Brief to the House of Commons Standing Committee on Health On
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Animal-To-Human Transplantation: Should Canada Proceed?
Animal-to-human transplantation: Should Canada proceed? A public consultation on xenotransplantation Canadian Public Health Association Animal-to-human transplantation: Should Canada proceed? A public consultation on xenotransplantation © December 2001 by the Canadian Public Health Association Permission is granted for non-commercial reproduction only, provided there is a clear acknowledgement of the source. ISBN 1-894324-20-X Canadian Public Health Association 400-1565 Carling Avenue Ottawa, Ontario, Canada, K1Z 8R1 CPHA’s Mission Statement The Canadian Public Health Association (CPHA) is a national, independent, not-for- profit, voluntary association representing public health in Canada with links to the international public health community. CPHA’s members believe in universal and equitable access to the basic conditions which are necessary to achieve health for all Canadians. CPHA’s mission is to constitute a special national resource in Canada that advocates for the improvement and maintenance of personal and community health according to the public health principles of disease prevention, health promotion and protection, and healthy public policy. This consultation was funded by Health Canada. The views expressed in this report are those of the Public Advisory Group, and are based on consultations with a broad sector of the Canadian public. They do not necessarily represent the official policy or views of Health Canada or the Canadian Public Health Association. The English and French reports and executive summaries are available on the consultation website at http://www.xeno.cpha.ca or through http://www.cpha.ca. French translation by Sylvie Lee January 7, 2002 The Honourable Allan Rock Minister of Health Brooke Claxton Building, Tunney’s Pasture Ottawa, Ontario, K1A 0K9 Dear Minister Rock: It is our pleasure to provide you with the report Animal-to-human transplantation: Should Canada proceed? This report documents the results of a comprehensive consultation with Canadians on the complex issue of xenotransplantation. -
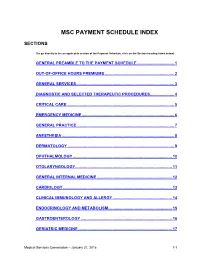
Msc Payment Schedule Index
MSC PAYMENT SCHEDULE INDEX SECTIONS (To go directly to the an applicable section of the Payment Schedule, click on the Section heading listed below) GENERAL PREAMBLE TO THE PAYMENT SCHEDULE .................................. 1 2. OUT-OF-OFFICE HOURS PREMIUMS ............................................................... 2 3. GENERAL SERVICES ......................................................................................... 3 4. DIAGNOSTIC AND SELECTED THERAPEUTIC PROCEDURES ...................... 4 5. CRITICAL CARE .................................................................................................. 5 6. EMERGENCY MEDICINE .................................................................................... 6 7. GENERAL PRACTICE ......................................................................................... 7 8. ANESTHESIA ...................................................................................................... 8 9. DERMATOLOGY ................................................................................................. 9 10. OPHTHALMOLOGY .......................................................................................... 10 11. OTOLARYNGOLOGY ........................................................................................ 11 12. GENERAL INTERNAL MEDICINE .................................................................... 12 13. CARDIOLOGY ................................................................................................... 13 14. CLINICAL IMMUNOLOGY AND ALLERGY -

Chronic Hepatitis C Viral Infection: Natural History and Treatment Outcomes in Substance Abusers
Chronic Hepatitis C Viral Infection: Natural History and Treatment Outcomes in Substance Abusers by Ava Ayana John-Baptiste A thesis submitted in conformity with the requirements for the degree of Doctor of Philosophy Graduate Department of Health Policy, Management and Evaluation University of Toronto © Copyright by Ava Ayana John-Baptiste, 2010 Chronic Hepatitis C Viral Infection: Natural History and Treatment Outcomes in Substance Abusers Ava Ayana John-Baptiste Doctor of Philosophy Graduate Department of Health Policy, Management and Evaluation University of Toronto 2010 Abstract Hepatitis C is the most common blood-borne viral illness in the North America. Chronic hepatitis C infection may lead to cirrhosis of the liver, liver failure and liver cancer. In North America, injection drug use is the most important risk factor for infection and substance abusing populations are disproportionately affected by the disease. Antiviral therapy exists and approximately 50% of infected individuals can be cured. The aim of this thesis was to provide information to help clinicians and policy-makers minimize the impact of hepatitis C in substance abusers. The thesis is comprised of three studies. The first assessed the rate of progression to cirrhosis for those acquiring infection through injection drug use, using a meta-analysis of 44 studies from the published literature. We estimated that fibrosis progression occurs at a rate of 8.1 per 1000 person-years (95% Credible Region (CR), 3.9 to 14.7) corresponding to a 20-year cirrhosis prevalence of 14.8% (95% CR, 7.5 to 25.5). The second study measured the association between successful antiviral therapy and quality of life. -

