Implementation of Medical Abortion in Norway 1998-2013
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Convention on the Rights of the Child (Article 42)
UNITED CRC NATIONS Convention on the Distr. Rights of the Child GENERAL CRC/C/129/Add.1 6 October 2004 Original: ENGLISH COMMITTEE ON THE RIGHTS OF THE CHILD CONSIDERATION OF REPORTS SUBMITTED BY STATES PARTIES UNDER ARTICLE 44 OF THE CONVENTION Third periodic report of States parties due in 2003 NORWAY* ** [24 April 2003] * For the second periodic report submitted by Norway, see CRC/C/70/Add.2; for its consideration by the Committee on 2 June 2000, see CRC/C/SR.625-626 and CRC/C/15/Add.126. ** In accordance with the information transmitted to States parties regarding the processing of their reports, the present document was not formally edited before being sent to the United Nations translation services. GE.04-44570 (E) 040105 CRC/C/129/Add.1 page 2 CONTENTS Paragraphs Page Foreword ................................................................................................... 1 - 3 5 Introduction .............................................................................................. 4 - 17 5 CHAPTER I. GENERAL MEASURES OF IMPLEMENTATION .... 18 - 77 8 A. Measures within national legislation and practice (article 4) ................................................................................ 18 - 53 8 B. Measures to increase awareness among adults and children of the principles and provisions of the Convention on the Rights of the Child (article 42) .............................................. 54 - 74 17 C. Measures to make Norway’s report widely available ............ 75 - 77 22 CHAPTER II. DEFINITION OF THE CHILD ..................................... 78 - 100 23 CHAPTER III. GENERAL PRINCIPLES .............................................. 101 - 212 28 A. Non-discrimination (article 2) ............................................... 101 - 136 28 B. The best interests of the child (article 3) ............................... 137 - 175 35 C. The right to life, survival and development (article 6) .......... 176 - 180 42 D. Respect for the views of the child (article 12) ...................... -

The Safety and Quality of Abortion Care in the United States (2018)
THE NATIONAL ACADEMIES PRESS This PDF is available at http://nap.edu/24950 SHARE The Safety and Quality of Abortion Care in the United States (2018) DETAILS 222 pages | 6 x 9 | PAPERBACK ISBN 978-0-309-46818-3 | DOI 10.17226/24950 CONTRIBUTORS GET THIS BOOK Committee on Reproductive Health Services: Assessing the Safety and Quality of Abortion Care in the U.S.; Board on Population Health and Public Health Practice; Board on Health Care Services; Health and Medicine Division; National FIND RELATED TITLES Academies of Sciences, Engineering, and Medicine SUGGESTED CITATION National Academies of Sciences, Engineering, and Medicine 2018. The Safety and Quality of Abortion Care in the United States. Washington, DC: The National Academies Press. https://doi.org/10.17226/24950. Visit the National Academies Press at NAP.edu and login or register to get: – Access to free PDF downloads of thousands of scientific reports – 10% off the price of print titles – Email or social media notifications of new titles related to your interests – Special offers and discounts Distribution, posting, or copying of this PDF is strictly prohibited without written permission of the National Academies Press. (Request Permission) Unless otherwise indicated, all materials in this PDF are copyrighted by the National Academy of Sciences. Copyright © National Academy of Sciences. All rights reserved. The Safety and Quality of Abortion Care in the United States THE SAFETY AND QUALITY OF ABORTION CARE IN THE UNITED STATES Committee on Reproductive Health Services: Assessing the Safety and Quality of Abortion Care in the U.S. Board on Population Health and Public Health Practice Board on Health Care Services Health and Medicine Division A Consensus Study Report of Copyright National Academy of Sciences. -

