Download File
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Genetic Variation Across the Human Olfactory Receptor Repertoire Alters Odor Perception
bioRxiv preprint doi: https://doi.org/10.1101/212431; this version posted November 1, 2017. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. Genetic variation across the human olfactory receptor repertoire alters odor perception Casey Trimmer1,*, Andreas Keller2, Nicolle R. Murphy1, Lindsey L. Snyder1, Jason R. Willer3, Maira Nagai4,5, Nicholas Katsanis3, Leslie B. Vosshall2,6,7, Hiroaki Matsunami4,8, and Joel D. Mainland1,9 1Monell Chemical Senses Center, Philadelphia, Pennsylvania, USA 2Laboratory of Neurogenetics and Behavior, The Rockefeller University, New York, New York, USA 3Center for Human Disease Modeling, Duke University Medical Center, Durham, North Carolina, USA 4Department of Molecular Genetics and Microbiology, Duke University Medical Center, Durham, North Carolina, USA 5Department of Biochemistry, University of Sao Paulo, Sao Paulo, Brazil 6Howard Hughes Medical Institute, New York, New York, USA 7Kavli Neural Systems Institute, New York, New York, USA 8Department of Neurobiology and Duke Institute for Brain Sciences, Duke University Medical Center, Durham, North Carolina, USA 9Department of Neuroscience, University of Pennsylvania School of Medicine, Philadelphia, Pennsylvania, USA *[email protected] ABSTRACT The human olfactory receptor repertoire is characterized by an abundance of genetic variation that affects receptor response, but the perceptual effects of this variation are unclear. To address this issue, we sequenced the OR repertoire in 332 individuals and examined the relationship between genetic variation and 276 olfactory phenotypes, including the perceived intensity and pleasantness of 68 odorants at two concentrations, detection thresholds of three odorants, and general olfactory acuity. -

OR2W1 (Human) Recombinant Protein
OR2W1 (Human) Recombinant Entrez GeneID: 26692 Protein Gene Symbol: OR2W1 Catalog Number: H00026692-G01 Gene Alias: MGC119162, MGC119163, MGC119165, hs6M1-15 Regulation Status: For research use only (RUO) Gene Summary: Olfactory receptors interact with Product Description: Human OR2W1 full-length ORF odorant molecules in the nose, to initiate a neuronal (NP_112165.1) recombinant protein without tag. response that triggers the perception of a smell. The olfactory receptor proteins are members of a large family Sequence: of G-protein-coupled receptors (GPCR) arising from MDQSNYSSLHGFILLGFSNHPKMEMILSGVVAIFYLITL single coding-exon genes. Olfactory receptors share a VGNTAIILASLLDSQLHTPMYFFLRNLSFLDLCFTTSIIP 7-transmembrane domain structure with many QMLVNLWGPDKTISYVGCIIQLYVYMWLGSVECLLLAV neurotransmitter and hormone receptors and are MSYDRFTAICKPLHYFVVMNPHLCLKMIIMIWSISLANS responsible for the recognition and G protein-mediated VVLCTLTLNLPTCGNNILDHFLCELPALVKIACVDTTTV transduction of odorant signals. The olfactory receptor EMSVFALGIIIVLTPLILILISYGYIAKAVLRTKSKASQRKA gene family is the largest in the genome. The MNTCGSHLTVVSMFYGTIIYMYLQPGNRASKDQGKFL nomenclature assigned to the olfactory receptor genes TLFYTVITPSLNPLIYTLRNKDMKDALKKLMRFHHKSTK and proteins for this organism is independent of other IKRNCKS organisms. [provided by RefSeq] Host: Wheat Germ (in vitro) Theoretical MW (kDa): 36.1 Applications: AP (See our web site product page for detailed applications information) Protocols: See our web site at http://www.abnova.com/support/protocols.asp or product page for detailed protocols Form: Liquid Preparation Method: in vitro wheat germ expression system with proprietary liposome technology Purification: None Recommend Usage: Heating may cause protein aggregation. Please do not heat this product before electrophoresis. Storage Buffer: 25 mM Tris-HCl of pH8.0 containing 2% glycerol. Storage Instruction: Store at -80°C. Aliquot to avoid repeated freezing and thawing. Page 1/1 Powered by TCPDF (www.tcpdf.org). -