Organ Utilization Among Deceased Donors in Canada, 1993–
838 NEUROANESTHESIACANADIAN JOURNAL AND OFINTENSIVE ANESTHESIA CARE Organ utilization among deceased donors in Canada, 1993–2002 [L’utilisation d’organes de donneurs décédés au Canada de 1993 à 2002] Kim Badovinac MA MBA,* Paul D. Greig MD FRCS(C),† Heather Ross MD MHSc FRCPC,‡ Christopher J. Doig MD MSc FRCPC,§ Sam D. Shemie MD¶ Background: Optimizing organ utilization from consented Contexte : Optimaliser l’utilisation d’organes de donneurs con- donors is a critical need, given a static organ donation rate. We sentants est une véritable nécessité, étant donné la stabilité actu- report changes in the characteristics of donors and organ utili- elle du taux de don d’organes. Nous présentons les caractéristiques zation patterns in Canada over a ten-year period. des donneurs et de l’utilisation des organes au Canada au cours Methods: For the decade spanning the years 1993–2002, data d’une décennie. were extracted from the Canadian Organ Replacement Register Méthode : Pour la décennie 1993-2202, les données ont été (CORR), the national transplant registry. A donor was defined extraites du Registre canadien des insuffisances et des transplan- as a deceased person from whom at least one vital organ was tations d’organes (RCITO). Un donneur était défini comme une retrieved and transplanted. personne décédée chez qui un organe au moins était prélevé et Results: The donor pool is aging (median age of donors transplanté. increased eight years over the decade), with proportionately Résultats : Le pool de donneurs est âgé (l’âge moyen a augmenté fewer donors dying from head trauma (motor vehicle collisions) de huit ans pendant la décennie) et il y a proportionnellement and proportionately more from cerebrovascular accidents. -

Lung Transplant
Lung Transplant Information for Alberta & NWT Residents Disclaimer The information in this booklet is a guide and is meant to support the information given to you by your healthcare professionals. All information was current at the time of printing but things can and do change. The transplant centre team will provide much more information about lung transplants once a person is referred for assessment. c o n t e n t s 4 Introduction 6 The Basics of Breathing 7 General Transplant Information 9 Your Questions Answered 17 Becoming a Lung Transplant Candidate 21 The Costs of a Lung Transplant 27 Resources 30 Funding Uninsured Costs 35 Other Things to Consider 39 End of Life and Legal Decisions 42 Glossary of Lung Diseases 45 Planning Checklist 48 Notes 3 i n t r o d u c t i o n For those suffering from severe lung disease, having a lung transplant may be their only option to survive. This can be intimidating and at the same time it can be difficult to acquire qualified information to help make informed decisions regarding treatment. If you have been told that you need a lung transplant (or may need one in the future), you likely have many questions about what happens next. Not knowing what to expect can create a lot of fear and worry. This booklet is available to supplement the information available from other sources; more detailed or individually relevent information would be provided to you from the transplant team should you move forward with needing a lung transplant. There are currently five hospitals in Canada that perform lung transplants. -

Living with Liver Transplantation Canadian Cataloguing in Publication Data Main Entry Under Title: Living with Liver Transplantation Includes Index
Living with Liver Transplantation Canadian Cataloguing in Publication Data Main entry under title: Living with liver transplantation Includes index. 1. Liver--Transplantation 2. Liver--Transplantation--Patients--Care. I. British Columbia Transplant Society. RD546.L48 1995 617.5’560592 C95-911011-9 Copyright © British Columbia Transplant Society, 1996 No part of this manual may be reproduced without the written permission of the Director (or designate) of the British Columbia Transplant Society. 2 Living with Liver Transplantation Acknowledgments I would like to thank all of the health care professionals of the various transplant teams who participated in the development of this manual. Their time, patience, and guidance was appreciated. I would like to extend a very special thank you to the manual committee members from the Vancouver Hospital and Health Sciences Centre, St. Paul’s Hospital, and BC Transplant Society for their involvement in the monumental task of writing multi-organ manuals. Without their commitment of time, sharing of expertise, and genuine concern for providing the best possible patient education material, this manual would not be possible. I would also like to thank the Kidney Foundation of Canada for permission to use some of the graphics in this manual. Yours Sincerely, Sue Howard Clinical Coordinator British Columbia Transplant Society Manual Committee Chairperson Living with Liver Transplantation 3 Table of Contents Introduction Chapter 1: Transplantation History of Transplantation ............................................................7-8 -

