybooks.com: Publishing Company, Inc. https://www.holybooks.com/hallucinogenic-plants-golden-guide/ HALLUCINOGENIC PLANTS by RICHARD EVANS SCHULTES Illustrated by ELMER W. SMITH ® GOLDEN PRESS • NEW YORK Western Publishing Company, Inc. Racine, Wisconsin Downloaded from https://www.holybooks.com: https://www.holybooks.com/hallucinogenic-plants-golden-guide/ FOREWORD Hallucinogenic plants have been used by man for thou sands of years, probably since he began gathering plants for food.