Explaining the Exceptional Behaviour of the Portuguese Church Hierarchy in Morality Politics
Shunning Direct Intervention: Explaining the Exceptional Behaviour of the Portuguese church Hierarchy in Morality Politics by Madalena Meyer Resende (FCSH-UNL and IPRI-UNL) and Anja Hennig (European University Viadrina) Abstract Why are the Catholic churches in most European countries politically active in relevant morality policy issues while the Portuguese hierarchy has remained reserved during mobilizing debates such as abortion and same-sex marriage, whose laws’ recent changes go against Catholic beliefs? The explanation could be institutional, as the fairly recent Portuguese transition to democracy dramatically changed the role attributed to the church by the former regimes. However, in Spain – whose case is similar to Portugal in matters of timing and political conditions – the hierarchy’s behaviour is different. This begs the question: what elements explain the exceptionality of the Portuguese case? This article shows that the Portuguese case illustrates an element usually not emphasized in the literature: the ideological inclination of the church elites. The article thus concludes that institutional access is a necessary, but not a sufficient, condition for the church to directly intervene in morality policy processes. A church may have access to influence political decision makers but, for ideological reasons, may be unwilling to use it. Keywords: Portugal, morality policy, Catholic church, Vatican Council II, abortion, gay-marriage, ideology, historical institutionalism Introduction the church from the policy-making arena. As we The recent debate in the Portuguese parliament will show, up until 2013, the Portuguese hierar- (July 2015) about restricting the 2007 liberal- chy showed great restraint during the process of ized abortion law in Portugal revealed a novum moral-political liberalization. -

Conscientious Objection to the Provision of Reproductive Healthcare
Volume 123, Supplement 3 (2013) Amsterdam • Boston • London • New York • Oxford • Paris • Philadelphia • San Diego • St. Louis International Journal of GYNECOLOGY & OBSTETRICS Editor: T. Johnson (USA) Editor Emeritus: J. Sciarra (USA) Associate Editor: W. Holzgreve (Germany) P. Serafini (Brazil) J. Fortney (USA) Associate Editor Emeritus: L. Keith (USA) Managing Editor: C. Addington (UK) Manuscript Editor: P. Chapman (UK) Honorary Associate Editor: L. Hamberger (Sweden) Associate Editors Ethical and Legal Issues R. Cook (Canada) in Reproductive Health: B. Dickens (Canada) Enabling Technologies: M. Hammoud (USA) FIGO Staging of Gynecologic Cancer: L. Denny (South Africa) Contemporary Issues in R. Adanu (Ghana) Women’s Health: V. Boama (South Africa) V. Guinto (Philippines) C. Sosa (Uruguay) Statistical Consultant: A. Vahratian (USA) Editorial Office: FIGO Secretariat, FIGO House Suite 3 - Waterloo Court, 10 Theed Street, London, SE1 8ST, UK Tel: +44 20 7928 1166 Fax: +44 20 7928 7099 E-mail: [email protected] Supplement to International Journal of Gynecology & Obstetrics Volume 123, Supplement 3 Conscientious objection to the provision of reproductive healthcare Guest Editor: Wendy Chavkin MD, MPH Publication of this supplement was made possible with support from Ford Foundation and an anonymous donor. We thank all Global Doctors for Choice funders for making the project possible. © 2013 International Federation of Gynecology and Obstetrics. All rights reserved. 0020-7292/06/$32.00 This journal and the individual contributions contained in it are protected under copyright by International Federation of Gynecology and Obstetrics, and the following terms and conditions apply to their use: Photocopying Single photocopies of single articles may be made for personal use as allowed by national copyright laws. -