Diverse Communities Vancouver Report
DIVERSE COMMUNITIES Consultation to Explore Perspectives on Organ and Tissue Donation SECTION III Vancouver Consultation with South Asian Communities TABLE OF CONTENTS 1. INTRODUCTION .................................................................................................. III-1 2. RESULTS ....................................................................................................... III-7 3. ANALYSIS ..................................................................................................... III-21 4. RECOMMENDATIONS....................................................................................... III-26 5. CONCLUSION.................................................................................................... III-26 APPENDIX A: CONSULTATION ON ORGAN AND TISSUE DONATION AND TRANSPLANTATION , VANCOUVER DRAFT DESCRIPTION, JANUARY 10, 2005 ..................................................................... III-28 APPENDIX B: PLANNING MEETING AGENDA ................................................. III-31 APPENDIX C: PROCESS FOR ORGANIZING PLANNING GROUP, FOCUS GROUPS AND INTERVIEWS........................................ III-32 APPENDIX D: PLANNING GROUP PARTICIPANTS ......................................... III-33 APPENDIX E: FINDINGS FROM PREVIOUS RESEARCH................................ III-34 APPENDIX F: FOCUS GROUP AND INTERVIEW INTRODUCTION ................ III-36 APPENDIX G: CONTACTS INITIATED............................................................... III-37 APPENDIX H: INTRODUCTORY LETTER -

Tissue Donation Potential Beyond Acute Care
The Canadian Council for Donation and Transplantation Tissue Donation Potential Beyond Acute Care Report © 2006 The Canadian Council for Donation and Transplantation This report may be reproduced in its present format without permission. Any alteration of contents must be approved by the Canadian Council for Donation and Transplantation. For reprints, please contact: The Canadian Council for Donation and Transplantation 1702, 8215 112 Street Edmonton, AB, Canada T6G 2C8 Telephone: 780 409-5651 Email: [email protected] www.ccdt.ca August 2006 ISBN 978-0-9738718-9-0 The Canadian Council for Donation and Transplantation (CCDT) assumes no responsibility or liability for any consequences, losses or injuries, foreseen or unforeseen, whatsoever or howsoever occurring, which might result from the implementation, use or misuse of any information or recommendations in the report, Tissue Donation Potential Beyond Acute Care. The views expressed herein do not necessarily represent the views of the CCDT and/or the federal, provincial or territorial governments of Canada. Production of this advice/report has been made possible through a financial contribution from Health Canada. Executive summary The Canadian Council for Donation and Transplantation (CCDT) was formed in 2001 with a mandate to develop advice for the Conference of Deputy Ministers of Health on issues and strategies related to organ and tissue donation and transplantation in Canada. The principle mandate of the Donation Committee of the CCDT is to ensure that all individuals who wish to give a gift of organ and tissue donation be given the opportunity to do so. To address this mandate, the Donation Committee strives to identify and eliminate barriers that prevent opportunities for families to donate tissues and organs of their deceased relatives. -