Lung Organoids and Their Use to Study Cell-Cell Interaction
Curr Pathobiol Rep (2017) 5:223–231 DOI 10.1007/s40139-017-0137-7 ORGANOID CULTURES (M HUCH, SECTION EDITOR) Lung Organoids and Their Use To Study Cell-Cell Interaction Marko Z. Nikolić1 & Emma L. Rawlins1 Published online: 24 April 2017 # The Author(s) 2017. This article is an open access publication Abstract types which self-organise through cell sorting and spatially Purpose of Review The lung research field has pioneered the restricted lineage commitment in a manner reminiscent of use of organoids for the study of cell-cell interactions. the native organ with some degree of organ functionality [1, Recent Findings The use of organoids for airway basal cells is 2]. Organoids have also been referred to as “mini-organs” and routine. However, the development of organoids for the other enable in vitro modelling of organ development, disease regions of the lung is still in its infancy. Such cultures usually modelling and drug screening. The 3D culture preserves na- rely on cell-cell interactions between the stem cells and a tive DNA integrity and prevents the cells from being trans- putative niche cell for their growth and differentiation. formed [13]. Organoids were first successfully derived from Summary The use of co-culture organoid systems has facili- mouse small intestine using single Lgr5+ stem cells [3]. These tated the in vitro cultivation of previously inaccessible stem organoids were entirely epithelial illustrating that organoids cell populations, providing a novel method for dissecting the can be built without a non-epithelial cellular niche. The molecular requirements of these cell-cell interactions. Future organoid was structured as crypt-villus units, with a similar technology development will allow the growth of epithelial- stem cell hierarchy to in vivo, showing epithelial cell interac- only organoids in more defined media and also the introduc- tions are sufficient for the creation of crypt-villus units. -

Targeted Exome Sequencing Provided Comprehensive Genetic Diagnosis of Congenital Anomalies of the Kidney and Urinary Tract
Journal of Clinical Medicine Article Targeted Exome Sequencing Provided Comprehensive Genetic Diagnosis of Congenital Anomalies of the Kidney and Urinary Tract 1,2, 3,4, 3 1,5 Yo Han Ahn y, Chung Lee y, Nayoung K. D. Kim , Eujin Park , Hee Gyung Kang 1,2,6,* , Il-Soo Ha 1,2,6, Woong-Yang Park 3,4,7 and Hae Il Cheong 1,2,6 1 Department of Pediatrics, Seoul National University College of Medicine, Seoul 03080, Korea; [email protected] (Y.H.A.); [email protected] (E.P.); [email protected] (I.-S.H.); [email protected] (H.I.C.) 2 Department of Pediatrics, Seoul National University Children’s Hospital, Seoul 03080, Korea 3 Samsung Genome Institute, Samsung Medical Center, Seoul 06351, Korea; [email protected] (C.L.); [email protected] (N.K.D.K.); [email protected] (W.-Y.P.) 4 Department of Health Sciences and Technology, Samsung Advanced Institute for Health Sciences and Technology, Sungkyunkwan University, Seoul 06351, Korea 5 Department of Pediatrics, Kangnam Sacred Heart Hospital, Hallym University College of Medicine, Seoul 07441, Korea 6 Kidney Research Institute, Medical Research Center, Seoul National University College of Medicine, Seoul 03080, Korea 7 Department of Molecular Cell Biology, Sungkyunkwan University School of Medicine, Suwon 16419, Korea * Correspondence: [email protected] These authors equally contributed to this article. y Received: 31 January 2020; Accepted: 8 March 2020; Published: 10 March 2020 Abstract: Congenital anomalies of the kidney and urinary tract (CAKUT) are the most common cause of chronic kidney disease in children. -