Clinical Updates in Reproductive Health
APRIL 2019 Clinical Updates in Reproductive Health Please use and share widely: www.ipas.org/clinicalupdates Also available in Spanish: www.ipas.org/actualizacionesclinicas For more information, email [email protected] CURH-E19 April 2019 © 2019 Ipas. Produced in the United States of America. Suggested citation: Ipas. (2019). Clinical Updates in Reproductive Health. L. Castleman & N. Kapp (Eds.). Chapel Hill, NC: Ipas. Ipas works globally to improve access to safe abortion and contraception so that every woman and girl can determine her own future. Across Africa, Asia and Latin America, we work with partners to make safe abortion and contraception widely available, to connect women with vital information so they can access safe services, and to advocate for safe, legal abortion. Cover photos, left to right: © Ipas; © Richard Lord; © Benjamin Porter Ipas is a registered 501(c)(3) nonprofit organization. All contributions to Ipas are tax deductible to the full extent allowed by law. For more information or to donate to Ipas: Ipas P.O. Box 9990 Chapel Hill, NC 27515 USA 1-919-967-7052 www.ipas.org APRIL 2019 Clinical Updates in Reproductive Health Medical Editor: Nathalie Kapp Medical Director: Laura Castleman Lead Writer: Emily Jackson Clinical advisory team: Sangeeta Batra, India Deeb Shrestha Dangol, Nepal Abiyot Belai, Ethiopia Steve Luboya, Zambia Guillermo Ortiz, United States Claudia Martinez Lopez, Mexico Bill Powell, United States ACKNOWLEDGEMENTS Thanks to those who contributed to this and previous versions of Clinical Updates in Reproductive Health: Rebecca Allen Lynn Borgatta Dalia Brahmi Anne Burke Catherine Casino Talemoh Dah Gillian Dean Alison Edelman Courtney Firestine Mary Fjerstad Bela Ganatra Vinita Goyal Joan Healy Bliss Kaneshiro Ann Leonard Radha Lewis Patricia Lohr Alice Mark (Founding Editor) Lisa Memmel Karen Padilla Regina Renner Cristião Rosas Laura Schoedler Clinical Updates topics are determined through queries gathered from Ipas-supported train- ings and programs in the public and private health sectors. -

How Politics and Abortion Laws Decides Women's Future
The Faculty of Health Sciences, UiT The Arctic University of Norway, 2017 Unsafe abortion in legally restricted areas – how politics and abortion laws decides women’s future A literature review on the incidence of induced abortion and adverse health consequences in Sub-Saharan African countries with restrictive abortion laws Edvarda Louise Salomonsen Report: MED-3950 Master Thesis/Class of 2012 Preface After spending three months on clinical rotation in Zimbabwe during my 4th year of medical school, I developed an interest in global health and especially women’s reproductive health. During my stay, I saw a lot of women admitted for complications following possibly unsafe abortions, and I noticed how vulnerable and stigmatized these women were. Zimbabwe do not permit abortion for any social reason, and it became clear to me during my stay in the Sub-Saharan African country that health is politics, and that a large proportion of the world’s population are suffering from the decisions of others. A woman dying of pregnancy-related causes is one of the world’s biggest tragedies, and I wanted to write my thesis about a subject that is important for global health, and even more important for me as a future doctor and citizen of the world. Writing a master thesis on unsafe abortion in countries with restrictive abortion laws is my contribution to the global community. I want to express my gratitude to my supervisor Jon Øyvind Odland for helping me shed some light on these important matters, for his engagement, and for being optimistic, helpful and supportive during the work of this thesis. -

Abortion Laws in Transnational Perspective: Cases and Controversies
This is a repository copy of Abortion Laws in Transnational Perspective: Cases and Controversies. Book Review. White Rose Research Online URL for this paper: http://eprints.whiterose.ac.uk/98822/ Version: Accepted Version Article: Krajewska, A. orcid.org/0000-0001-9096-1056 (2016) Abortion Laws in Transnational Perspective: Cases and Controversies. Book Review. Medical Law Review, 24 (2). pp. 290-296. ISSN 0967-0742 https://doi.org/10.1093/medlaw/fwv041 Reuse Unless indicated otherwise, fulltext items are protected by copyright with all rights reserved. The copyright exception in section 29 of the Copyright, Designs and Patents Act 1988 allows the making of a single copy solely for the purpose of non-commercial research or private study within the limits of fair dealing. The publisher or other rights-holder may allow further reproduction and re-use of this version - refer to the White Rose Research Online record for this item. Where records identify the publisher as the copyright holder, users can verify any specific terms of use on the publisher’s website. Takedown If you consider content in White Rose Research Online to be in breach of UK law, please notify us by emailing [email protected] including the URL of the record and the reason for the withdrawal request. [email protected] https://eprints.whiterose.ac.uk/ Abortion Laws in Transnational Perspective: Cases and Controversies REBECCA J COOK, JOANNA N ERDMAN, BERNARD M DICKENS (eds.) Philadelphia, University of Pennsylvania Press, 2014, 480 pp., hardback, £45.50, 9780812246278 Atina Krajewska, Sheffield Law School, University of Sheffield, England, [email protected] For a while at least, it seemed that proponents and opponents of decriminalisation and liberalisation of abortion laws had become entrenched in their well-known positions and that national legislators and politicians had reached a form of, usually fragile, consensus. -
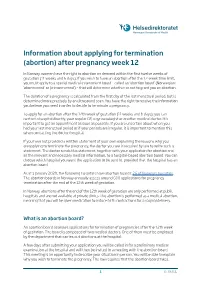
Information About Applying for Termination (Abortion) After Pregnancy Week 12
Information about applying for termination (abortion) after pregnancy week 12 In Norway, women have the right to abortion on demand within the first twelve weeks of gestation (11 weeks and 6 days). If you wish to have an abortion after the 12-week time limit, you must apply to a special medical assessment board – called an ’abortion board’ (Norwegian: ‘abortnemnd’ or ‘primærnemnd’) – that will determine whether or not to grant you an abortion. The duration of a pregnancy is calculated from the first day of the last menstrual period, but is determined more precisely by an ultrasound scan. You have the right to receive the information you believe you need in order to decide to terminate a pregnancy. To apply for an abortion after the 12th week of gestation (11 weeks and 6 days), you can contact a hospital directly, your regular GP, a gynaecologist or another medical doctor. It is important to get an appointment as soon as possible. If you are uncertain about when you had your last menstrual period or if your periods are irregular, it is important to mention this when contacting the doctor/hospital. If you have not provided a written statement of your own explaining the reasons why you areapplying to terminate the pregnancy, the doctor you see is required by law to write such a statement. The doctor sends this statement, together with your application for abortion and all the relevant and necessary medical information, to a hospital-based abortion board. You can choose which hospital you want the application to be sent to, provided that the hospital has an abortion board. -