CIBMTR Scientific Working Committee Research Portfolio July 1, 2019
CIBMTR Scientific July 1, Working Committee 2019 Research Portfolio Milwaukee Campus Minneapolis Campus Medical College of Wisconsin National Marrow Donor Program/ 9200 W Wisconsin Ave, Suite C5500 Be The Match – 500 N 5th St Milwaukee, WI 53226 USA Minneapolis, MN 55401-9959 USA (414) 805-0700 (763) 406-5800 cibmtr.org CIBMTR Scientific Working Committee Research Portfolio: July 1, 2019 TABLE OF CONTENTS 1.0 OVERVIEW .................................................................................................................................................................. 1 1.1 Membership ........................................................................................................................................................... 2 1.2 Leadership .............................................................................................................................................................. 2 1.3 Productivity ............................................................................................................................................................ 3 1.4 How to Get Involved ............................................................................................................................................ 3 2.0 ACUTE LEUKEMIA WORKING COMMITTEE .................................................................................................. 6 2.1 Leadership ............................................................................................................................................................. -
Canadian Highly Sensitized Patient and Living Donor Paired Exchange Registries
The Canadian Council for Donation and Transplantation Canadian Highly Sensitized Patient and Living Donor Paired Exchange Registries October 28-30, 2005 Toronto, Ontario Task Force Discussion Document © 2005 The Canadian Council for Donation and Transplantation This report may be reproduced in its present format without permission. Any alteration of contents must be approved by the Canadian Council for Donation and Transplantation. For reprints, please contact: The Canadian Council for Donation and Transplantation 1702, 8215 112 Street Edmonton, AB, Canada T6G 2C8 Telephone: 780 409-5651 Email: [email protected] www.ccdt.ca December 2005 ISBN 0-9738718-5-7 The Canadian Council for Donation and Transplantation (CCDT) assumes no responsibility or liability for any consequences, losses or injuries, foreseen or unforeseen, whatsoever or howsoever occurring, which might result from the implementation, use or misuse of any information or recommendations in the report, Canadian Highly Sensitized Patient and Living Donor Paired Exchange Registries. This report contains recommendations that must be assessed in the context of a full review of applicable medical, legal and ethical requirements in any individual case. The views expressed herein do not necessarily represent the views of the CCDT and/or the Federal, Provincial or Territorial governments of Canada. Production of this advice/report has been made possible through a financial contribution from Health Canada. Contents PREFACE ................................................................................................................................... -

Canadian Organ Replacement Register Annual Report: Treatment of End-Stage Organ Failure in Canada, 2004 to 2013
Canadian Organ Replacement Register Annual Report: Treatment of End-Stage Organ Failure in Canada, 2004 to 2013 Report April 2015 Types of Care Our Vision Better data. Better decisions. Healthier Canadians. Our Mandate To lead the development and maintenance of comprehensive and integrated health information that enables sound policy and effective health system management that improve health and health care. Our Values Respect, Integrity, Collaboration, Excellence, Innovation Table of Contents Acknowledgements .....................................................................................................................5 Summary ....................................................................................................................................7 Highlights ....................................................................................................................................9 Chapter 1—Introduction ............................................................................................................ 13 1.1 Data Sources .................................................................................................................. 15 1.2 Under-Reporting Across Canada .................................................................................... 16 1.3 Data Quality .................................................................................................................... 18 1.4 Organization of the Report ............................................................................................. -
Kidney Transplant Recipient Booklet
LLIIVVIINNGG WWIITTHH KKIIDDNNEEYY TTRRAANNSSPPLLAANNTTAATTIIOONN www.transplant.bc.ca 1 INTRODUCTION This booklet has been written to provide you with information about living with a kidney transplant. Please take some time to go through this booklet to help you to have a better understanding about kidney transplantation. Should you have any further questions, please contact us at the following numbers: Vancouver Coastal Health Program Coordinator * Kidney Pre-Transplant Service 5th Floor, Solid Organ Transplant Clinic Gordon & Leslie Diamond Health Care Centre 2775 Laurel Street, Vancouver, BC V5Z 1M9 Phone: 604 875-5182 Fax: 604 875-5236 St. Paul’s Hospital Clinical Nurse Leader and Patient Educator * Pre Kidney Transplant Program Ward 6A 1081 Burrard Street Vancouver, British Columbia V6Z 1Y6 Phone: 604 806-9078 Fax: 604 806-9658 British Columbia’s Children’s Hospital Transplant Nurse Clinician * 4480 Oak Street Vancouver, British Columbia V6H 3V4 Phone: 604 875-3604 Fax: 604 875-2943 * Referred to as transplant nurses in this booklet Living With Kidney Transplantation March 2011 2 Table of Contents Chapter 1 Introduction 5 I. Overview of Transplantation 6 II. Your Transplant Team 7 III. The History of Organ Transplantation 8 IV. How Your Kidneys Work 9 V. How Kidney Failure Affects Your Health 11 Chapter 2 Pre -Transplant Assessment 13 I. Being referred for transplant assessment 13 II. Before you appointment 14 III. Appointments with the transplant team 14 IV. Completing the assessment 15 Chapter 3 Living Donor Kidney Transplantation 17 I. Who can be a living kidney donor? 18 II. Paired kidney exchange program 19 III. Preparing for a living donor kidney transplant 20 IV.