Systematic Review of Drug Effects in Humans and Models with Surfactant-Processing Disease
REVIEW DRUG EFFECTS Systematic review of drug effects in humans and models with surfactant-processing disease Dymph Klay1, Thijs W. Hoffman1, Ankie M. Harmsze2, Jan C. Grutters1,3 and Coline H.M. van Moorsel1,3 Affiliations: 1Interstitial Lung Disease Center of Excellence, Dept of Pulmonology, St Antonius Hospital, Nieuwegein, The Netherlands. 2Dept of Clinical Pharmacy, St Antonius Hospital, Nieuwegein, The Netherlands. 3Division of Heart and Lung, University Medical Center Utrecht, Utrecht, The Netherlands. Correspondence: Coline H.M. van Moorsel, Interstitial Lung Disease Center of Excellence, St Antonius Hospital, Koekoekslaan 1, Nieuwegein, 3435CM, The Netherlands. E-mail: [email protected] @ERSpublications Drug effects in disease models of surfactant-processing disease are highly dependent on mutation http://ow.ly/ZYZH30k3RkK Cite this article as: Klay D, Hoffman TW, Harmsze AM, et al. Systematic review of drug effects in humans and models with surfactant-processing disease. Eur Respir Rev 2018; 27: 170135 [https://doi.org/10.1183/ 16000617.0135-2017]. ABSTRACT Fibrotic interstitial pneumonias are a group of rare diseases characterised by distortion of lung interstitium. Patients with mutations in surfactant-processing genes, such as surfactant protein C (SFTPC), surfactant protein A1 and A2 (SFTPA1 and A2), ATP binding cassette A3 (ABCA3) and Hermansky–Pudlak syndrome (HPS1, 2 and 4), develop progressive pulmonary fibrosis, often culminating in fatal respiratory insufficiency. Although many mutations have been described, little is known about the optimal treatment strategy for fibrotic interstitial pneumonia patients with surfactant-processing mutations. We performed a systematic literature review of studies that described a drug effect in patients, cell or mouse models with a surfactant-processing mutation. -

University of Groningen Developmental and Pathological Roles of BMP/Follistatin-Like 1 in the Lung Tania, Navessa
University of Groningen Developmental and pathological roles of BMP/follistatin-like 1 in the lung Tania, Navessa IMPORTANT NOTE: You are advised to consult the publisher's version (publisher's PDF) if you wish to cite from it. Please check the document version below. Document Version Publisher's PDF, also known as Version of record Publication date: 2017 Link to publication in University of Groningen/UMCG research database Citation for published version (APA): Tania, N. (2017). Developmental and pathological roles of BMP/follistatin-like 1 in the lung. University of Groningen. Copyright Other than for strictly personal use, it is not permitted to download or to forward/distribute the text or part of it without the consent of the author(s) and/or copyright holder(s), unless the work is under an open content license (like Creative Commons). The publication may also be distributed here under the terms of Article 25fa of the Dutch Copyright Act, indicated by the “Taverne” license. More information can be found on the University of Groningen website: https://www.rug.nl/library/open-access/self-archiving-pure/taverne- amendment. Take-down policy If you believe that this document breaches copyright please contact us providing details, and we will remove access to the work immediately and investigate your claim. Downloaded from the University of Groningen/UMCG research database (Pure): http://www.rug.nl/research/portal. For technical reasons the number of authors shown on this cover page is limited to 10 maximum. Download date: 01-10-2021 CHAPTER 7 1 Variant club cell differentiation is driven by bone morphogenetic protein 4 in adult human airway epithelium: Implications for goblet cell metaplasia and basal cell hyperplasia in COPD Navessa P. -