Norway Health System Review
Health Systems in Transition Vol. 15 No. 8 2013 Norway Health system review Ånen Ringard • Anna Sagan Ingrid Sperre Saunes • Anne Karin Lindahl Anna Sagan (Editor), Sarah Thomson and Ewout van Ginneken were responsible for this HiT Editorial Board Series editors Reinhard Busse, Berlin University of Technology, Germany Josep Figueras, European Observatory on Health Systems and Policies Martin McKee, London School of Hygiene & Tropical Medicine, United Kingdom Elias Mossialos, London School of Economics and Political Science, United Kingdom Sarah Thomson, European Observatory on Health Systems and Policies Ewout van Ginneken, Berlin University of Technology, Germany Series coordinator Gabriele Pastorino, European Observatory on Health Systems and Policies Editorial team Jonathan Cylus, European Observatory on Health Systems and Policies Cristina Hernández-Quevedo, European Observatory on Health Systems and Policies Marina Karanikolos, European Observatory on Health Systems and Policies Anna Maresso, European Observatory on Health Systems and Policies David McDaid, European Observatory on Health Systems and Policies Sherry Merkur, European Observatory on Health Systems and Policies Philipa Mladovsky, European Observatory on Health Systems and Policies Dimitra Panteli, Berlin University of Technology, Germany Wilm Quentin, Berlin University of Technology, Germany Bernd Rechel, European Observatory on Health Systems and Policies Erica Richardson, European Observatory on Health Systems and Policies Anna Sagan, European Observatory on Health -

Fetal Cannibalism Planned Parenthood Style in China They Eat Babies; Planned Parenthood Kills Them and Then Sells Their Organs
Volume 25, Number 5 September-October 2015 A review and analysis of worldwide population control activity Fetal Cannibalism Planned Parenthood Style In China they eat babies; Planned Parenthood kills them and then sells their organs. Which is worse? By Steven Mosher and Jonathan Abbamonte On the menu of some exclusive Chinese restaurants is an item that goes by the name of Spare Rib Soup. Very expensive, it is usually served only in the back rooms to known customers, who are willing to pay to premium for this delicacy. So what is Spare Rib Soup? Brace yourselves. Spare Rib Soup is actually a human soup, made from the bodies of aborted babies. It is regarded by the Chinese—at least some Chinese—as a rejuvenating potion. A kind of fountain of youth that will fix sagging wrinkles, grow back missing hair, and generally put a spring back in your step. Shutterstock All of which is quite simply discusses the importance of not nonsense. crushing the organs so she “can get INSIDE THIS ISSUE But I thought of Spare Rib Soup it all intact” will stay with you a long Fetal Cannibalism 1 when I watched the video of Dr. time. Or the thought of her sipping President’s Page 2 Deborah Nucatola, Senior Director her cabernet sauvignon as she brags, May I Send You These Gifts? 4 of Medical Services, Planned “We’ve been very good at getting Manual Vacuum Aspirators 6 Parenthood, describing how her heart, lung, liver.” How the abortionist can manage to Tough Challenges Ahead 8 organization is harvesting and selling parts and pieces from aborted babies. -