Misexpression of Cancer/Testis (Ct) Genes in Tumor Cells and the Potential Role of Dream Complex and the Retinoblastoma Protein Rb in Soma-To-Germline Transformation
Michigan Technological University Digital Commons @ Michigan Tech Dissertations, Master's Theses and Master's Reports 2019 MISEXPRESSION OF CANCER/TESTIS (CT) GENES IN TUMOR CELLS AND THE POTENTIAL ROLE OF DREAM COMPLEX AND THE RETINOBLASTOMA PROTEIN RB IN SOMA-TO-GERMLINE TRANSFORMATION SABHA M. ALHEWAT Michigan Technological University, [email protected] Copyright 2019 SABHA M. ALHEWAT Recommended Citation ALHEWAT, SABHA M., "MISEXPRESSION OF CANCER/TESTIS (CT) GENES IN TUMOR CELLS AND THE POTENTIAL ROLE OF DREAM COMPLEX AND THE RETINOBLASTOMA PROTEIN RB IN SOMA-TO- GERMLINE TRANSFORMATION", Open Access Master's Thesis, Michigan Technological University, 2019. https://doi.org/10.37099/mtu.dc.etdr/933 Follow this and additional works at: https://digitalcommons.mtu.edu/etdr Part of the Cancer Biology Commons, and the Cell Biology Commons MISEXPRESSION OF CANCER/TESTIS (CT) GENES IN TUMOR CELLS AND THE POTENTIAL ROLE OF DREAM COMPLEX AND THE RETINOBLASTOMA PROTEIN RB IN SOMA-TO-GERMLINE TRANSFORMATION By Sabha Salem Alhewati A THESIS Submitted in partial fulfillment of the requirements for the degree of MASTER OF SCIENCE In Biological Sciences MICHIGAN TECHNOLOGICAL UNIVERSITY 2019 © 2019 Sabha Alhewati This thesis has been approved in partial fulfillment of the requirements for the Degree of MASTER OF SCIENCE in Biological Sciences. Department of Biological Sciences Thesis Advisor: Paul Goetsch. Committee Member: Ebenezer Tumban. Committee Member: Zhiying Shan. Department Chair: Chandrashekhar Joshi. Table of Contents List of figures .......................................................................................................................v -

Supplementary Table 1
Supplementary Table 1. 492 genes are unique to 0 h post-heat timepoint. The name, p-value, fold change, location and family of each gene are indicated. Genes were filtered for an absolute value log2 ration 1.5 and a significance value of p ≤ 0.05. Symbol p-value Log Gene Name Location Family Ratio ABCA13 1.87E-02 3.292 ATP-binding cassette, sub-family unknown transporter A (ABC1), member 13 ABCB1 1.93E-02 −1.819 ATP-binding cassette, sub-family Plasma transporter B (MDR/TAP), member 1 Membrane ABCC3 2.83E-02 2.016 ATP-binding cassette, sub-family Plasma transporter C (CFTR/MRP), member 3 Membrane ABHD6 7.79E-03 −2.717 abhydrolase domain containing 6 Cytoplasm enzyme ACAT1 4.10E-02 3.009 acetyl-CoA acetyltransferase 1 Cytoplasm enzyme ACBD4 2.66E-03 1.722 acyl-CoA binding domain unknown other containing 4 ACSL5 1.86E-02 −2.876 acyl-CoA synthetase long-chain Cytoplasm enzyme family member 5 ADAM23 3.33E-02 −3.008 ADAM metallopeptidase domain Plasma peptidase 23 Membrane ADAM29 5.58E-03 3.463 ADAM metallopeptidase domain Plasma peptidase 29 Membrane ADAMTS17 2.67E-04 3.051 ADAM metallopeptidase with Extracellular other thrombospondin type 1 motif, 17 Space ADCYAP1R1 1.20E-02 1.848 adenylate cyclase activating Plasma G-protein polypeptide 1 (pituitary) receptor Membrane coupled type I receptor ADH6 (includes 4.02E-02 −1.845 alcohol dehydrogenase 6 (class Cytoplasm enzyme EG:130) V) AHSA2 1.54E-04 −1.6 AHA1, activator of heat shock unknown other 90kDa protein ATPase homolog 2 (yeast) AK5 3.32E-02 1.658 adenylate kinase 5 Cytoplasm kinase AK7 -

Sex-Specific Transcriptome Differences in Human Adipose
G C A T T A C G G C A T genes Article Sex-Specific Transcriptome Differences in Human Adipose Mesenchymal Stem Cells 1, 2, 3 1,3 Eva Bianconi y, Raffaella Casadei y , Flavia Frabetti , Carlo Ventura , Federica Facchin 1,3,* and Silvia Canaider 1,3 1 National Laboratory of Molecular Biology and Stem Cell Bioengineering of the National Institute of Biostructures and Biosystems (NIBB)—Eldor Lab, at the Innovation Accelerator, CNR, Via Piero Gobetti 101, 40129 Bologna, Italy; [email protected] (E.B.); [email protected] (C.V.); [email protected] (S.C.) 2 Department for Life Quality Studies (QuVi), University of Bologna, Corso D’Augusto 237, 47921 Rimini, Italy; [email protected] 3 Department of Experimental, Diagnostic and Specialty Medicine (DIMES), University of Bologna, Via Massarenti 9, 40138 Bologna, Italy; fl[email protected] * Correspondence: [email protected]; Tel.: +39-051-2094114 These authors contributed equally to this work. y Received: 1 July 2020; Accepted: 6 August 2020; Published: 8 August 2020 Abstract: In humans, sexual dimorphism can manifest in many ways and it is widely studied in several knowledge fields. It is increasing the evidence that also cells differ according to sex, a correlation still little studied and poorly considered when cells are used in scientific research. Specifically, our interest is on the sex-related dimorphism on the human mesenchymal stem cells (hMSCs) transcriptome. A systematic meta-analysis of hMSC microarrays was performed by using the Transcriptome Mapper (TRAM) software. This bioinformatic tool was used to integrate and normalize datasets from multiple sources and allowed us to highlight chromosomal segments and genes differently expressed in hMSCs derived from adipose tissue (hADSCs) of male and female donors. -
Sean Raspet – Molecules
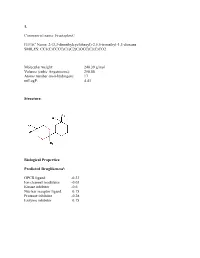
1. Commercial name: Fructaplex© IUPAC Name: 2-(3,3-dimethylcyclohexyl)-2,5,5-trimethyl-1,3-dioxane SMILES: CC1(C)CCCC(C1)C2(C)OCC(C)(C)CO2 Molecular weight: 240.39 g/mol Volume (cubic Angstroems): 258.88 Atoms number (non-hydrogen): 17 miLogP: 4.43 Structure: Biological Properties: Predicted Druglikenessi: GPCR ligand -0.23 Ion channel modulator -0.03 Kinase inhibitor -0.6 Nuclear receptor ligand 0.15 Protease inhibitor -0.28 Enzyme inhibitor 0.15 Commercial name: Fructaplex© IUPAC Name: 2-(3,3-dimethylcyclohexyl)-2,5,5-trimethyl-1,3-dioxane SMILES: CC1(C)CCCC(C1)C2(C)OCC(C)(C)CO2 Predicted Olfactory Receptor Activityii: OR2L13 83.715% OR1G1 82.761% OR10J5 80.569% OR2W1 78.180% OR7A2 77.696% 2. Commercial name: Sylvoxime© IUPAC Name: N-[4-(1-ethoxyethenyl)-3,3,5,5tetramethylcyclohexylidene]hydroxylamine SMILES: CCOC(=C)C1C(C)(C)CC(CC1(C)C)=NO Molecular weight: 239.36 Volume (cubic Angstroems): 252.83 Atoms number (non-hydrogen): 17 miLogP: 4.33 Structure: Biological Properties: Predicted Druglikeness: GPCR ligand -0.6 Ion channel modulator -0.41 Kinase inhibitor -0.93 Nuclear receptor ligand -0.17 Protease inhibitor -0.39 Enzyme inhibitor 0.01 Commercial name: Sylvoxime© IUPAC Name: N-[4-(1-ethoxyethenyl)-3,3,5,5tetramethylcyclohexylidene]hydroxylamine SMILES: CCOC(=C)C1C(C)(C)CC(CC1(C)C)=NO Predicted Olfactory Receptor Activity: OR52D1 71.900% OR1G1 70.394% 0R52I2 70.392% OR52I1 70.390% OR2Y1 70.378% 3. Commercial name: Hyperflor© IUPAC Name: 2-benzyl-1,3-dioxan-5-one SMILES: O=C1COC(CC2=CC=CC=C2)OC1 Molecular weight: 192.21 g/mol Volume -

Genetic Characterization of Greek Population Isolates Reveals Strong Genetic Drift at Missense and Trait-Associated Variants