Teenage Pregnancies Internationally
FORUMSex Education and Family Planning 2 – 2007 ´ ` ´ ` Information service of the Federal Centre for Health Education Teenage´ pregnancies ` Underage pregnant women Services provided Teenage Fertility internationallyin Germany. and help required for in Ireland Statistical data on underage pregnant women Stephanie O’Keeffe, Mary Smith terminations of pregnancy and mothers in Berlin and births and Brandenburg. Sexual and reproductive ´ Evelyn Laue Results of a survey of experts health. Monika Häußler-Sczepan, Preventing unwanted Teenage pregnancies Sabine Wienholz pregnancies and abortion in Germany. in Norway Results of a study of the risk ‘Pregnant under 18’. Ulla Leth Ollendorff factors and contraception A new Internet service failures in the case of from the Federal Centre Adolescent pregnancy ` pregnancies of underage for Health Education in Iceland women Petra Otto, Mechthild Paul Sóley S. Bender Karin Block, Silja Matthiesen Trends in teenage live births and their determinants in Europe ´ Osmo Kontula ` EDITORIAL In this third issue of the FORUM series on the subject of ‘Teenage pregnancies’ the perspective is extended: As well as contributions on current studies in Germany, we are also providing information about representative data and approaches to prevention in other European countries. First of all the Federal Statistical Office gives an overview of the number of births and terminations of pregnancy by underage women in Germany and shows the development between 2000 and 2006. Based on a survey carried out amongst some 1,800 underage pregnant women in pro familia information centres, specialists have addressed the risk factors and errors in contraception which are most often the cause of unwanted pregnancies. We also report on a study, conducted on behalf of the BZgA, in which it was assessed on the basis of 100 expert interviews what provisions and help are available for underage pregnant women in Berlin and Brandenburg, whether the existing services are known and whether they are accepted by the young people. -

Peasant Radicalism in Early Nineteenth Century Norway: the Case of Hans Nielsen Hauge (1771-1824)
Peasant Radicalism in Early Nineteenth Century Norway: The Case of Hans Nielsen Hauge (1771-1824) Glen Peter Ryland B.A., Trinity Western University, 1989 PROJECT SUBMITTED IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF MASTER OF ARTS IN LIBERAL STUDIES In the Graduate Liberal Studies Program 43 Glen Ryland 2005 SIMON FRASER UNIVERSITY Fall, 2005 All rights reserved. This work may not be reproduced in whole or in part, by photocopy or other means, without permission of the author. APPROVAL Name: Glen Ryland Degree: Master of Arts in Liberal Studies Title of Project: Peasant Radicalism in Early Nineteenth Century Norway: The Case of Hans Nielsen Hauge (177 1- 1824) Examining Committee: Chair: Dr. Anne Marie Feenberg-Dibon Associate Director of Graduate Liberal Studies Dr. Michael Fellman Supervisor Director, Graduate Liberal Studies Dr. Stephen Duguid Examiner Professor of Humanities Dr. Michael Kenny External Examiner Professor of Anthropology Date DefendedlApproved: October 13,2005 . 11 SIMON FRASER ' UNIWRSIW~I bra ry DECLARATION OF PARTIAL COPYRIGHT LICENCE The author, whose copyright is declared on the title page of this work, has granted to Simon Fraser University the right to lend this thesis, project or extended essay to users of the Simon Fraser University Library, and to make partial or single copies only for such users or in response to a request from the library of any other university, or other educational institution, on its own behalf or for one of its users. The author has further granted permission to Simon Fraser University to keep or make a digital copy for use in its circulating collection, and, without changing the content, to translate the thesislproject or extended essays, if technically possible, to any medium or format for the purpose of preservation of the digital work.