ARTICLE Received 22 Apr 2014 | Accepted 22 Sep 2014 | Published 6 Nov 2014 DOI: 10.1038/ncomms6345 OPEN Genetic characterization of Greek population isolates reveals strong genetic drift at missense and trait-associated variants Kalliope Panoutsopoulou1,*, Konstantinos Hatzikotoulas1,*, Dionysia Kiara Xifara2,3, Vincenza Colonna4, Aliki-Eleni Farmaki5, Graham R.S. Ritchie1,6, Lorraine Southam1,2, Arthur Gilly1, Ioanna Tachmazidou1, Segun Fatumo1,7,8, Angela Matchan1, Nigel W. Rayner1,2,9, Ioanna Ntalla5,10, Massimo Mezzavilla1,11, Yuan Chen1, Chrysoula Kiagiadaki12, Eleni Zengini13,14, Vasiliki Mamakou13,15, Antonis Athanasiadis16, Margarita Giannakopoulou17, Vassiliki-Eirini Kariakli5, Rebecca N. Nsubuga18, Alex Karabarinde18, Manjinder Sandhu1,8, Gil McVean2, Chris Tyler-Smith1, Emmanouil Tsafantakis12, Maria Karaleftheri16, Yali Xue1, George Dedoussis5 & Eleftheria Zeggini1 Isolated populations are emerging as a powerful study design in the search for low-frequency and rare variant associations with complex phenotypes. Here we genotype 2,296 samples from two isolated Greek populations, the Pomak villages (HELIC-Pomak) in the North of Greece and the Mylopotamos villages (HELIC-MANOLIS) in Crete. We compare their genomic characteristics to the general Greek population and establish them as genetic isolates. In the MANOLIS cohort, we observe an enrichment of missense variants among the variants that have drifted up in frequency by more than fivefold. In the Pomak cohort, we find novel associations at variants on chr11p15.4 showing large allele frequency increases (from 0.2% in the general Greek population to 4.6% in the isolate) with haematological traits, for example, with mean corpuscular volume (rs7116019, P ¼ 2.3 Â 10 À 26). We replicate this association in a second set of Pomak samples (combined P ¼ 2.0 Â 10 À 36). -

The Regulation of Self-Renewal in Normal Human Urothelial Cells
The Regulation of Self-Renewal in Normal Human Urothelial Cells Lisa A. Kirkwood PhD University of York Department of Biology April 2012 Abstract The urinary tract is lined by a mitotically-quiescent, but highly regenerative epithelium, the urothelium. The mechanisms regulating urothelial regeneration are incompletely understood although autocrine stimulation of the Epidermal Growth Factor Receptor (EGFR) signalling pathway has been implicated. The hypothesis developed in this thesis is that urothelial homeostasis is regulated through resolution of interactive signal transduction networks downstream of local environmental cues, such as cell:cell contact. Here, canonical Wnt signalling was examined as a candidate key pathway due to the pivotal role of β-catenin in both nuclear transcription and intercellular adherens junctions. Normal human urothelial (NHU) cells isolated from surgical biopsies were grown as finite cell lines in monolayer culture. mRNA analysis from proliferating cultures inferred all components for a functional autocrine-activated canonical Wnt cascade were present. In proliferating cells, β-catenin was nuclear and Axin2 expression provided an objective hallmark of β-catenin/TCF transcription factor activity. This endogenous activity was not mediated by Wnt receptor activation, as Wnt ligand was produced in inactive (non-palmitylated) form in serum-free culture, but instead -catenin activation was driven via EGFR- mediated phosphorylation of GSK3 and inhibition of the β-catenin destruction complex. In quiescent, contact–inhibited cultures, β-catenin was seen to re- localise to the adherens junctions and GSK3β activity was re-established. Knock-down of β-catenin using RNA interference led to significant changes in p-ERK and p-AKT activity as well as an increase in E-cadherin protein expression.